0001179929false2021FYP3YP5YP3YP5Yhttp://fasb.org/us-gaap/2021-01-31#OtherAssetsNoncurrenthttp://fasb.org/us-gaap/2021-01-31#OtherAssetsNoncurrenthttp://fasb.org/us-gaap/2021-01-31#AccountsPayableAndAccruedLiabilitiesCurrenthttp://fasb.org/us-gaap/2021-01-31#AccountsPayableAndAccruedLiabilitiesCurrenthttp://fasb.org/us-gaap/2021-01-31#OtherLiabilitiesNoncurrenthttp://fasb.org/us-gaap/2021-01-31#OtherLiabilitiesNoncurrenthttp://fasb.org/us-gaap/2021-01-31#AccountsPayableAndAccruedLiabilitiesCurrenthttp://fasb.org/us-gaap/2021-01-31#AccountsPayableAndAccruedLiabilitiesCurrent00011799292021-01-012021-12-3100011799292021-06-30iso4217:USD00011799292022-02-11xbrli:shares00011799292020-01-012020-12-3100011799292019-01-012019-12-31iso4217:USDxbrli:shares00011799292021-12-3100011799292020-12-310001179929srt:ParentCompanyMember2021-12-310001179929srt:ParentCompanyMember2020-12-310001179929us-gaap:CommonStockMember2018-12-310001179929us-gaap:AdditionalPaidInCapitalMember2018-12-310001179929us-gaap:AccumulatedOtherComprehensiveIncomeMember2018-12-310001179929us-gaap:RetainedEarningsMember2018-12-3100011799292018-12-310001179929us-gaap:RetainedEarningsMember2019-01-012019-12-310001179929us-gaap:AdditionalPaidInCapitalMember2019-01-012019-12-310001179929srt:CumulativeEffectPeriodOfAdoptionAdjustmentMemberus-gaap:AccumulatedOtherComprehensiveIncomeMember2018-12-310001179929srt:CumulativeEffectPeriodOfAdoptionAdjustmentMemberus-gaap:RetainedEarningsMember2018-12-310001179929srt:CumulativeEffectPeriodOfAdoptionAdjustmentMember2018-12-310001179929us-gaap:AccumulatedOtherComprehensiveIncomeMember2019-01-012019-12-310001179929us-gaap:CommonStockMember2019-12-310001179929us-gaap:AdditionalPaidInCapitalMember2019-12-310001179929us-gaap:AccumulatedOtherComprehensiveIncomeMember2019-12-310001179929us-gaap:RetainedEarningsMember2019-12-3100011799292019-12-310001179929us-gaap:RetainedEarningsMember2020-01-012020-12-310001179929us-gaap:CommonStockMember2020-01-012020-12-310001179929us-gaap:AdditionalPaidInCapitalMember2020-01-012020-12-310001179929us-gaap:AccumulatedOtherComprehensiveIncomeMember2020-01-012020-12-310001179929us-gaap:CommonStockMember2020-12-310001179929us-gaap:AdditionalPaidInCapitalMember2020-12-310001179929us-gaap:AccumulatedOtherComprehensiveIncomeMember2020-12-310001179929us-gaap:RetainedEarningsMember2020-12-310001179929us-gaap:RetainedEarningsMember2021-01-012021-12-310001179929us-gaap:CommonStockMember2021-01-012021-12-310001179929us-gaap:AdditionalPaidInCapitalMember2021-01-012021-12-310001179929us-gaap:AccumulatedOtherComprehensiveIncomeMember2021-01-012021-12-310001179929us-gaap:CommonStockMember2021-12-310001179929us-gaap:AdditionalPaidInCapitalMember2021-12-310001179929us-gaap:AccumulatedOtherComprehensiveIncomeMember2021-12-310001179929us-gaap:RetainedEarningsMember2021-12-310001179929moh:HealthPlansMember2021-12-31moh:membermoh:position0001179929moh:HealthPlansMembersrt:MinimumMember2021-01-012021-12-310001179929moh:HealthPlansMembersrt:MaximumMember2021-01-012021-12-310001179929moh:HealthPlansMemberstpr:NY2021-10-250001179929stpr:NYmoh:AgeWellNewYorkMembermoh:NewYorkAcquisitionMedicaidMember2021-08-31moh:security0001179929stpr:NYmoh:AgeWellNewYorkMembermoh:NewYorkAcquisitionMedicaidMember2020-01-012020-12-310001179929moh:NewYorkAcquisitionMedicaidMember2021-10-072021-10-0700011799292021-09-012021-09-300001179929moh:GovernmentReceivablesMember2021-12-310001179929moh:GovernmentReceivablesMember2020-12-310001179929moh:PharmacyRebateReceivablesMember2021-12-310001179929moh:PharmacyRebateReceivablesMember2020-12-310001179929moh:HealthInsurerFeeReimbursementReceivablesMember2021-12-310001179929moh:HealthInsurerFeeReimbursementReceivablesMember2020-12-310001179929moh:OtherReceivablesMember2021-12-310001179929moh:OtherReceivablesMember2020-12-310001179929moh:CompleteCareReceivablesMember2021-12-310001179929moh:CompleteCareReceivablesMember2020-12-310001179929us-gaap:FairValueInputsLevel3Member2021-12-310001179929srt:MinimumMember2021-01-012021-12-310001179929srt:MaximumMember2021-01-012021-12-310001179929moh:COVID19Member2021-01-012021-12-310001179929moh:MMPPlansMember2020-01-012020-12-310001179929moh:COVID19Member2020-01-012020-12-310001179929us-gaap:HealthCarePremiumMembersrt:MinimumMember2021-01-012021-12-31xbrli:pure0001179929us-gaap:HealthCarePremiumMembersrt:MaximumMember2021-01-012021-12-310001179929stpr:CAmoh:HealthPlansMember2021-01-012021-12-310001179929stpr:CAmoh:HealthPlansMember2020-01-012020-12-310001179929stpr:CAmoh:HealthPlansMember2019-01-012019-12-310001179929stpr:FLmoh:HealthPlansMember2021-01-012021-12-310001179929stpr:FLmoh:HealthPlansMember2020-01-012020-12-310001179929stpr:FLmoh:HealthPlansMember2019-01-012019-12-310001179929moh:HealthPlansMemberstpr:IL2021-01-012021-12-310001179929moh:HealthPlansMemberstpr:IL2020-01-012020-12-310001179929moh:HealthPlansMemberstpr:IL2019-01-012019-12-310001179929moh:HealthPlansMemberstpr:KY2021-01-012021-12-310001179929moh:HealthPlansMemberstpr:KY2020-01-012020-12-310001179929moh:HealthPlansMemberstpr:KY2019-01-012019-12-310001179929moh:HealthPlansMemberstpr:MI2021-01-012021-12-310001179929moh:HealthPlansMemberstpr:MI2020-01-012020-12-310001179929moh:HealthPlansMemberstpr:MI2019-01-012019-12-310001179929moh:HealthPlansMemberstpr:NY2021-01-012021-12-310001179929moh:HealthPlansMemberstpr:NY2020-01-012020-12-310001179929moh:HealthPlansMemberstpr:NY2019-01-012019-12-310001179929stpr:OHmoh:HealthPlansMember2021-01-012021-12-310001179929stpr:OHmoh:HealthPlansMember2020-01-012020-12-310001179929stpr:OHmoh:HealthPlansMember2019-01-012019-12-310001179929moh:HealthPlansMemberstpr:TX2021-01-012021-12-310001179929moh:HealthPlansMemberstpr:TX2020-01-012020-12-310001179929moh:HealthPlansMemberstpr:TX2019-01-012019-12-310001179929stpr:WAmoh:HealthPlansMember2021-01-012021-12-310001179929stpr:WAmoh:HealthPlansMember2020-01-012020-12-310001179929stpr:WAmoh:HealthPlansMember2019-01-012019-12-310001179929moh:HealthPlansMembermoh:OtherGeographicalAreasMember2021-01-012021-12-310001179929moh:HealthPlansMembermoh:OtherGeographicalAreasMember2020-01-012020-12-310001179929moh:HealthPlansMembermoh:OtherGeographicalAreasMember2019-01-012019-12-310001179929moh:HealthPlansMember2021-01-012021-12-310001179929moh:HealthPlansMember2020-01-012020-12-310001179929moh:HealthPlansMember2019-01-012019-12-3100011799292021-10-012021-12-31moh:business_combination0001179929moh:HealthPlansSegmentMember2021-10-250001179929us-gaap:ContractualRightsMember2021-12-310001179929us-gaap:ContractualRightsMember2021-01-012021-12-310001179929moh:ProviderNetworkMember2021-12-310001179929moh:ProviderNetworkMember2021-01-012021-12-310001179929us-gaap:TradeNamesMember2021-12-310001179929us-gaap:TradeNamesMember2021-01-012021-12-310001179929moh:MagellanCompleteCareMember2020-12-310001179929moh:MagellanCompleteCareMember2020-12-012020-12-310001179929moh:MagellanCompleteCareMember2021-10-012021-12-310001179929moh:MagellanCompleteCareMember2021-01-012021-12-310001179929us-gaap:CorporateDebtSecuritiesMember2021-12-310001179929us-gaap:CorporateDebtSecuritiesMemberus-gaap:FairValueInputsLevel1Member2021-12-310001179929us-gaap:FairValueInputsLevel2Memberus-gaap:CorporateDebtSecuritiesMember2021-12-310001179929us-gaap:CorporateDebtSecuritiesMemberus-gaap:FairValueInputsLevel3Member2021-12-310001179929us-gaap:CommercialMortgageBackedSecuritiesMember2021-12-310001179929us-gaap:CommercialMortgageBackedSecuritiesMemberus-gaap:FairValueInputsLevel1Member2021-12-310001179929us-gaap:FairValueInputsLevel2Memberus-gaap:CommercialMortgageBackedSecuritiesMember2021-12-310001179929us-gaap:CommercialMortgageBackedSecuritiesMemberus-gaap:FairValueInputsLevel3Member2021-12-310001179929us-gaap:USTreasuryNotesSecuritiesMember2021-12-310001179929us-gaap:USTreasuryNotesSecuritiesMemberus-gaap:FairValueInputsLevel1Member2021-12-310001179929us-gaap:FairValueInputsLevel2Memberus-gaap:USTreasuryNotesSecuritiesMember2021-12-310001179929us-gaap:USTreasuryNotesSecuritiesMemberus-gaap:FairValueInputsLevel3Member2021-12-310001179929us-gaap:AssetBackedSecuritiesMember2021-12-310001179929us-gaap:FairValueInputsLevel1Memberus-gaap:AssetBackedSecuritiesMember2021-12-310001179929us-gaap:FairValueInputsLevel2Memberus-gaap:AssetBackedSecuritiesMember2021-12-310001179929us-gaap:FairValueInputsLevel3Memberus-gaap:AssetBackedSecuritiesMember2021-12-310001179929moh:MunicipalSecuritiesMember2021-12-310001179929moh:MunicipalSecuritiesMemberus-gaap:FairValueInputsLevel1Member2021-12-310001179929us-gaap:FairValueInputsLevel2Membermoh:MunicipalSecuritiesMember2021-12-310001179929moh:MunicipalSecuritiesMemberus-gaap:FairValueInputsLevel3Member2021-12-310001179929moh:OtherSecuritiesMember2021-12-310001179929moh:OtherSecuritiesMemberus-gaap:FairValueInputsLevel1Member2021-12-310001179929us-gaap:FairValueInputsLevel2Membermoh:OtherSecuritiesMember2021-12-310001179929moh:OtherSecuritiesMemberus-gaap:FairValueInputsLevel3Member2021-12-310001179929us-gaap:FairValueInputsLevel1Member2021-12-310001179929us-gaap:FairValueInputsLevel2Member2021-12-310001179929us-gaap:CorporateDebtSecuritiesMember2020-12-310001179929us-gaap:CorporateDebtSecuritiesMemberus-gaap:FairValueInputsLevel1Member2020-12-310001179929us-gaap:FairValueInputsLevel2Memberus-gaap:CorporateDebtSecuritiesMember2020-12-310001179929us-gaap:CorporateDebtSecuritiesMemberus-gaap:FairValueInputsLevel3Member2020-12-310001179929us-gaap:CommercialMortgageBackedSecuritiesMember2020-12-310001179929us-gaap:CommercialMortgageBackedSecuritiesMemberus-gaap:FairValueInputsLevel1Member2020-12-310001179929us-gaap:FairValueInputsLevel2Memberus-gaap:CommercialMortgageBackedSecuritiesMember2020-12-310001179929us-gaap:CommercialMortgageBackedSecuritiesMemberus-gaap:FairValueInputsLevel3Member2020-12-310001179929us-gaap:USTreasuryNotesSecuritiesMember2020-12-310001179929us-gaap:USTreasuryNotesSecuritiesMemberus-gaap:FairValueInputsLevel1Member2020-12-310001179929us-gaap:FairValueInputsLevel2Memberus-gaap:USTreasuryNotesSecuritiesMember2020-12-310001179929us-gaap:USTreasuryNotesSecuritiesMemberus-gaap:FairValueInputsLevel3Member2020-12-310001179929us-gaap:AssetBackedSecuritiesMember2020-12-310001179929us-gaap:FairValueInputsLevel1Memberus-gaap:AssetBackedSecuritiesMember2020-12-310001179929us-gaap:FairValueInputsLevel2Memberus-gaap:AssetBackedSecuritiesMember2020-12-310001179929us-gaap:FairValueInputsLevel3Memberus-gaap:AssetBackedSecuritiesMember2020-12-310001179929moh:MunicipalSecuritiesMember2020-12-310001179929moh:MunicipalSecuritiesMemberus-gaap:FairValueInputsLevel1Member2020-12-310001179929us-gaap:FairValueInputsLevel2Membermoh:MunicipalSecuritiesMember2020-12-310001179929moh:MunicipalSecuritiesMemberus-gaap:FairValueInputsLevel3Member2020-12-310001179929us-gaap:FairValueInputsLevel1Member2020-12-310001179929us-gaap:FairValueInputsLevel2Member2020-12-310001179929us-gaap:FairValueInputsLevel3Member2020-12-310001179929moh:PassportHealthPlanIncMember2021-12-310001179929moh:PassportHealthPlanIncMemberus-gaap:SubsequentEventMember2022-01-012022-01-310001179929us-gaap:SeniorNotesMembermoh:A5375SeniorNotesMember2021-12-310001179929us-gaap:CarryingReportedAmountFairValueDisclosureMemberus-gaap:SeniorNotesMembermoh:A5375SeniorNotesMember2021-12-310001179929us-gaap:EstimateOfFairValueFairValueDisclosureMemberus-gaap:SeniorNotesMembermoh:A5375SeniorNotesMember2021-12-310001179929us-gaap:CarryingReportedAmountFairValueDisclosureMemberus-gaap:SeniorNotesMembermoh:A5375SeniorNotesMember2020-12-310001179929us-gaap:EstimateOfFairValueFairValueDisclosureMemberus-gaap:SeniorNotesMembermoh:A5375SeniorNotesMember2020-12-310001179929us-gaap:SeniorNotesMembermoh:A4375SeniorNotesMember2021-12-310001179929us-gaap:CarryingReportedAmountFairValueDisclosureMemberus-gaap:SeniorNotesMembermoh:A4375SeniorNotesMember2021-12-310001179929us-gaap:EstimateOfFairValueFairValueDisclosureMemberus-gaap:SeniorNotesMembermoh:A4375SeniorNotesMember2021-12-310001179929us-gaap:CarryingReportedAmountFairValueDisclosureMemberus-gaap:SeniorNotesMembermoh:A4375SeniorNotesMember2020-12-310001179929us-gaap:EstimateOfFairValueFairValueDisclosureMemberus-gaap:SeniorNotesMembermoh:A4375SeniorNotesMember2020-12-310001179929us-gaap:SeniorNotesMembermoh:ThreePointEightSevenFivePercentSeniorNotesMember2021-12-310001179929us-gaap:CarryingReportedAmountFairValueDisclosureMemberus-gaap:SeniorNotesMembermoh:ThreePointEightSevenFivePercentSeniorNotesMember2021-12-310001179929us-gaap:EstimateOfFairValueFairValueDisclosureMemberus-gaap:SeniorNotesMembermoh:ThreePointEightSevenFivePercentSeniorNotesMember2021-12-310001179929us-gaap:CarryingReportedAmountFairValueDisclosureMemberus-gaap:SeniorNotesMembermoh:ThreePointEightSevenFivePercentSeniorNotesMember2020-12-310001179929us-gaap:EstimateOfFairValueFairValueDisclosureMemberus-gaap:SeniorNotesMembermoh:ThreePointEightSevenFivePercentSeniorNotesMember2020-12-310001179929moh:A3875SeniorNotesMemberus-gaap:SeniorNotesMember2021-12-310001179929moh:A3875SeniorNotesMemberus-gaap:CarryingReportedAmountFairValueDisclosureMemberus-gaap:SeniorNotesMember2021-12-310001179929moh:A3875SeniorNotesMemberus-gaap:EstimateOfFairValueFairValueDisclosureMemberus-gaap:SeniorNotesMember2021-12-310001179929moh:A3875SeniorNotesMemberus-gaap:CarryingReportedAmountFairValueDisclosureMemberus-gaap:SeniorNotesMember2020-12-310001179929moh:A3875SeniorNotesMemberus-gaap:EstimateOfFairValueFairValueDisclosureMemberus-gaap:SeniorNotesMember2020-12-310001179929us-gaap:CarryingReportedAmountFairValueDisclosureMember2021-12-310001179929us-gaap:EstimateOfFairValueFairValueDisclosureMember2021-12-310001179929us-gaap:CarryingReportedAmountFairValueDisclosureMember2020-12-310001179929us-gaap:EstimateOfFairValueFairValueDisclosureMember2020-12-310001179929us-gaap:MortgageBackedSecuritiesMember2021-12-310001179929us-gaap:MortgageBackedSecuritiesMember2020-12-310001179929us-gaap:CashAndCashEquivalentsMember2021-12-310001179929us-gaap:CashAndCashEquivalentsMember2020-12-310001179929moh:CompleteCareMember2021-12-310001179929moh:CompleteCareMember2020-12-310001179929us-gaap:FurnitureAndFixturesMembersrt:MinimumMember2021-01-012021-12-310001179929us-gaap:FurnitureAndFixturesMembersrt:MaximumMember2021-01-012021-12-310001179929us-gaap:ComputerSoftwareIntangibleAssetMember2021-01-012021-12-310001179929srt:MinimumMemberus-gaap:LeaseholdImprovementsMember2021-01-012021-12-310001179929us-gaap:LeaseholdImprovementsMembersrt:MaximumMember2021-01-012021-12-310001179929us-gaap:BuildingAndBuildingImprovementsMembersrt:MinimumMember2021-01-012021-12-310001179929us-gaap:BuildingAndBuildingImprovementsMembersrt:MaximumMember2021-01-012021-12-310001179929us-gaap:SoftwareAndSoftwareDevelopmentCostsMember2021-12-310001179929us-gaap:SoftwareAndSoftwareDevelopmentCostsMember2020-12-310001179929us-gaap:FurnitureAndFixturesMember2021-12-310001179929us-gaap:FurnitureAndFixturesMember2020-12-310001179929us-gaap:BuildingAndBuildingImprovementsMember2021-12-310001179929us-gaap:BuildingAndBuildingImprovementsMember2020-12-310001179929us-gaap:LandMember2021-12-310001179929us-gaap:LandMember2020-12-310001179929us-gaap:PropertyPlantAndEquipmentMember2021-12-310001179929us-gaap:PropertyPlantAndEquipmentMember2020-12-310001179929moh:CompleteCareMember2021-12-310001179929moh:CompleteCareMember2020-12-310001179929moh:MedicaidMember2019-12-310001179929moh:MedicareMember2019-12-310001179929moh:OtherProgramMember2019-12-310001179929moh:MedicaidMember2020-01-012020-12-310001179929moh:MedicareMember2020-01-012020-12-310001179929moh:OtherProgramMember2020-01-012020-12-310001179929moh:MedicaidMember2020-12-310001179929moh:MedicareMember2020-12-310001179929moh:OtherProgramMember2020-12-310001179929moh:MedicaidMember2021-01-012021-12-310001179929moh:MedicareMember2021-01-012021-12-310001179929moh:OtherProgramMember2021-01-012021-12-310001179929moh:MedicaidMember2021-12-310001179929moh:MedicareMember2021-12-310001179929moh:OtherProgramMember2021-12-310001179929moh:ContractRightsandLicensingAgreementsMember2021-12-310001179929moh:ContractRightsandLicensingAgreementsMember2020-12-310001179929moh:ProviderNetworksMember2021-12-310001179929moh:ProviderNetworksMember2020-12-310001179929us-gaap:TradeNamesMember2020-12-310001179929moh:CompleteCareMember2019-12-310001179929moh:MarketplaceMember2020-12-310001179929moh:MarketplaceMember2021-01-012021-12-310001179929moh:MarketplaceMember2021-12-310001179929moh:MarketplaceMember2019-12-310001179929moh:MarketplaceMember2020-01-012020-12-310001179929moh:MedicaidMember2018-12-310001179929moh:MedicareMember2018-12-310001179929moh:MarketplaceMember2018-12-310001179929moh:MedicaidMember2019-01-012019-12-310001179929moh:MedicareMember2019-01-012019-12-310001179929moh:MarketplaceMember2019-01-012019-12-310001179929us-gaap:ShortDurationInsuranceContractAccidentYear2019Member2019-01-012019-12-310001179929us-gaap:ShortDurationInsuranceContractAccidentYear2019Member2020-01-012020-12-310001179929us-gaap:ShortDurationInsuranceContractAccidentYear2019Member2021-01-012021-12-310001179929us-gaap:ShortDurationInsuranceContractAccidentYear2019Member2021-12-310001179929us-gaap:ShortDurationInsuranceContractAccidentYear2020Member2020-01-012020-12-310001179929us-gaap:ShortDurationInsuranceContractAccidentYear2020Member2021-01-012021-12-310001179929us-gaap:ShortDurationInsuranceContractAccidentYear2020Member2021-12-310001179929us-gaap:ShortDurationInsuranceContractAccidentYear2021Member2021-01-012021-12-310001179929us-gaap:ShortDurationInsuranceContractAccidentYear2021Member2021-12-310001179929us-gaap:ShortDurationInsuranceContractAccidentYear2019Member2019-12-310001179929us-gaap:ShortDurationInsuranceContractAccidentYear2019Member2020-12-310001179929us-gaap:ShortDurationInsuranceContractAccidentYear2020Member2020-12-310001179929us-gaap:SeniorNotesMembermoh:A5375SeniorNotesMember2020-12-310001179929us-gaap:SeniorNotesMembermoh:A4375SeniorNotesMember2020-12-310001179929us-gaap:SeniorNotesMembermoh:ThreePointEightSevenFivePercentSeniorNotesMember2020-12-310001179929moh:A3875SeniorNotesMemberus-gaap:SeniorNotesMember2020-12-310001179929us-gaap:RevolvingCreditFacilityMemberus-gaap:LineOfCreditMember2021-12-310001179929us-gaap:LineOfCreditMember2021-01-012021-12-310001179929us-gaap:SeniorNotesMember2021-01-012021-12-310001179929us-gaap:SeniorNotesMember2021-12-310001179929moh:A3875SeniorNotesMemberus-gaap:SeniorNotesMember2021-11-160001179929moh:A3875SeniorNotesMemberus-gaap:SeniorNotesMember2021-11-162021-11-160001179929us-gaap:StateAndLocalJurisdictionMember2021-12-310001179929us-gaap:ForeignCountryMember2021-12-310001179929us-gaap:CommonStockMember2021-09-300001179929us-gaap:SubsequentEventMember2021-09-012022-02-140001179929us-gaap:CommonStockMember2021-01-012021-02-110001179929us-gaap:CommonStockMember2020-11-012020-12-3100011799292020-11-012020-12-310001179929us-gaap:CommonStockMemberus-gaap:EmployeeStockMember2021-01-012021-12-310001179929us-gaap:CommonStockMemberus-gaap:EmployeeStockMember2020-01-012020-12-310001179929moh:RestrictedandPerformanceStockMember2021-01-012021-12-310001179929moh:RestrictedandPerformanceStockMember2020-01-012020-12-310001179929moh:RestrictedandPerformanceStockMember2019-01-012019-12-310001179929moh:EmployeeStockPurchasePlanandStockOptionsMember2021-01-012021-12-310001179929moh:EmployeeStockPurchasePlanandStockOptionsMember2020-01-012020-12-310001179929moh:EmployeeStockPurchasePlanandStockOptionsMember2019-01-012019-12-310001179929moh:EquityIncentivePlanMember2020-12-310001179929us-gaap:RestrictedStockMember2021-01-012021-12-310001179929us-gaap:RestrictedStockUnitsRSUMember2021-01-012021-12-310001179929us-gaap:RestrictedStockMember2020-12-310001179929us-gaap:RestrictedStockUnitsRSUMember2020-12-310001179929us-gaap:RestrictedStockMember2021-12-310001179929us-gaap:RestrictedStockUnitsRSUMember2021-12-310001179929us-gaap:PerformanceSharesMember2021-01-012021-12-310001179929srt:MinimumMemberus-gaap:PerformanceSharesMember2021-01-012021-12-310001179929us-gaap:PerformanceSharesMembersrt:MaximumMember2021-01-012021-12-310001179929us-gaap:PerformanceSharesMember2021-12-310001179929us-gaap:RestrictedStockMember2020-01-012020-12-310001179929us-gaap:RestrictedStockMember2019-01-012019-12-310001179929us-gaap:RestrictedStockUnitsRSUMember2020-01-012020-12-310001179929us-gaap:RestrictedStockUnitsRSUMember2019-01-012019-12-310001179929us-gaap:EmployeeStockOptionMember2021-01-012021-12-310001179929us-gaap:EmployeeStockMember2021-01-012021-12-310001179929moh:OtherProgramMember2019-01-012019-12-310001179929us-gaap:OperatingSegmentsMember2021-01-012021-12-310001179929us-gaap:OperatingSegmentsMember2020-01-012020-12-310001179929us-gaap:OperatingSegmentsMember2019-01-012019-12-310001179929us-gaap:MaterialReconcilingItemsMember2021-01-012021-12-310001179929us-gaap:MaterialReconcilingItemsMember2020-01-012020-12-310001179929us-gaap:MaterialReconcilingItemsMember2019-01-012019-12-310001179929srt:ParentCompanyMember2021-01-012021-12-310001179929srt:ParentCompanyMember2020-01-012020-12-310001179929srt:ParentCompanyMember2019-01-012019-12-310001179929srt:ParentCompanyMember2019-12-310001179929srt:ParentCompanyMember2018-12-31
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
Form 10-K
(Mark One)
| | | | | |
| ☒ | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
FOR THE FISCAL YEAR ENDED DECEMBER 31, 2021
or
| | | | | |
| ☐ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
Commission File Number 1-31719
MOLINA HEALTHCARE, INC.
(Exact name of registrant as specified in its charter)
| | | | | | | | |
| Delaware | | 13-4204626 |
| (State or other jurisdiction of | | (I.R.S. Employer |
| incorporation or organization) | | Identification No.) |
200 Oceangate, Suite 100, Long Beach, California 90802
(Address of principal executive offices)
(562) 435-3666
(Registrant’s telephone number, including area code)
Securities registered pursuant to Section 12(b) of the Act:
| | | | | | | | |
| Title of Each Class | Trading Symbol(s) | Name of Each Exchange on Which Registered |
| Common Stock, $0.001 Par Value | MOH | New York Stock Exchange |
Securities registered pursuant to Section 12(g) of the Act:
None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. ☒ Yes ☐ No
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. ☐ Yes ☒ No
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. ☒ Yes ☐ No
Indicate by check mark whether the registrant has submitted electronically every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S-T during the preceding 12 months (or for such shorter period that the registrant was required to submit such files). ☒ Yes ☐ No
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer,” “smaller reporting company,” and “emerging growth company” in Rule 12b-2 of the Exchange Act.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Large accelerated filer | ☒ | Accelerated filer | ☐ | Non-accelerated filer | ☐ | Smaller reporting company | ☐ | Emerging growth company | ☐ |
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ☐
Indicate by check mark whether the registrant has filed a report on and attestation to its management’s assessment of the effectiveness of its internal control over financial reporting under Section 404(b) of the Sarbanes-Oxley Act (15 U.S.C. 7262(b)) by the registered public accounting firm that prepared or issued its audit report. ☒
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act). ☐ Yes ☒ No
The aggregate market value of Common Stock held by non-affiliates of the registrant as of June 30, 2021, the last business day of our most recently completed second fiscal quarter, was approximately $14.7 billion (based upon the closing price for shares of the registrant’s Common Stock as reported by the New York Stock Exchange, Inc. on June 30, 2021).
As of February 11, 2022, approximately 58,400,000 shares of the registrant’s Common Stock, $0.001 par value per share, were outstanding.
DOCUMENTS INCORPORATED BY REFERENCE
Portions of the registrant’s Proxy Statement for the 2022 Annual Meeting of Stockholders to be held on May 4, 2022, are incorporated by reference into Part III of this Form 10-K, to the extent described therein.
MOLINA HEALTHCARE, INC. 2021 FORM 10-K
TABLE OF CONTENTS
| | | | | | | | |
| Page |
| | |
| Part I |
| Item Number | |
| 1. | | |
| | |
| 1A. | | |
| | |
| 1B. | Unresolved Staff Comments | Not Applicable. |
| | |
| 2. | | |
| | |
| 3. | | |
| | |
| 4. | Mine Safety Disclosures | Not Applicable. |
| | |
Part II |
| | |
| 5. | | |
| | |
| 6. | [Reserved] | Not Applicable. |
| | |
| 7. | | |
| | |
| 7A. | | |
| | |
| 8. | | |
| | |
| 9. | Changes in and Disagreements with Accountants on Accounting and Financial Disclosure | Not Applicable. |
| | |
| 9A. | | |
| | |
| 9B. | | |
| | |
| 9C. | Disclosure Regarding Foreign Jurisdictions that Prevent Inspections | Not Applicable. |
| | |
Part III |
| | |
| 10. | | |
| | |
| 11. | | |
| | |
| 12. | | |
| | |
| 13. | | |
| | |
| 14. | | |
| | |
Part IV |
| | |
| 15. | | |
| | |
| 16. | Form 10-K Summary | Not Applicable. |
FORWARD LOOKING STATEMENTS
This Annual Report on Form 10-K (this “Form 10-K”) contains forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995 that involve risks and uncertainties. Many of the forward-looking statements are located under the heading “Management’s Discussion and Analysis of Financial Condition and Results of Operations.” Forward-looking statements provide current expectations of future events based on certain assumptions and include any statement that does not directly relate to any historical or current fact. Forward-looking statements can also be identified by words such as “guidance,” “future,” “anticipates,” “believes,” “estimates,” “expects,” “growth,” “intends,” “plans,” “predicts,” “projects,” “will,” “would,” “could,” “can,” “may,” and similar terms. Readers are cautioned not to place undue reliance on any forward-looking statements, as forward-looking statements are not guarantees of future performance and the Company’s actual results may differ significantly due to numerous known and unknown risks and uncertainties. Those known risks and uncertainties include, but are not limited to, the risk factors identified in the section of this Form 10-K titled “Risk Factors,” as well as the following:
•the impact of the COVID-19 pandemic and its associated or indirect effects on our business, operations, and financial results, including without limitation the duration of the Public Health Emergency Declaration (“PHE”) and associated suspension in redeterminations, and the potential impact on our workforce or contractors of federal or state vaccine mandates;
•significant budget pressures on state governments from diminished tax revenues incidental to the COVID-19 pandemic and their efforts to reduce rates or limit rate increases, to impose profit caps or risk corridors, or to recoup previously paid premium amounts on a retroactive basis;
•the numerous political, judicial, and market-based uncertainties associated with the Affordable Care Act (the “ACA”);
•the market dynamics surrounding the ACA Marketplaces, including issues impacting enrollment, risk adjustment estimates and results, the potential for disproportionate enrollment of higher acuity members, and the discontinuation of premium tax credits;
•the outcome of the legal proceedings in Kentucky with regard to the Medicaid contract award to our Kentucky health plan and our acquisition of certain assets of Passport;
•the success of our efforts to retain existing or awarded government contracts, and the success of any bid submissions in response to requests for proposal, including our contracts in California and Texas;
•subsequent adjustments to reported premium revenue based upon subsequent developments or new information, including changes to estimated amounts payable or receivable related to Marketplace risk adjustment;
•our ability to consummate, integrate, and realize benefits from acquisitions, including the completed acquisitions of Magellan Complete Care, Passport, Affinity, and the Medicaid assets of Cigna in Texas, and the announced acquisition of AgeWell New York;
•effective management of our medical costs;
•our ability to predict with a reasonable degree of accuracy utilization rates, including utilization rates associated with COVID-19;
•cyber-attacks, ransomware attacks, or other privacy or data security incidents resulting in an inadvertent unauthorized disclosure of protected information;
•the ability to manage our operations, including maintaining and creating adequate internal systems and controls relating to authorizations, approvals, provider payments, and the overall success of our care management initiatives;
•our receipt of adequate premium rates to support increasing pharmacy costs, including costs associated with specialty drugs and costs resulting from formulary changes that allow the option of higher-priced non-generic drugs;
•our ability to operate profitably in an environment where the trend in premium rate increases lags behind the trend in increasing medical costs;
•the interpretation and implementation of federal or state medical cost expenditure floors, administrative cost and profit ceilings, premium stabilization programs, profit-sharing arrangements, and risk adjustment provisions and requirements;
•our estimates of amounts owed for such cost expenditure floors, administrative cost and profit ceilings, premium stabilization programs, profit-sharing arrangements, and risk adjustment provisions and requirements;
•the Medicaid expansion medical cost corridor, and any other retroactive adjustment to revenue where methodologies and procedures are subject to interpretation or dependent upon information about the health status of participants other than Molina members;
Molina Healthcare, Inc. 2021 Form 10-K | 1
•the interpretation and implementation of at-risk premium rules and state contract performance requirements regarding the achievement of certain quality measures, and our ability to recognize revenue amounts associated therewith;
•the success and renewal of our duals demonstration programs in California, Illinois, Michigan, Ohio, South Carolina, and Texas;
•the accurate estimation of incurred but not reported or paid medical costs across our health plans;
•efforts by states to recoup previously paid and recognized premium amounts;
•changes in our annual effective tax rate, due to federal and/or state legislation, or changes in our mix of earnings and other factors;
•complications, member confusion, eligibility redeterminations, or enrollment backlogs related to the renewal of Medicaid coverage;
•fraud, waste and abuse matters, government audits or reviews, comment letters, or potential investigations, and any fine, sanction, enrollment freeze, corrective action plan, monitoring program, or premium recovery that may result therefrom;
•our exit from Puerto Rico, including the payment in full of our outstanding accounts receivable, the effective run-out of claims, the return of our capital, and the outcome of the claims filed against our Puerto Rico health plan and us by the Puerto Rico Health Insurance Administration, or ASES;
•changes with respect to our provider contracts and the loss of providers;
•approval by state regulators of dividends and distributions by our health plan subsidiaries;
•changes in funding under our contracts as a result of regulatory changes, programmatic adjustments, or other reforms;
•high dollar claims related to catastrophic illness;
•the resolution, favorable or unfavorable, of litigation, arbitration, or administrative proceedings;
•the relatively small number of states in which we operate health plans, including the greater scale and revenues of our California, Ohio, Texas, and Washington health plans;
•the failure to comply with the financial or other covenants in our credit agreement or the indentures governing our outstanding notes;
•the availability of adequate financing on acceptable terms to fund and capitalize our expansion and growth, repay our outstanding indebtedness at maturity, and meet our general liquidity needs;
•the sufficiency of funds on hand to pay the amounts due upon maturity of our outstanding notes;
•the failure of a state in which we operate to renew its federal Medicaid waiver;
•changes generally affecting the managed care industry;
•increases in government surcharges, taxes, and assessments;
•the unexpected loss of the leadership of one or more of our senior executives; and
•increasing competition and consolidation in the Medicaid industry.
Each of the terms “Molina Healthcare, Inc.” “Molina Healthcare,” “Company,” “we,” “our,” and “us,” as used herein, refers collectively to Molina Healthcare, Inc. and its wholly owned subsidiaries, unless otherwise stated. The Company assumes no obligation to revise or update any forward-looking statements for any reason, except as required by law.
Molina Healthcare, Inc. 2021 Form 10-K | 2
OVERVIEW
ABOUT MOLINA HEALTHCARE
Molina Healthcare, Inc., a FORTUNE 500 company (currently ranked 155), provides managed healthcare services under the Medicaid and Medicare programs, and through the state insurance marketplaces (the “Marketplace”). Molina was founded in 1980 as a provider organization serving low-income families in Southern California. We were originally organized in California as a health plan holding company and reincorporated in Delaware in 2002. We served approximately 5.2 million members as of December 31, 2021, located across 18 states.
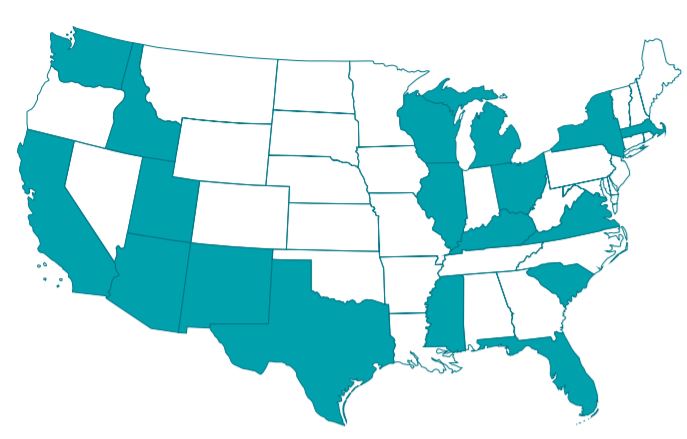
Our business footprint, as of December 31, 2021, is illustrated below.
FINANCIAL HIGHLIGHTS
| | | | | | | | | | | | | | |
| | 2021 | | 2020 |
| | (Dollars in millions, except per-share amounts) |
| | | | |
Premium Revenue | | $26,855 | | $18,299 |
Total Revenue | | $27,771 | | $19,423 |
Medical Care Ratio (“MCR”) (1) | | 88.3% | | 86.5% |
After-Tax Margin (2) | | 2.4% | | 3.5% |
Net Income per Diluted Share | | $11.25 | | $11.23 |
_______________________
(1)Medical care ratio represents medical care costs as a percentage of premium revenue.
(2)After-tax margin represents net income as a percentage of total revenue.
Molina Healthcare, Inc. 2021 Form 10-K | 3
OUR SEGMENTS
In the first quarter of 2021, we realigned our reportable operating segments to reflect recent changes in our internal operating and reporting structure, which is now organized by government program. These reportable segments consist of: 1) Medicaid; 2) Medicare; 3) Marketplace; and 4) Other.
The Medicaid, Medicare, and Marketplace segments represent the government-funded or sponsored programs under which we offer managed healthcare services. The Other segment, which is insignificant to our consolidated results of operations, includes certain corporate amounts not associated with or allocated to the Medicaid, Medicare, or Marketplace segments. Additionally, the Other segment includes service revenues and service costs associated with the long-term services and supports consultative services we now provide in Wisconsin, as a result of the Magellan Complete Care acquisition on December 31, 2020.
Refer to Notes to Consolidated Financial Statements, Note 16, “Segments,” for further information, including segment revenue and profit information.
SEGMENT MEMBERSHIP
The following table summarizes our membership by segment as of the dates indicated:
| | | | | | | | | | | |
| As of December 31, |
| 2021 | | 2020 |
| | | |
| | | |
| | | |
| Medicaid | 4,329,000 | | | 3,599,000 | |
| | | |
| | | |
| Medicare | 142,000 | | | 115,000 | |
| | | |
| Marketplace | 728,000 | | | 318,000 | |
Total (1) | 5,199,000 | | | 4,032,000 | |
____________________
(1)Approximately 200,000 members, from the Magellan Complete Care acquisition that closed on December 31, 2020, are not included in the totals as of December 31, 2020.
MISSION
We improve the health and lives of our members by delivering high-quality healthcare.
VISION
We will distinguish ourselves as the low-cost, most effective and reliable health plan delivering government-sponsored care.
STRATEGY
Our growth strategy continues to be anchored by our capital allocation priorities: first, organic growth of our core businesses by growing with new state procurement opportunities, retaining existing contracts, increasing market share in current service areas and pursuing carve-in opportunities; second, inorganic growth through accretive acquisitions; third, programmatically returning excess capital to shareholders, for example, in the form of targeted share repurchase programs; and fourth, strong MCR and general and administrative (“G&A”) management to drive attractive and sustainable margins. We are a pure-play government managed care business with synergistic segments and are committed to our core business. The key capabilities that enable our growth strategy follow:
Low-Cost: We provide low-cost health plans to our state customers for Medicaid, and to our members in the Medicare-Medicaid Plan (“MMP”) and Marketplace programs.
High Quality and Appropriate Access to Care: We provide our members effective and appropriate access to care at the right time and in the right setting.
Reliable Service and Seamless Experience: We offer our state customers, members, and providers reliable service and a seamless experience.
Strong Capital Foundation: We have a strong balance sheet that provides a foundation for stability and growth.
Right Management Team to Execute on our Growth Strategy: We have an accountable performance driven culture and a proven industry-leading team with over 20 decades of experience.
Molina Healthcare, Inc. 2021 Form 10-K | 4
Committed to Building Future Capabilities: We are building capabilities that include, but are not limited to, complex care management, scalable and agile technology infrastructure, and advanced data analytics.
KEY DEVELOPMENTS
Presented below are key recent developments and accomplishments relating to progress on our growth strategy:
New York Acquisition—Medicaid. On October 25, 2021, we closed on our acquisition of substantially all of the assets of Affinity Health Plan, Inc., a Medicaid health plan in New York. As a result, we added approximately 310,000 members in New York.
New York Acquisition—Medicaid. On October 7, 2021, we announced a definitive agreement to acquire the Medicaid Managed Long Term Care business of AgeWell New York (“AgeWell”). As of August 31, 2021, AgeWell served approximately 13,000 managed long-term services and supports members, with full-year 2020 premium revenue of approximately $700 million. The transaction is subject to applicable federal and state regulatory approvals and the satisfaction of other customary closing conditions. We currently expect the transaction to close by the third quarter of 2022.
Nevada Procurement—Medicaid. On August 17, 2021, we announced that our Nevada health plan subsidiary was selected as an awardee in Clark and Washoe Counties. This new contract commenced on January 1, 2022, and offers health coverage to TANF, CHIP and Medicaid Expansion beneficiaries. The four-year contract with a possible two-year extension was ratified in September 2021.
Texas Acquisition—Medicaid and Medicare. On January 1, 2022, we closed on our acquisition of Cigna Corporation’s Texas Medicaid and MMP contracts, along with certain operating assets.
Arizona, Virginia, Florida, Wisconsin, New York and Massachusetts. On December 31, 2020, we closed on the acquisition of Magellan Complete Care (“MCC”), a managed care organization serving members in six states, including Medicaid members in Arizona and statewide in Virginia, and Integrated Acute Care members in Florida. Through its Senior Whole Health branded plans, MCC provides fully integrated plans for Medicaid and Medicare dual beneficiaries in Massachusetts, as well as Managed Long-Term Care in New York. MCC also provides consultative services to participants who self-direct their care through Wisconsin’s long-term services and supports (“LTSS”) program. As a result, we added approximately 200,000 members in managed care plans and 25,000 LTSS program participants in Wisconsin.
Continued management of our cash, investments, and capital structure is enabling us to meet the short- and long-term objectives and obligations of our business while maintaining liquidity and financial flexibility. We have continued to execute a capital plan that has produced a strong and stable balance sheet, with a simplified capital structure, which resulted in the following accomplishments in 2021:
•In November 2021, we completed the private offering of $750 million aggregate principal amount of 3.875% senior notes due 2032. We used approximately $725 million of the net proceeds from this offering to redeem the entire $700 million outstanding principal amount of the 5.375% Notes due 2022 and to pay related fees and expenses. We intend to use the remaining net proceeds of this offering for general corporate purposes, which may include repayment of indebtedness, share repurchases, funding for acquisitions, capital expenditures, additions to working capital and capital contributions to our health plan subsidiaries to meet statutory requirements in new or existing states.
•In September 2021, our board of directors authorized the purchase of up to $500 million, in the aggregate, of our common stock. This new program immediately supersedes the stock purchase program previously approved by our board of directors in September 2020. This new program will be funded with cash on hand and extends through December 31, 2022. The exact timing and amount of any repurchase will be determined by management based on market conditions and share price, in addition to other factors, and subject to the restrictions relating to volume, price and timing under applicable law.
Molina Healthcare, Inc. 2021 Form 10-K | 5
OUR BUSINESS
MEDICAID
Overview
Medicaid was established in 1965 under the U.S. Social Security Act to provide healthcare and long-term care services and support to low-income Americans. Although jointly funded by federal and state governments, Medicaid is a state-operated and state-implemented program. Subject to federal laws and regulations, states have significant flexibility to structure their own programs in terms of eligibility, benefits, delivery of services, and provider payments. As a result, there are 56 separate Medicaid programs—one for each U.S. state, each U.S. territory, and the District of Columbia.
The federal government guarantees matching funds to states for qualifying Medicaid expenditures based on each state’s federal medical assistance percentage (“FMAP”). A state’s FMAP is calculated annually and varies inversely with average personal income in the state. The approximate average FMAP across all jurisdictions is currently 66%, and currently ranges from a federally established FMAP floor of 56% to as high as 85%. See further discussion regarding the FMAP below in “COVID-19 Pandemic—Federal Economic Stabilization and Other Programs.”
We participate in the following Medicaid programs:
•Temporary Assistance for Needy Families (“TANF”) - This is the most common Medicaid program. It primarily covers low-income families with children.
•Medicaid Aged, Blind or Disabled (“ABD”) - ABD programs cover low-income persons with chronic physical disabilities or behavioral health impairments. ABD beneficiaries typically use more services than those served by other Medicaid programs because of their critical health issues.
•Children’s Health Insurance Program (“CHIP”) - CHIP is a joint federal and state matching program that provides healthcare coverage to children whose families earn too much to qualify for Medicaid coverage. States have the option of administering CHIP through their Medicaid programs.
•Medicaid Expansion - In states that have elected to participate, Medicaid Expansion provides eligibility to nearly all low-income individuals under age 65 with incomes at or below 138% of the federal poverty line.
Our state Medicaid contracts typically have terms of three to five years, contain renewal options exercisable by the state Medicaid agency, and allow either the state or the health plan to terminate the contract with or without cause. Such contracts are subject to risk of loss in states that issue requests for proposal (“RFP”) open to competitive bidding by other health plans. If one of our health plans is not a successful responsive bidder to a state RFP, its contract may not be renewed.
In addition to contract renewal, our state Medicaid contracts may be periodically amended to include or exclude certain health benefits (such as pharmacy services, behavioral health services, or long-term care services); populations such as the aged, blind or disabled (“ABD”); and regions or service areas.
Status of Significant Contracts
Our consolidated Medicaid premium revenue constituted 74% of our total revenue in the year ended December 31, 2021. Our Medicaid contracts with each of the states of California, Ohio, Texas and Washington accounted for approximately 10% or more of our consolidated Medicaid premium revenues in each of the years ended December 31, 2021, and 2020. The current status of each of these contracts is described below.
California. Our managed care contracts with the California Department of Health Care Services (“DHCS”) cover six regions in northern and southern California (including Los Angeles County, California, as a subcontractor to another health plan holding a direct contract with the state). These contracts are effective through December 31, 2022, which we expect to be renewed annually until the effectiveness of new forms of contract following RFP awards. DHCS released the Medicaid RFP in early February 2022, for implementation in January 2024. Our California Medicaid contracts represented premium revenue of approximately $1,978 million, or 10%, of our consolidated Medicaid premium revenue in 2021.
Molina Healthcare, Inc. 2021 Form 10-K | 6
Ohio. On April 13, 2021, we announced that our Ohio health plan subsidiary was selected as an awardee in all three regions across the state pursuant to the Medicaid managed care request for application issued on September 30, 2020, by the Ohio Department of Medicaid. This new contract is expected to begin July 1, 2022, and will offer health care coverage to Medicaid beneficiaries through the state of Ohio’s Covered Family and Children, Expansion, and ABD programs. Our Ohio Medicaid contract represented approximately $2,308 million, or 11%, of our consolidated Medicaid premium revenue in 2021.
Texas. In March 2020, the Texas Health and Human Services Commission (“HHSC”) notified our Texas health plan that our protest was upheld and HHSC was canceling all October 2019 awarded contracts associated with the re-procurement for the ABD program (known in Texas as “STAR+PLUS”). In addition, HHSC canceled the pending re-procurement associated with the TANF and CHIP programs (known in Texas as “STAR/CHIP”). HHSC has indicated that the STAR+PLUS RFP will be posted in early 2022, with awards estimated to be announced in the third or fourth quarter of 2022, and start of operations in the second half of 2023. HHSC has also indicated that the STAR/CHIP RFP will be posted in the third or fourth quarter of 2022, with awards estimated to be announced in mid-2023, and start of operations in mid-2024. Our Texas Medicaid contracts represented approximately $2,158 million, or 11%, of consolidated Medicaid premium revenue in 2021.
Washington. Our managed care contract with the Washington State Health Care Authority (“HCA”) covers all ten regions of the state’s Apple Health Integrated Managed Care program, and is effective through December 31, 2021. HCA has exercised its renewal option for at least one year, through December 31, 2022. Our Washington Medicaid contract represented approximately $3,939 million, or 19%, of consolidated Medicaid premium revenue in 2021.
A loss of any of our significant Medicaid contracts could have a material adverse effect on our business, financial condition, cash flows, and results of operations.
Member Enrollment and Marketing
Most states allow eligible Medicaid members to select the Medicaid plan of their choice. This opportunity to choose a plan is typically afforded to the member at the time of first enrollment and, at a minimum, annually thereafter. In some of the states in which we operate, a substantial majority of new Medicaid members voluntarily select a plan with the remainder subject to the auto-assignment process described below, while in other states less than half of new members voluntarily choose a plan.
Our Medicaid health plans may benefit from auto-assignment of individuals who do not choose a plan, but for whom participation in managed care programs is mandatory. Each state differs in its approach to auto-assignment, but one or more of the following criteria is typical in auto-assignment algorithms: a Medicaid beneficiary's previous enrollment with a health plan or experience with a particular provider contracted with a health plan, enrolling family members in the same plan, a plan's quality or performance status, a plan’s network and enrollment size, awarding all auto-assignments to a plan with the lowest bid in a county or region, and equal assignment of individuals who do not choose a plan in a specified county or region.
Our Medicaid marketing efforts are regulated by the states in which we operate, each of which imposes different requirements for, or restrictions on, Medicaid sales and marketing. These requirements and restrictions are revised from time to time. None of the jurisdictions in which we operate permit direct sales by Medicaid health plans.
MEDICARE
Overview
Medicare Advantage. Medicare is a federal program that provides eligible persons age 65 and over and some disabled persons with a variety of hospital, medical insurance, and prescription drug benefits. Medicare is funded by Congress, and administered by the Centers for Medicare and Medicaid Services (“CMS”). Medicare beneficiaries may enroll in a Medicare Advantage plan, under which managed care plans contract with CMS to provide benefits that are comparable to original Medicare. Such benefits are provided in exchange for a fixed per-member per-month (“PMPM”) premium payment that varies based on the county in which a member resides, the demographics of the member, and the member’s health condition. Since 2006, Medicare beneficiaries have had the option of selecting a prescription drug benefit from an existing Medicare Advantage plan. The drug benefit, available to beneficiaries for a monthly premium, is subject to certain cost sharing depending upon the specific benefit design of the selected plan.
Medicare-Medicaid Plans, or MMPs. Over 12 million low-income elderly and disabled people qualify for both the Medicare and Medicaid programs (“dual eligible” individuals). These beneficiaries are more likely than other Medicare beneficiaries to be frail, live with multiple chronic conditions, and have functional and cognitive impairments. Medicare is their primary source of health insurance coverage. Medicaid supplements Medicare by paying for services not covered by Medicare, such as dental care and long-term care services and supports, and by
Molina Healthcare, Inc. 2021 Form 10-K | 7
helping to cover Medicare’s premiums and cost-sharing requirements. Together, these two programs help to shield very low-income Medicare beneficiaries from potentially unaffordable out-of-pocket medical and long-term care costs. To coordinate care and deliver services in a more financially efficient manner, some states have undertaken demonstration programs to integrate Medicare and Medicaid services for dual-eligible individuals. The health plans participating in such demonstrations are referred to as MMPs. We operate MMPs in six states, as described further below.
Contracts
We enter into Medicare and MMP contracts with CMS, in partnership with each state’s department of health and human services. Such contracts typically have terms of one to three years.
Status of MMP Contracts
Our California and Ohio MMP contracts are effective through December 31, 2022, which represented aggregate premium revenue of approximately $812 million in 2021. Our Illinois, Michigan, South Carolina and Texas MMP contracts are effective through December 31, 2023, which represented aggregate premium revenue of approximately $987 million in 2021.
Member Enrollment and Marketing
Our Medicare members may be enrolled through auto-assignment, as described above in “Medicaid—Member Enrollment and Marketing,” or by enrolling in our plans with the assistance of insurance agents employed by Molina, outside brokers, or via the Internet.
Our Medicare marketing and sales activities are regulated by CMS and the states in which we operate. CMS has oversight over all marketing materials used by Medicare Advantage plans, and in some cases has imposed advance approval requirements. CMS generally limits sales activities to those conveying information regarding benefits, describing the operations of our managed care plans, and providing information about eligibility requirements.
We employ our own insurance agents and contract with independent, licensed insurance agents to market our Medicare Advantage products. We have continued to expand our use of independent agents because the cost of these agents is largely variable and we believe the use of independent, licensed agents is more conducive to the shortened Medicare selling season and the open enrollment period. The activities of our independent, licensed insurance agents are also regulated by CMS. We also use direct mail, mass media and the Internet to market our Medicare Advantage products.
MARKETPLACE
Overview
Effective January 1, 2014, the Affordable Care Act (“ACA”) authorized the creation of Marketplace insurance exchanges, allowing individuals and small groups to purchase federally subsidized health insurance. We offer Marketplace plans in many of the states where we offer Medicaid health plans. Our plans allow our Medicaid members to stay with their providers as they transition between Medicaid and the Marketplace. Additionally, our plans remove financial barriers to quality care and seek to minimize members' out-of-pocket expenses. In 2022, we are participating in the Marketplace in all our markets except New York, Nevada and the Magellan Complete Care markets in Arizona, Massachusetts, and Virginia.
We expect Marketplace enrollment to decrease by approximately 66% in 2022, to a total of 250,000 members by the end of the year. This would represent an estimated premium revenue decline of approximately 38% in 2022, and is in line with our product and pricing strategy to achieve our target margins in this business.
Contracts
We enter into contracts with CMS annually for the state Marketplace programs. These contracts have a one-year term ending on December 31, and must be renewed annually.
Other Developments
Special Enrollment Period. In January 2021, President Biden issued the Executive Order on Strengthening Medicaid and the Affordable Care Act. As a result of the order, a new three-month special enrollment period was launched to allow uninsured and under-insured individuals to obtain Marketplace coverage. The special enrollment period was initially open from February 15, 2021 to May 15, 2021, and then extended through August 15, 2021. This special enrollment period has now ended in all of our states.
Molina Healthcare, Inc. 2021 Form 10-K | 8
Member Enrollment and Marketing
Our Marketplace members enroll in our plans with the assistance of insurance agents employed by Molina, outside brokers, vendors, direct to consumer marketing and via the Internet.
While our Marketplace sales activities are regulated by CMS (such as eligibility determinations), our marketing activities are regulated by the individual states in which we operate. Some states require us to obtain prior approval of our marketing materials, others simply require us to provide them with copies of our marketing materials, and some states do not request our marketing materials. We are able to freely contact our members and provide them with marketing materials as long as those materials are fair and do not discriminate.
Our Marketplace sales and marketing strategy is to provide high quality, affordable, compliant and consumer centric Marketplace products through a variety of distribution channels. Our Marketplace products are displayed on the Federally Facilitated Marketplace (“FFM”) and the State Based Marketplace (“SBM”) in the states in which we participate in the Marketplace. We also contract with independent, licensed insurance agents to market our Marketplace products. The activities of our independently licensed insurance agents are also regulated by both CMS and the departments of insurance in the states in which we participate. Our sales cycle typically peaks during the annual Open Enrollment Period (“OEP”) as defined and regulated by CMS and the applicable FFM and SBM.
BASIS FOR PREMIUM RATES
The following table presents our consolidated premium revenue by program for the periods indicated:
| | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 |
| | | |
| (In millions) |
| Medicaid | $ | 20,461 | | | $ | 14,265 | |
| Medicare | 3,361 | | | 2,512 | |
| Marketplace | 3,033 | | | 1,522 | |
| Total | $ | 26,855 | | | $ | 18,299 | |
Medicaid
Under our Medicaid contracts, state government agencies pay our health plans fixed PMPM rates that vary by state, line of business, demographics and, in most instances, health risk factors. CMS requires these rates to be actuarially sound. In exchange for the payment received, Molina arranges, pays for, and manages healthcare services provided to Medicaid beneficiaries. Therefore, our health plans are at risk for the medical costs associated with their members’ healthcare. Payments to us under each of our Medicaid contracts are subject to each state’s annual appropriation process. The amount of the premiums paid to our health plans may vary substantially between states and among various government programs. For the year ended December 31, 2021, Medicaid program PMPM premium revenues ranged from $170.00 to $1,580.00.
Medicare
Under Medicare Advantage, managed care plans contract with CMS to provide benefits in exchange for a fixed PMPM premium payment that varies based on health plan star rating and member demographics, including county residence and health risk factors. CMS also considers inflation, changes in utilization patterns and average per capita fee-for-service Medicare costs in the calculation of the fixed PMPM premium payment. Amounts payable to us under the Medicare Advantage contracts are subject to annual revision by CMS, including any federal budget cuts or tax changes applicable to Medicare. We elect to participate in each Medicare service area or region on an annual basis. Medicare Advantage premiums paid to us are subject to federal government reviews and audits which can result, and have resulted, in retroactive and prospective premium adjustments. Compared with our Medicaid plans, Medicare Advantage and MMP contracts generate higher average PMPM revenues and healthcare costs. For the year ended December 31, 2021, Medicare program PMPM premium revenues ranged from $1,090.00 to $3,270.00.
Marketplace
For Marketplace, we develop each state’s premium rates during the spring of each year for policies effective in the following calendar year. Premium rates are based on our estimates of utilization of services and unit costs, anticipated member risk acuity and related federal risk adjustment transfer amounts, and non-benefit expenses such as administrative costs, taxes, and fees. The premium rates are filed for approval with the various state and
Molina Healthcare, Inc. 2021 Form 10-K | 9
federal authorities in accordance with the rules and regulations applicable to the ACA individual market, including, but not limited to, minimum loss ratio thresholds and adjustments for permissible rate variations by age, geographic area, and variations in plan design. In the year ended December 31, 2021, Marketplace program PMPM premium revenues ranged from $330.00 to $590.00.
COVID-19 PANDEMIC
As the COVID-19 pandemic continues to evolve, its ultimate impact to our business, results of operations, financial condition and cash flows is uncertain and difficult to predict. Specific trends and uncertainties related to our health plans follow.
Federal Economic Stabilization and Other Programs
In addition to various programs enacted in 2020 and described in our 2020 Annual Report on Form 10-K, the $1.9 trillion American Rescue Plan Act of 2021 was enacted on March 11, 2021. This legislation includes several components to assist in COVID-19 vaccine testing and deployment, as well as provisions relating to the opening of schools; direct immediate relief to working families; and additional support for communities struggling in the wake of the pandemic. Among its specific provisions:
•$350 billion in state and local funding;
•Funding for Medicaid and CHIP COVID-19 vaccines and treatment to be matched at 100% of the FMAP;
•Incentives for states that have not expanded Medicaid to do so;
•State flexibility to extend Medicaid eligibility to women for 12 months postpartum;
•A temporary 10% FMAP increase for states to improve Medicaid home- and community-based services for one year; and
•An increase to the ACA Marketplace premium subsidies for 2021 and 2022.
In addition, effective January 16, 2022, the Biden Administration extended the COVID-19 related PHE, which, among other things, continues the suspension in state Medicaid eligibility redeterminations for at least 90 days. The PHE will remain in effect until April 16, 2022, unless earlier extended.
Also, President Biden’s January 2021 executive order providing for a three-month Marketplace special enrollment period from February 15, 2021 to May 15, 2021, was extended through August 15, 2021. This special enrollment period has now ended in all of our states.
Due to the uncertainty as to the duration and breadth of the pandemic, we are unable to reasonably estimate the ultimate impact of the economic stabilization and other programs to our business, financial condition, and operating results.
Operations
Enrollment and Premium Revenue
Excluding acquisitions and our exit from Puerto Rico, we have added approximately 750,000 new Medicaid members since March 31, 2020, when we first began to report on the impacts of the pandemic. We believe this membership increase was mainly due to the suspension of redeterminations for Medicaid eligibility. We expect Medicaid enrollment to continue to benefit from the extension of the PHE period, and the associated pause on membership redeterminations, at least through mid-April 2022.
Marketplace revenue growth was 99% in 2021, and we ended 2021 with 728,000 members, an increase of 129% compared to December 31, 2020. The growth was partially driven by the special enrollment period discussed above.
The current rate environment is stable and rational. We continue to believe that the risk-sharing corridors previously introduced are related to the declared PHE and will likely be eliminated as the COVID pandemic subsides. However, the risk corridors continue to contribute an added level of variability to our results of operations. In the year ended December 31, 2021, we recognized approximately $323 million for the impact of risk corridors enacted in several states beginning in the second quarter of 2020, in response to the lower utilization of medical services resulting from COVID-19. Approximately $564 million was recognized in 2020 related to these COVID-related risk corridors.
It is possible that certain states could change the structure of existing risk corridors, implement new risk corridors in the future or discontinue existing risk corridors. Due to these uncertainties, the ultimate outcomes could differ materially from our estimates as a result of changes in facts or further developments, which could have an adverse effect on our consolidated financial position, results of operations, or cash flows.
Molina Healthcare, Inc. 2021 Form 10-K | 10
Medical Care Costs
We expect continued uncertainty regarding utilization trends as the pandemic continues. The speed and extent to which utilization rebounds will be greatly impacted by the economy and consumer behavior, provider capacity, and the recent resurgence of COVID-19 infection rates. We believe that some portion of the utilization curtailment experienced in the year ended December 31, 2021 is likely the result of service deferrals, which will likely be provided to members over the upcoming year.
Capital and Financial Resources
We continue to monitor and assess the estimated operating and financial impact of the COVID-19 pandemic, and as it evolves, we continue to process, assemble, and assess member utilization information. We believe that our cash resources, borrowing capacity available under the Credit Agreement, and cash flow generated from operations will be sufficient to withstand the financial impact of the pandemic, and will enable us to continue to support our operations, regulatory requirements, debt repayment obligations, and capital expenditures for the foreseeable future. Refer to “Liquidity and Financial Condition” below for a discussion of our capital and financial resources.
LEGISLATIVE AND POLITICAL ENVIRONMENT
PRESSURES ON MEDICAID FUNDING
Due to states’ budget challenges, including shortfalls resulting from the COVID-19 pandemic, and political agendas at both the state and federal levels, there are a number of different legislative proposals being considered, some of which would involve significantly reduced federal or state spending on the Medicaid program, constitute a fundamental change to the federal role in healthcare and, if enacted, could have a material adverse effect on our business, financial condition, cash flows, or results of operations. These proposals include elements such as the following, as well as numerous other potential changes and reforms:
•Changes in the entitlement nature of Medicaid (and perhaps Medicare as well) by capping future increases in federal health spending for these programs, and shifting much more of the risk for health costs in the future to states and consumers;
•Reversing the ACA’s expansion of Medicaid that enables states to cover low-income childless adults;
•Changing Medicaid to a state block grant program, including potentially capping spending on a per-enrollee basis;
•Requiring Medicaid beneficiaries to work; and
•Limiting the amount of lifetime benefits for Medicaid beneficiaries.
AFFORDABLE CARE ACT
Status of Constitutionality Court Case
In December 2018, a federal judge in Texas held that the individual mandate of the Affordable Care Act (the “ACA”) and thus the entire ACA, is unconstitutional. On appeal, in December 2019, a three-judge panel of the Fifth Circuit Court of Appeal, in a two to one decision, affirmed the District Court’s ruling that the individual mandate is unconstitutional, but remanded the case back to the District Court for further consideration of the severability issue. The intervenor defendant states led by California subsequently appealed the case to the U.S. Supreme Court, and the Supreme Court heard oral arguments in the case on November 10, 2020. In June 2021, the Supreme Court held in a 7-2 opinion that the states and individuals that brought the lawsuit challenging the ACA’s individual mandate did not have standing to challenge the law. Although the Supreme Court did not reach the merits of the challenge, it vacated the District Court’s judgment and remanded the case with instructions to dismiss—effectively ending the case. There are no changes to our business as a result of the decision.
Other Proposed Changes and Reforms
Other proposed changes and reforms to the ACA have included, or may include the following:
•Prohibiting the federal government from operating Marketplaces;
•Eliminating the advanced premium tax credits, and cost sharing reductions for low income individuals who purchase their health insurance through the Marketplaces;
•Expanding and encouraging the use of private health savings accounts;
•Providing for insurance plans that offer fewer and less extensive health insurance benefits than under the ACA’s essential health benefits package, including broader use of catastrophic coverage plans, or short-
Molina Healthcare, Inc. 2021 Form 10-K | 11
term health insurance;
•Establishing and funding high risk pools or reinsurance programs for individuals with chronic or high cost conditions; and
•Allowing insurers to sell insurance across state lines.
The passage of any of these changes or other reforms could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
CORPORATE TAX REFORM
Recent proposals related to corporate tax reform propose raising corporate taxes, among other things. Some proposed reforms could have a material impact on our future results of operations. We will continue to monitor developments.
OPERATIONS
QUALITY
Our long-term success depends, to a significant degree, on the quality of the services we provide. As of December 31, 2021, 13 of our health plans were accredited by the National Committee for Quality Assurance (“NCQA”), of which 12 of those health plans also received the Multicultural Health Care Distinction, which is awarded to organizations that meet or exceed NCQA’s rigorous requirements for multicultural healthcare.
For the states where our health plans are accredited by the NCQA and/or have Medicare Star Ratings, the table below presents such health plans’ NCQA status, as well as their current scores as part of the Medicare Star Ratings, which measures the quality of Medicare plans across the country using a 5-star rating system.
We believe that these objective measures of quality are important to state Medicaid agencies, as a growing number of states link reimbursement and patient assignment to quality scores. Additionally, Medicare pays quality bonuses to health plans that achieve high quality.
Molina Healthcare, Inc. 2021 Form 10-K | 12
PROVIDERS
We arrange healthcare services for our members through contracts with a vast network of providers, including independent physicians and physician groups, hospitals, ancillary providers, and pharmacies. We strive to ensure that our providers have the appropriate expertise and cultural and linguistic experience.
The quality, depth and scope of our provider network are essential if we are to ensure quality, cost-effective care for our members. In partnering with quality, cost-effective providers, we utilize clinical and financial information derived by our medical informatics function, as well as the experience we have gained in serving Medicaid members, to gain insight into the needs of both our members and our providers.
Physicians
We contract with both primary care physicians and specialists, many of whom are organized into medical groups or independent practice associations. Primary care physicians provide office-based primary care services. Primary care physicians may be paid under capitation or fee-for-service contracts and may receive additional compensation by providing certain preventive care services. Under capitation payment arrangements, healthcare providers receive fixed, pre-arranged monthly payments per enrolled member, whereas under fee-for-service payment arrangements, healthcare providers are paid a fee for each particular service rendered. Our specialists care for patients for a specific episode or condition, usually upon referral from a primary care physician, and are usually compensated on a fee-for-service basis. When we contract with groups of physicians on a capitated basis, we monitor their solvency.
Hospitals
We generally contract with hospitals that have significant experience dealing with the medical needs of the Medicaid population. We reimburse hospitals under a variety of payment methods, including fee-for-service, per diems, diagnostic-related groups, capitation, and case rates.
Ancillary Providers
Our ancillary agreements provide coverage of medically-necessary care, including laboratory services, home health, physical, speech and occupational therapy, durable medical equipment, radiology, ambulance and transportation services, and are reimbursed on a capitation and fee-for-service basis.
Pharmacy
We outsource pharmacy benefit management services, including claims processing, pharmacy network contracting, rebate processing and mail and specialty pharmacy fulfillment services.
MEDICAL MANAGEMENT
Our mission is to improve the health and lives of our members by delivering high-quality healthcare. We believe our singular focus on government-sponsored healthcare enables us to identify and implement efficiencies that distinguish us as the low-cost, high-quality health plan of choice. We emphasize primary care physicians as the central point of delivery for routine and preventive care, coordination of referrals to specialists, and appropriate assessment of the need for hospital care. This model has proved to be an effective method of coordinating medical care for our members.
Utilization Management
Our goal is to optimize access to low-cost, high-quality care. This is achieved by sound clinical policy based on current evidence-based practices. Additionally, we continuously monitor utilization patterns and strive to identify new opportunities to reduce cost and improve quality of care. Our utilization management process serves as a bridge to identify at-risk members for referral into internally developed case management programs such as “Transitions of Care,” which facilitates post-discharge safety and appropriate outcomes.
Population Management
We believe high-quality, affordable care is achieved through a variety of programs tailored to our members’ emerging needs. Individuals are identified for interventions, and programs are customized, based on predictive analytics and our member assessment process. These tools ensure that the appropriate level of services and support are provided to address physical health, behavioral health, and social determinants of health. This comprehensive and customized approach is designed to help members achieve their goals and improve their overall quality of life.
Molina Healthcare, Inc. 2021 Form 10-K | 13
Pharmacy Management
Our pharmacy programs are designed to make us a trusted partner in improving member health and healthcare affordability. We strategically partner with physicians and other healthcare providers who treat our members. This collaboration results in drug formularies and clinical initiatives that promote improved patient care. We employ full-time pharmacists and pharmacy technicians who work closely with providers to educate them about our formulary products, clinical programs, and the importance of cost-effective care.
Medical Cost Management
We use various strategies to mitigate the negative effects of healthcare cost inflation. Specifically, our health plans try to control medical care costs through contracts with independent providers of healthcare services. Through these contracted providers, our health plans emphasize preventive healthcare and appropriate use of specialty and hospital services. There can be no assurance, however, that our strategies to mitigate medical care cost inflation will be successful. Competitive pressures, new healthcare and pharmaceutical product introductions, demands from healthcare providers and customers, applicable regulations, or other factors may affect our ability to control medical care costs.
INFORMATION TECHNOLOGY
Our business is dependent on effective and secure information systems that assist us in processing provider claims, monitoring utilization and other cost factors, supporting our medical management techniques, providing data to our regulators, and implementing our data security measures. Our members and providers also depend upon our information systems for enrollment, premium processing, primary care and specialist physician roster access, membership verifications, claims status, provider payments, and other information.
We have partnered with third parties to support our information technology systems. This makes our operations vulnerable to adverse effects if such third parties fail to perform adequately. In 2019, we entered into an agreement with a third-party vendor who manages certain of our information technology services including, among other things, our infrastructure operations, end-user services, data centers, public cloud and application management. As a result of the agreement, we were able to reduce our administrative expenses, while improving the reliability of our information technology functions, and maintain targeted levels of service and operating performance. A portion of these services are provided on our premises, while other portions of the services are performed at the vendor’s facilities.
Our information systems require an ongoing commitment of significant resources to maintain, protect, and enhance existing systems and develop new systems to keep pace with continuing changes in information processing technology, evolving systems and regulatory standards, changing customer preferences, acquisitions and increased security risks.
CENTRALIZED SERVICES
We provide certain centralized medical and administrative services to our subsidiaries pursuant to administrative services agreements that include, but are not limited to, information technology, product development and administration, underwriting, claims processing, customer service, certain care management services, human resources, marketing, purchasing, risk management, actuarial, finance, accounting, compliance, legal and public relations.
COMPETITIVE CONDITIONS AND ENVIRONMENT
We face varying levels of competition. Healthcare reform proposals may cause organizations to enter or exit the market for government-sponsored health programs. However, the licensing requirements and bidding and contracting procedures in some states may present partial barriers to entry into our industry.
We compete for government contracts, renewals of those government contracts, members, and providers. State agencies consider many factors in awarding contracts to health plans. Among such factors are the health plan’s provider network, quality scores, medical management, degree of member satisfaction, timeliness of claims payment, and financial resources. Potential members typically choose a health plan based on a specific provider being a part of the network, the quality of care and services available, accessibility of services, and reputation or name recognition of the health plan. We believe factors that providers consider in deciding whether to contract with a health plan include potential member volume, payment methods, timeliness and accuracy of claims payment, and administrative service capabilities.
Molina Healthcare, Inc. 2021 Form 10-K | 14
Medicaid
The Medicaid managed care industry is subject to ongoing changes as a result of healthcare reform, business consolidations and new strategic alliances. We compete with national, regional, and local Medicaid service providers, principally on the basis of size, location, quality of the provider network, quality of service, and reputation. Our primary competitors in the Medicaid managed care industry include Centene Corporation, UnitedHealth Group Incorporated, Anthem, Inc., Aetna Inc., and other large not-for-profit healthcare organizations. Competition can vary considerably from state to state.
Medicare
The Medicare market is highly competitive across the country, with large competitors, such as UnitedHealth Group Incorporated, Humana Inc., and Aetna Inc., holding significant market share.
Marketplace
Low-income members who receive government subsidies comprise the vast majority of Marketplace membership, which is served by a limited number of health plans. Our primary competitor for low-income Marketplace membership is Centene Corporation.
REGULATION
Our health plans are highly regulated by both state and federal government agencies. Regulation of managed care products and healthcare services varies from jurisdiction to jurisdiction, and changes in applicable laws and rules occur frequently. Regulatory agencies generally have discretion to issue regulations and interpret and enforce laws and rules. Compliance with such laws and rules may lead to additional costs related to the implementation of additional systems, procedures and programs that we have not yet identified. Such agencies have become increasingly active in recent years in their review and scrutiny of health insurers and managed care organizations, including those operating in the Medicaid and Medicare programs.
HIPAA AND THE HITECH ACT
In 1996, Congress enacted the Health Insurance Portability and Accountability Act (“HIPAA”). All health plans are subject to HIPAA, including ours. HIPAA generally requires health plans to:
•Establish the capability to receive and transmit electronically certain administrative healthcare transactions, such as claims payments, in a standardized format;
•Afford privacy to patient health information; and
•Protect the privacy of patient health information through physical and electronic security measures.
In 2009, the Health Information Technology for Economic and Clinical Health Act (“HITECH”) imposed requirements on uses and disclosures of health information; included requirements for HIPAA business associate agreements; extended parts of HIPAA privacy and security provisions to business associates; added data breach notification requirements for covered entities and business associates and reporting requirements to the U.S. Department of Health and Human Services (“HHS”) and, in some cases, to the media; strengthened enforcement; and imposed higher financial penalties for HIPAA violations. In the conduct of our business, depending on the circumstances, we may act as either a covered entity and/or a business associate. HIPAA privacy regulations do not preempt more stringent state laws and regulations that may apply to us.
We maintain a HIPAA compliance program, which we believe complies with HIPAA privacy and security regulations, and have dedicated resources to monitor compliance with this program.
Healthcare reform created additional tools for fraud prevention, including increased oversight of providers and suppliers participating or enrolling in Medicaid, CHIP, and Medicare. Those enhancements included mandatory licensure for all providers, and site visits, fingerprinting, and criminal background checks for higher risk providers.
FRAUD AND ABUSE LAWS AND THE FALSE CLAIMS ACT
Because we receive payments from federal and state governmental agencies, we are subject to various laws commonly referred to as “fraud and abuse” laws, including federal and state anti-kickback statutes, prohibited referrals, and the federal False Claims Act, which permit agencies and enforcement authorities to institute a suit against us for violations and, in some cases, to seek treble damages, criminal and civil fines, penalties, and assessments. Violations of these laws can also result in exclusion, debarment, temporary or permanent suspension
Molina Healthcare, Inc. 2021 Form 10-K | 15
from participation in government healthcare programs, or the institution of corporate integrity agreements. Liability under such federal and state statutes and regulations may arise if we know, or it is determined that we should have known, that information we provide to form the basis for a claim for government payment is false or fraudulent, and some courts have permitted False Claims Act suits to proceed if the claimant was out of compliance with program requirements.
Fraud, waste and abuse prohibitions encompass a wide range of operating activities, including kickbacks or other inducements for referral of members or for the coverage of products (such as prescription drugs) by a plan, billing for unnecessary medical services by a provider, upcoding, payments made to excluded providers, improper marketing, and the violation of patient privacy rights. In particular, there has recently been increased scrutiny by the Department of Justice on health plans’ risk adjustment practices, particularly in the Medicare program. Companies involved in public healthcare programs such as Medicaid and Medicare are required to maintain compliance programs to detect and deter fraud, waste and abuse, and are often the subject of fraud, waste and abuse investigations and audits.
The federal government has taken the position that claims presented in violation of the federal anti-kickback statute may be considered a violation of the federal False Claims Act. In addition, under the federal civil monetary penalty statute, the HHS Office of Inspector General has the authority to impose civil penalties against any person who, among other things, knowingly presents, or causes to be presented, certain false or otherwise improper claims. Qui tam actions under federal and state law are brought by a private individual, known as a relator, on behalf of the government. A relator who brings a successful qui tam lawsuit can receive 15 to 30 percent of the damages the government recovers from the defendants, which damages are trebled under the False Claims Act. Because of these financial inducements offered to plaintiffs, qui tam actions have increased significantly in recent years, causing greater numbers of healthcare companies to incur the costs of having to defend false claims actions, many of which are spurious and without merit. In addition, meritorious false claims actions could result in fines, or debarment from the Medicare, Medicaid, or other state or federal healthcare programs.
LICENSING AND SOLVENCY
Our health plans are generally licensed by the insurance departments in the states in which they operate, except the following: our California health plan is licensed by the California Department of Managed Health Care; one of our New York health plans is licensed as a prepaid health services plan by the New York State Department of Health; and our Massachusetts health plan acquired on December 31, 2020, is regulated as a risk-bearing entity by the Massachusetts Executive Office of Health and Human Services.
Our health plans are subject to stringent requirements to maintain a minimum amount of statutory capital determined by statute or regulation, and restrictions that limit their ability to pay dividends to us. For further information, refer to the Notes to Consolidated Financial Statements, Note 15, “Commitments and Contingencies—Regulatory Capital Requirements and Dividend Restrictions.”
HUMAN CAPITAL
As of December 31, 2021, we had nearly 14,000 employees. This includes over 2,600 employees we onboarded through the acquisitions of Magellan Complete Care, Passport, Evolent and Affinity Health Plan. Our diverse employee population reflects the diversity of the members and communities we serve.
Over the last couple of years, we have increased our focus on the health and safety of our employees. In response to the COVID-19 pandemic, we have offered a number of new benefits to our employees, including but not limited to supplemental compensation, paid time away and resources to support changing work-life needs.
As part of our workplace modernization program, we continue to introduce improvements focused on employee development, diversity, equity and inclusion, total rewards offerings and human capital policies and practices. We believe these improvements help us to achieve our goal to become a destination employer in the government-sponsored healthcare industry.
Annually, we invite all employees to participate in our engagement survey. The purpose of our survey is to obtain honest, comprehensive feedback on what is going well and which strategic, operational or cultural concerns are top of mind for our employees. Our results compare favorably to the benchmark data about all other employers.
Succession planning and managing our talent pipelines are key to our human capital strategy. We regularly monitor high performer retention and development. Our performance management practices and pay and recognition
Molina Healthcare, Inc. 2021 Form 10-K | 16
programs are aligned with meeting and exceeding our corporate objectives. The board of directors has purview to our employee engagement results, key executive performance and succession planning.
We offer formal leadership development programs such as new leader orientation, executive onboarding, front- line leadership essentials, and experienced leader training. We have targeted development plans for critical roles with an emphasis on leadership and business acumen.
We invest in our workforce through market competitive total rewards including, pay, benefits and time-off. Our pay and recognition program is designed to engage, motivate and reward top performers and attract new employees. To foster ownership and align the interests of employees with shareholders, we offer an employee stock purchase plan and grant equity-based compensation under our long-term incentive plan to eligible employees.
We also offer a comprehensive suite of benefits to all eligible employees, including, among others:
•Comprehensive health insurance coverage for employees working 30 hours or more per week;
•401(k) matching contributions of up to 100% on the first 4% contributed by the employee;
•Personal time off that provides employees with paid time away from work, combining vacation and sick leave;
•Volunteer time off that provides employees with paid time away from work to build strong community partnerships and connect with the people we serve;
•Employee wellness programs that provide tools and incentives to live a healthy life focusing on physical, emotional, financial and work well-being;
•Up to ten dependent-care back-up visits per year for a low co-pay, and five hours of homework and tutoring support per child per month at no cost;
•Employee assistance program benefits that provides up to six confidential counseling sessions per rolling 12-month period and includes assistance with physical, emotional, and financial related matters; and
•Employee discount and other programs, including tuition reimbursement.
AVAILABLE INFORMATION
Our principal executive offices are located at 200 Oceangate, Suite 100, Long Beach, California 90802, and our telephone number is (562) 435-3666. We also maintain corporate offices in New York City, New York.
You can access our website at www.molinahealthcare.com to learn more about our Company. From that site, you can download and print copies of our Annual Reports on Form 10-K, Quarterly Reports on Form 10-Q, and Current Reports on Form 8-K, along with amendments to those reports. You can also download our Corporate Governance Guidelines, board of director’s committee charters, Code of Business Conduct and Ethics and Environmental, Social and Governance Report. We make periodic reports and amendments available, free of charge, as soon as reasonably practicable after we file or furnish these reports to the U.S. Securities and Exchange Commission (“SEC”). We will also provide a copy of any of our corporate governance policies published on our website free of charge, upon request. To request a copy of any of these documents, please submit your request to: Molina Healthcare, Inc., 200 Oceangate, Suite 100, Long Beach, California 90802, Attn: Investor Relations. Information on or linked to our website is neither part of nor incorporated by reference into this Form 10-K or any other SEC filings.
Molina Healthcare, Inc. 2021 Form 10-K | 17
RISK FACTORS
You should carefully consider the risks described below and all of the other information set forth in this Form 10-K, including our consolidated financial statements and accompanying notes. These risks and other factors may affect our forward-looking statements, including those we make in this Form 10-K or elsewhere, such as in press releases, presentations to securities analysts or investors, or other communications made by or with the approval of one of our executive officers.
The risks described in the following section are not the only risks facing our Company. Additional risks that we are unaware of, or that we currently believe are not material, may also become important factors that adversely affect our business. In addition to the risks relating to the COVID-19 pandemic that are specifically described in these risk factors, the effects of the COVID-19 pandemic may also have the effect of significantly heightening many of the other risks associated with our business, including those described below. If any of the following risks actually occurs, our business, financial condition, results of operations, and future prospects could be materially and adversely affected. In that event, among other effects, the trading price of our common stock could decline, and you could lose part or all of your investment.
RISKS RELATED TO OUR INDUSTRY
Our business, financial condition, cash flows, and results of operations will continue to be impacted by the COVID-19 pandemic, and the extent of such impact cannot be reasonably foreseen at this time.
We currently expect that the COVID-19 pandemic will continue to impact our business, financial condition, cash flows, and results of operations in a number of ways, including the following:
•It will have an adverse impact on the health of an indeterminate number of our members, resulting in increases in their medical care costs, as well as increased costs related to testing and vaccination protocols;
•Spikes in hospitalizations and positive COVID-19 cases due to the continued emergence of variants, such as Delta, Omicron, and any new variants of potentially greater transmissibility and virulence that may emerge in 2022 and beyond could also increase the cost of caring for our members;
•Uncertainty and variability associated with the demand for medical services may lead states to pursue retroactive rate refunds (as has already occurred in certain instances), or to impose medical cost risk corridors or rate cuts that exceed the ultimate demand for medical services;
•Disrupted care patterns, as a result of the pandemic, may temporarily affect the ability to obtain complete member health status information, impacting future revenue in our Medicare and Marketplace lines of business, which utilize risk adjustment methodologies;
•As a result of the pandemic’s impact on the national economy, state tax revenues have declined significantly and may not recover in 2022, resulting in the extension of risk corridors or rate cuts, and also threatening the ability of states to make timely monthly capitation payments to us;
•The reduced demand for certain routine and non-critical medical services has created financial stress for certain providers and could result in the insolvency of such providers;
•The pandemic may continue to cause increased volatility in the capital markets and such volatility could have a negative impact on our ability to access those markets on acceptable terms;
•We will continue to incur increased costs associated with the measures we are currently implementing and planning to implement to mitigate the implications of the COVID-19 pandemic;
•The continuing work-from-home status of our workforce may heighten the risk of a cybersecurity incident or HIPAA (as defined below) breach;
•The pandemic may impact the ability of our outsourced information technology service providers, and other third-party vendors, to perform contracted services; and
•The PHE and associated suspension in redeterminations, and the potential impact on our workforce or contractors of federal or state vaccine mandates, could adversely affect our business.
Due to the uncertainty around the duration and breadth of the COVID-19 pandemic and its broad cascading effects, the ultimate impact on our business, financial condition, cash flows, and operating results cannot be reasonably estimated at this time.
Molina Healthcare, Inc. 2021 Form 10-K | 18
State and federal budget deficits may result in Medicaid, CHIP, or Medicare funding cuts which could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
Nearly all of our premium revenues come from the joint federal and state funding of the Medicaid, Medicare, and CHIP programs. The states in which we operate regularly face significant budgetary pressures. State budgetary pressures may result in unexpected Medicaid, CHIP, or Medicare rate cuts which could reduce our revenues and profit margins. For example, in 2020, and continuing through December 31, 2021, various states enacted temporary risk corridors in response to the reduced demand for medical services stemming from COVID-19, which have resulted in a reduction of our medical margin. In some cases, these risk corridors were retroactive to earlier periods in 2020, or as early as the beginning of the states’ fiscal years in 2019. Beginning in the second quarter of 2020, we have recognized retroactive risk corridors that we believe to be probable, and where the ultimate premium amount is reasonably estimable. We recognized approximately $323 million related to such risk corridors in 2021, primarily in the Medicaid segment. It is possible that certain states could change the structure of existing risk corridors, implement new risk corridors in the future or discontinue existing risk corridors. Due to these uncertainties, the ultimate outcomes could differ materially from our estimates as a result of changes in facts or further developments, which could have an adverse effect on our consolidated financial position, results of operations, or cash flows.
The Medicare-Medicaid Duals Demonstration Pilot Programs could be discontinued or altered, resulting in a loss of premium revenue.
To coordinate care for those who qualify to receive both Medicare and Medicaid services (the “dual eligibles”), and to deliver services to these individuals in a more financially efficient manner, under the direction of CMS some states implemented demonstration pilot programs to integrate Medicare and Medicaid services for the dual eligibles. The health plans participating in such demonstrations are referred to as Medicare-Medicaid Plans (“MMPs”). We operate MMPs in six states: California, Illinois, Michigan, Ohio, South Carolina, and Texas. At December 31, 2021, our membership included approximately 69,000 integrated MMP members, representing approximately 1% of our total membership. However, the capitation paid to us for dual eligibles is significantly higher than the capitation paid for other members, representing 7% of our total premium revenues in 2021. If the states running the MMP demonstration pilot programs where we have members conclude that the demonstration pilot programs are not delivering better coordinated care and reduced costs, or they perceive other lack of benefits in the pilot programs, they may decide to discontinue such programs. If an MMP pilot program were discontinued and not succeeded by a substitutive program in which we participated, our premium revenues could be reduced.
If state regulators do not approve payments of dividends and distributions by our subsidiaries, it may negatively affect our ability to meet our debt service and other obligations.
We are a corporate parent holding company and hold most of our assets in, and conduct most of our operations through, our direct subsidiaries. As a holding company, our results of operations depend on the results of operations of our subsidiaries. Moreover, we are dependent on dividends or other intercompany transfers of funds from our subsidiaries to meet our debt service and other obligations. The ability of our subsidiaries to pay dividends or make other payments or advances to us will depend on their operating results and will be subject to applicable laws and restrictions contained in agreements governing the debt of such subsidiaries. In addition, our health plan subsidiaries are subject to laws and regulations that limit the amount of ordinary dividends and distributions that they can pay to us without prior approval of, or notification to, state regulators. In general, our health plans must give thirty days’ advance notice and the opportunity to disapprove “extraordinary” dividends to the respective state departments of insurance for amounts that exceed either (a) ten percent of surplus or net worth at the prior year end or (b) the net income for the prior year, depending on the respective state statute. The discretion of the state regulators, if any, in approving or disapproving a dividend is not clearly defined. Our health plans generally must provide notice to the applicable state regulator prior to paying a dividend or other distribution to us. Our parent company received $564 million and $635 million in dividends from our regulated health plan subsidiaries during 2021 and 2020, respectively. If the regulators were to deny or significantly restrict our subsidiaries’ requests to pay dividends to us, the funds available to our Company as a whole would be limited, which could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
Our use and disclosure of personally identifiable information and other non-public information, including protected health information, is subject to federal and state privacy and security regulations, and our failure to comply with those regulations or to adequately secure the information we hold could result in significant liability or reputational harm.
State and federal laws and regulations including, but not limited to, the Health Insurance Portability and Accountability Act, as amended by the Health Information Technology for Economic and Clinical Health Act, and all regulations promulgated thereunder (collectively, “HIPAA”), the California Consumer Privacy Act (the “CCPA”) and the Gramm-Leach-Bliley Act, govern the collection, dissemination, use, privacy, confidentiality, security, availability,
Molina Healthcare, Inc. 2021 Form 10-K | 19
and integrity of personally identifiable information (“PII”), including protected health information (“PHI”). HIPAA establishes basic national privacy and security standards for protection of PHI by covered entities and business associates, including health plans such as ours. HIPAA requires covered entities like us to develop and maintain policies and procedures regarding PHI, and to adopt administrative, physical, and technical safeguards to protect PHI.
HIPAA violations may result in significant civil penalties. HIPAA authorizes state attorneys general to file suit under HIPAA on behalf of state residents. Courts can award damages, costs, and attorneys’ fees related to violations of HIPAA in such cases. We have experienced HIPAA breaches in the past, including breaches affecting over 500 individuals.
Even when HIPAA does not apply, according to the Federal Trade Commission (the “FTC”), failing to take appropriate steps to keep consumers’ personal information secure constitutes unfair acts or practices in or affecting commerce in violation of Section 5(a) of the Federal Trade Commission Act, 15 U.S.C § 45(a). The FTC expects a company’s data security measures to be reasonable and appropriate in light of the sensitivity and volume of consumer information it holds, the size and complexity of its business, and the cost of available tools to improve security and reduce vulnerabilities. Individually identifiable health information is considered sensitive data that merits stronger safeguards. The FTC’s guidance for appropriately securing consumers’ personal information is similar to what is required by the HIPAA security regulations.
In addition, certain state laws govern the privacy and security of health information in certain circumstances, many of which differ from each other in significant ways, thus complicating compliance efforts. For example, California enacted the CCPA, which became effective on January 1, 2020. The CCPA, among other things, creates new data privacy obligations for covered companies and provides new privacy rights to California residents, including the right to opt out of certain disclosures of their information. The CCPA also creates a private right of action with statutory damages for certain data breaches, thereby potentially increasing risks associated with a data breach.
If we do not comply with existing or new laws and regulations related to PHI, PII, or non-public information, we could be subject to criminal or civil sanctions. Any security breach involving the misappropriation, loss, or other unauthorized disclosure or use of confidential member information, whether by us or a third party, such as our vendors, could subject us to civil and criminal penalties, divert management’s time and energy, and have a material adverse effect on our business, financial condition, cash flows, or results of operations.
Unforeseen changes in pharmaceutical regulations or market conditions may impact our revenues and adversely affect our results of operations.
Pharmaceutical products and services are a significant component of our healthcare costs. Evolving regulations and state and federal mandates regarding coverage may impact the ability of our health plans to continue to receive existing price discounts on pharmaceutical products for our members. Other factors affecting our pharmaceutical costs include, but are not limited to, the price of pharmaceuticals, geographic variation in utilization of new and existing pharmaceuticals, and changes in discounts. The unpredictable nature of these factors may have a material adverse effect on our business, financial condition, cash flows, or results of operations.
Increases in our pharmaceutical costs could have a material adverse effect on the level of our medical costs and our results of operations.
Introduction of new high cost specialty drugs and sudden cost spikes for existing drugs increase the risk that the pharmacy cost assumptions used to develop our capitation rates are not adequate to cover the actual pharmacy costs, which jeopardizes the overall actuarial soundness of our rates. Bearing the high costs of new specialty drugs or the high cost inflation of generic drugs without an appropriate rate adjustment or other reimbursement mechanism would have an adverse impact on our financial condition and results of operations. In addition, evolving regulations and state and federal mandates regarding coverage may impact the ability of our health plans to continue to receive existing price discounts on pharmaceutical products for our members. Other factors affecting our pharmaceutical costs include, but are not limited to, geographic variation in utilization of new and existing pharmaceuticals, changes in discounts, civil investigations, and litigation. Some of our competitors have been subject to substantial sanctions related to allegations of improper transfer pricing practices. Further, our principal pharmacy benefit manager, or PBM, CVS Caremark (“CVS”), is party to certain lawsuits and putative class actions regarding its drug pricing practices and its rebate arrangements with drug manufacturers. The ultimate outcome of these complaints may have an adverse impact on our pharmaceutical costs, or potentially could result in our becoming involved or impleaded into similar or related costly litigation. Although we will continue to work with state Medicaid agencies in an effort to ensure that we receive appropriate and actuarially sound reimbursement for all new drug therapies and pharmaceuticals trends, there can be no assurance that we will be successful in that regard.
Molina Healthcare, Inc. 2021 Form 10-K | 20
Large-scale medical emergencies in one or more states in which we operate our health plans could significantly increase utilization rates and medical costs.
Large-scale medical emergencies can take many forms and be associated with widespread illness or medical conditions. For example, natural disasters, such as a major earthquake or wildfire in California, or a major hurricane affecting Florida, South Carolina or Texas, could have a significant impact on the health of a large number of our covered members. Other conditions that could impact our members include a virulent flu season or epidemic, newly emergent mosquito-borne illnesses, such as the Zika virus, the West Nile virus, or the Chikungunya virus, or new viruses such as COVID-19, conditions for which vaccines may not exist, are not effective, or have not been widely administered.
In addition, federal and state law enforcement officials have issued warnings about potential terrorist activity involving biological or other weapons of mass destruction. All of these conditions, and others, could have a significant impact on the health of the population of wide-spread areas. If one of the states in which we operate were to experience a large-scale natural disaster, a significant terrorist attack, or some other large-scale event affecting the health of a large number of our members, our covered medical expenses in that state would rise, which could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
We face various risks inherent in the government contracting process that could materially and adversely affect our business and profitability, including periodic routine and non-routine reviews, audits, and investigations by government agencies.
We are subject to various risks inherent in the government contracting process. These risks include routine and non-routine governmental reviews, audits, and investigations, and compliance with government reporting requirements. Violation of the laws, regulations, or contract provisions governing our operations, or changes in interpretations of those laws and regulations, could result in the imposition of civil or criminal penalties, the cancellation of our government contracts, the suspension or revocation of our licenses, the exclusion from participation in government sponsored health programs, or the revision and recoupment of past payments made based on audit findings. If we are unable to correct any noted deficiencies, or become subject to material fines or other sanctions, we could suffer a substantial reduction in profitability, and could also lose one or more of our government contracts. In addition, government receivables are subject to government audit and negotiation, and government contracts are vulnerable to disagreements with the government. The final amounts we ultimately receive under government contracts may be different from the amounts we initially recognize in our financial statements.
Any changes to the laws and regulations governing our business, or the interpretation and enforcement of those laws or regulations, could require us to modify our operations and could negatively impact our operating results.
Our business is extensively regulated by the federal government and the states in which we operate. The laws and regulations governing our operations are generally intended to benefit and protect health plan members and providers rather than managed care organizations. The government agencies administering these laws and regulations have broad latitude in interpreting and applying them. Changes in the interpretation or application of our contracts could reduce our profitability if we have detrimentally relied on a prior interpretation or application. These laws and regulations, along with the terms of our government contracts, regulate how we do business, what services we offer, and how we interact with our members and the public. For instance, some states mandate minimum medical expense levels as a percentage of premium revenues. These laws and regulations, and their interpretations, are subject to frequent change. The interpretation of certain contract provisions by our governmental regulators may also change. Changes in existing laws or regulations, or their interpretations, or the enactment of new laws or regulations, could reduce our profitability by imposing additional capital requirements, increasing our liability, increasing our administrative and other costs, increasing mandated benefits, forcing us to restructure our relationships with providers, requiring us to implement additional or different programs and systems, or making it more difficult to predict future results. For example, on January 18, 2022, New York’s Governor unveiled the Executive Budget proposal for the fiscal year 2023 which, among other things, includes proposed changes to the procurement process with respect to procurement of managed care plans in certain of New York’s existing managed care lines. Among other things, if the Executive Budget proposal is approved in its current form, the State would be required to select two plans per product line, per region, but no more than five plans in a region. Currently, we operate our Medicaid Managed Care (“MMC”) and Health and Recovery Plans (“HARP”) plans in six of the eight CMS rating regions in New York. If the proposed Executive Budget is approved in its current form, our business, financial condition, cash flows, or results of operations could be adversely affected.
Molina Healthcare, Inc. 2021 Form 10-K | 21
We are subject to extensive fraud and abuse laws that may give rise to lawsuits and claims against us, the outcome of which may have a material adverse effect on our business, financial condition, cash flows, or results of operations.
Because we receive payments from federal and state governmental agencies, we are subject to various laws commonly referred to as “fraud and abuse” laws, including federal and state anti-kickback statutes, prohibited referrals, and the federal False Claims Act, which permit agencies and enforcement authorities to institute a suit against us for violations and, in some cases, to seek treble damages, criminal and civil fines, penalties, and assessments. Violations of these laws can also result in exclusion, debarment, temporary or permanent suspension from participation in government healthcare programs, or the institution of corporate integrity agreements. Liability under such federal and state statutes and regulations may arise if we know, or it is determined that we should have known, that information we provide to form the basis for a claim for government payment is false or fraudulent, and some courts have permitted False Claims Act suits to proceed if the claimant was out of compliance with program requirements.
Fraud, waste and abuse prohibitions encompass a wide range of operating activities, including kickbacks or other inducements for referral of members or for the coverage of products (such as prescription drugs) by a plan, billing for unnecessary medical services by a provider, upcoding, payments made to excluded providers, improper marketing, and the violation of patient privacy rights. In particular, there has recently been increased scrutiny by the Department of Justice on health plans’ risk adjustment practices, particularly in the Medicare program. Companies involved in public healthcare programs such as Medicaid and Medicare are required to maintain compliance programs to detect and deter fraud, waste and abuse, and are often the subject of fraud, waste and abuse investigations and audits.
The federal government has taken the position that claims presented in violation of the federal anti-kickback statute may be considered a violation of the federal False Claims Act. In addition, under the federal civil monetary penalty statute, the U.S. Department of Health and Human Services’ Office of Inspector General has the authority to impose civil penalties against any person who, among other things, knowingly presents, or causes to be presented, certain false or otherwise improper claims. Qui tam actions under federal and state law are brought by a private individual, known as a relator, on behalf of the government. A relator who brings a successful qui tam lawsuit can receive 15 to 30 percent of the damages the government recovers from the defendants, which damages are trebled under the False Claims Act. Because of these financial inducements offered to plaintiffs, qui tam actions have increased significantly in recent years, causing greater numbers of healthcare companies to incur the costs of having to defend false claims actions, many of which are spurious and without merit. In addition, meritorious false claims actions could result in fines, or debarment from the Medicare, Medicaid, or other state or federal healthcare programs. If we are subject to liability under a qui tam or other actions, our business, financial condition, cash flows, or results of operations could be adversely affected. Even if we are successful in defending qui tam actions against us, the fact that these actions were filed against us, even if ultimately determined to be without merit, could result in expensive defense costs, and also could have an adverse impact on our reputation and our ability to obtain regulatory approval for acquisitions that we may pursue.
RISKS RELATED TO OUR BUSINESS
The May 2020 contract award to our Kentucky Medicaid plan, and its acquisition of Passport, is the subject of a legal challenge.
On September 4, 2020, Anthem Kentucky Managed Care Plan, Inc. brought an action in Franklin County Circuit Court against the Kentucky Finance and Administration Cabinet, the Kentucky Cabinet for Health and Family Services, and all of the five winning bidder health plans, including our Kentucky health plan. This matter remains subject to additional legal and appellate proceedings, and no assurances can be given regarding the ultimate outcome. Under the Court’s June 16, 2021 final Order, our Kentucky health plan will continue to operate for the foreseeable future under its current Medicaid contract and provide care to Kentucky Medicaid members. In the event the contract award to our Kentucky health plan or the novation of the Passport Medicaid contract is overturned, the business and revenue of our Kentucky health plan may be materially and adversely affected.
If the responsive bids of our health plans for new or renewed Medicaid contracts are not successful, or if our government contracts are terminated or are not renewed on favorable terms, our premium revenues could be materially reduced and our operating results could be negatively impacted.
We currently derive our premium revenues from health plans that operate in 18 states. Our consolidated Medicaid premium revenue constituted 76% of our total premium revenue in the year ended December 31, 2021. Measured by Medicaid premium revenue by health plan, our top four health plans were in California, Ohio, Texas, and
Molina Healthcare, Inc. 2021 Form 10-K | 22
Washington, with aggregate Medicaid premium revenue of $10.4 billion, or approximately 51% of consolidated Medicaid premium revenue, in the year ended December 31, 2021. If we are unable to continue to operate in any of our existing jurisdictions, or if our current operations in those jurisdictions or any portions of those jurisdictions are significantly curtailed or terminated entirely, our revenues could decrease materially.
Many of our government contracts are effective only for a fixed period of time and will only be extended for an additional period of time if the contracting entity elects to do so. For example, our contract in California is expected to be subject to re-procurement in February 2022, and our STAR+PLUS and STAR/CHIP contracts in Texas are expected to be subject to re-procurement in early 2022 and late 2022, respectively. When our government contracts expire, they may be opened for bidding by competing health plans, and there is no guarantee that the contracts will be renewed or extended. Even if our contracts are renewed or extended, there can be no assurance that they will be renewed or extended on the same terms or without a reduction in the applicable service areas.
Even if our responsive bids are successful, the bids may be based upon assumptions regarding enrollment, utilization, medical costs, or other factors which could result in the contract being less profitable than we had expected or could result in a net loss. Furthermore, our contracts contain certain provisions regarding, among other things, eligibility, enrollment and dis-enrollment processes for covered services, eligible providers, periodic financial and information reporting, quality assurance and timeliness of claims payment, and are subject to cancellation if we fail to perform in accordance with the standards set by regulatory agencies.
We are subject to risks associated with outsourcing services and functions to third parties.
We contract with third party vendors and service providers who provide services to us and our subsidiaries or to whom we delegate selected functions. Some of these third parties have direct access to our systems. Our arrangements with third party vendors and service providers may make our operations vulnerable if those third parties fail to satisfy their obligations to us, including their obligations to maintain and protect the security and confidentiality of our information and data or the information and data relating to our members or customers. We are also at risk of a data security incident involving a vendor or third party, which could result in a breakdown of such third party’s data protection processes or cyber-attackers gaining access to our infrastructure through the third party. To the extent that a vendor or third party suffers a data security incident that compromises its operations, we could incur significant costs and possible service interruption. Any contractual remedies and/or indemnification obligations we may have for vendor or service provider failures or incidents may not be adequate to fully compensate us for any losses suffered as a result of any vendor’s failure to satisfy its obligations to us or under applicable law. Violations of, or noncompliance with, laws and/or regulations governing our business or noncompliance with contract terms by third party vendors and service providers could increase our exposure to liability to our members, providers, or other third parties, or could result in sanctions and/or fines from the regulators that oversee our business. In turn, this could increase the costs associated with the operation of our business or have an adverse impact on our business and reputation. Moreover, if these vendor and service provider relationships were terminated for any reason, we may not be able to find alternative partners in a timely manner or on acceptable financial terms. This may incur significant costs and/or experience significant disruption to our operations in connection with any such vendor or service provider transition. As a result, we may not be able to meet the full demands of our members or customers and, in turn, our business, financial condition, and results of operations may be harmed.
If we sustain a cyber-attack or suffer data privacy or security breaches that disrupt our information systems or operations, or result in the dissemination of sensitive personal or confidential information, we could suffer increased costs, exposure to significant liability, reputational harm, loss of business, and other serious negative consequences.
As part of our normal operations, we routinely collect, process, store, and transmit large amounts of data, including sensitive personal information as well as proprietary or confidential information relating to our business or third parties. To ensure information security, we have implemented controls designed to protect the confidentiality, integrity and availability of this data and the systems that store and transmit such data. However, our information technology systems and safety control systems are subject to a growing number of threats from computer programmers, hackers, and other adversaries that may be able to penetrate our network security and misappropriate our confidential information or that of third parties, create system disruptions, or cause damage, security issues, or shutdowns. They also may be able to develop and deploy viruses, worms, and other malicious software programs that attack our systems or otherwise exploit security vulnerabilities. As a result of the COVID-19 pandemic, we may face increased cybersecurity risks due to our reliance on internet technology and the number of our employees who are working remotely, which may create additional opportunities for cybercriminals to exploit vulnerabilities. Because the techniques used to circumvent, gain access to, or sabotage security systems can be highly sophisticated and change frequently, they often are not recognized until launched against a target, and may originate from less regulated and remote areas around the world. We may be unable to anticipate these techniques
Molina Healthcare, Inc. 2021 Form 10-K | 23
or implement adequate preventive measures, resulting in potential data loss and damage to our systems. Our systems are also subject to compromise from internal threats such as improper action by employees, including malicious insiders, or by vendors, counterparties, and other third parties with otherwise legitimate access to our systems. Our policies, employee training (including phishing prevention training), procedures and technical safeguards may not prevent all improper access to our network or proprietary or confidential information by employees, vendors, counterparties, or other third parties. Our facilities may also be vulnerable to security incidents or security attacks, acts of vandalism or theft, misplaced or lost data, human errors, or other similar events that could negatively affect our systems and our and our members’ data.
Moreover, we face the ongoing challenge of managing access controls in a complex environment. The process of enhancing our protective measures can itself create a risk of systems disruptions and security issues. Given the breadth of our operations and the increasing sophistication of cyberattacks, a particular incident could occur and persist for an extended period of time before being detected. The extent of a particular cyberattack and the steps that we may need to take to investigate the attack may take a significant amount of time before such an investigation could be completed and full and reliable information about the incident is known. During such time, the extent of any harm or how best to remediate it might not be known, which could further increase the risks, costs, and consequences of a data security incident. In addition, our systems must be routinely updated, patched, and upgraded to protect against known vulnerabilities. The volume of new software vulnerabilities has increased substantially, as has the importance of patches and other remedial measures. In addition to remediating newly identified vulnerabilities, previously identified vulnerabilities must also be updated. We are at risk that cyber attackers exploit these known vulnerabilities before they have been addressed. The complexity of our systems and platforms, the increased frequency at which vendors are issuing security patches to their products, our need to test patches, and in some instances, coordinate with third-parties before they can be deployed, all could further increase our risks.
Where doing so is necessary in order to conduct our business, we also provide sensitive personal member information, as well as proprietary or confidential information relating to our business, to our third-party service providers. Although we obtain assurances from those third parties that they have systems and processes in place to protect such data, and that they will take steps to assure the protection of such data by other third parties, those third-party service providers may also be subject to data intrusion or data breach. Any compromise of the confidential data of our members, employees, or business, or the failure to prevent or mitigate the loss of or damage to this data through breach, could result in operational, reputational, competitive, or other business harm, as well as financial costs and regulatory action. The Company maintains cybersecurity insurance in the event of an information security or cyber incident. However, the coverage may not be sufficient to cover all financial losses.
We may be unable to successfully integrate our acquisitions or realize the anticipated benefits of such acquisitions.
Our growth strategy includes the pursuit of targeted inorganic growth opportunities that we believe will provide a strategic fit, leverage operational synergies, and lead to incremental earnings accretion. For example, on December 31, 2020, we closed on our acquisition of the Magellan Complete Care line of business of Magellan Health, Inc., in the fourth quarter of 2021, we closed on our acquisition of Affinity Health Plan, Inc. in New York and in January 2022, we closed on our acquisition of the Medicaid assets of Cigna Corporation in Texas. In October 2021, we entered into a definitive agreement to acquire the Medicaid Managed Long Term Care business of AgeWell New York. Subject to the receipt of applicable federal and state regulatory approvals and the satisfaction of customary closing conditions, the closing of this transaction is expected to occur by the third quarter of 2022. The integration of acquired businesses with our existing business is a complex, costly and time-consuming process. The success of acquisitions we make will depend, in part, on our ability to successfully combine our existing business with such acquired businesses and realize the anticipated benefits, including synergies, cost savings, growth in earnings, innovation, and operational efficiencies, from the combinations. If we are unable to achieve these objectives within the anticipated time frame, or at all, the anticipated benefits may not be realized fully or at all, or may take longer to realize than expected.
Our acquisitions and the related integration activities involve a number of risks, including the following:
•The transition services that a seller may have agreed to provide following the closing, such as those Magellan Health, Inc. is currently providing in connection with the Magellan Complete Care transaction, may not be provided in a timely or efficient manner, or certain necessary transition services may not be provided at all;
•Unforeseen expenses or delays associated with the acquisition and/or integration;
•The assumptions underlying our expectations regarding the integration process or the expected benefits to be achieved from an acquisition may prove to be incorrect;
Molina Healthcare, Inc. 2021 Form 10-K | 24
•Maintaining employee morale and retaining key management and other employees;
•Difficulties retaining the business and operational relationships of the acquired business, and attracting new business and operational relationships;
•Unanticipated attrition in the membership of the acquired business pending the completion of the proposed transaction or after the closing of the transaction;
•Unanticipated difficulties or costs in integrating information technology, communications and other systems, consolidating corporate and administrative infrastructures, and eliminating duplicative operations;
•Attention to integration activities may divert management’s attention from ongoing business concerns, which could result in performance shortfalls;
•Successfully addressing the challenges inherent in managing a larger company and coordinating geographically separate organizations; and
•Delays in obtaining, or inability to obtain, necessary state or federal regulatory approvals, or such approvals may impose conditions that were not anticipated.
Many of these factors are outside of our control and any one of them could result in delays, increased costs, decreases in the amount of expected revenues, and diversion of management's time and energy, which could have a material adverse effect on our business, financial condition, cash flows or results of operations. There can be no assurances that we will be successful in managing our expanded operations as a result of acquisitions or that we will realize the expected growth in earnings, operating efficiencies, cost savings, or other benefits.
If we lose contracts that constitute a significant amount of our premium revenue, we will lose the administrative cost efficiencies or cost leverage that is inherent in a larger revenue base. In such circumstances, we may not be able to reduce fixed costs proportionally with our lower revenue, and the financial impact of lost contracts may exceed the net income ascribed to those contracts.
We currently spread the cost of centralized services over a large revenue base. Many of our administrative costs are fixed in nature, and will be incurred at the same level regardless of the size of our revenue base. If we lose contracts that constitute a significant amount of our revenue, we may not be able to reduce the expense of centralized services in a manner that is proportional to that loss of revenue. In such circumstances, not only will our total dollar margins decline, but our percentage margins, measured as a percentage of revenue, will also decline. This loss of cost efficiency or cost leverage, and the resulting stranded administrative costs, could have a material and adverse impact on our business, financial condition, cash flows, or results of operations.
Our health plans operate with very low profit margins, and small changes in operating performance or slight changes to our accounting estimates will have a disproportionate impact on our reported net income.
A substantial portion of our premium revenue is subject to contract provisions pertaining to medical cost expenditure floors and corridors, administrative cost and profit ceilings, premium stabilization programs, and cost-plus and performance-based reimbursement programs. Many of these contract provisions are complex, or are poorly or ambiguously drafted, and thus are subject to differing interpretations by us and the relevant government agency with whom we contract. If the applicable government agency disagrees with our interpretation or implementation of a particular contract provision, we could be required to adjust the amount of our obligation under that provision. Any such adjustment could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
In addition, many of our contracts contain provisions pertaining to at-risk premiums that require us to meet certain quality performance measures to earn all of our contract revenues. If we are unsuccessful in achieving the stated performance measure, we will be unable to recognize the revenue associated with that measure, which could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
Our Medicaid premium revenues could be adversely impacted by retroactive adjustments or states’ delays in processing rate changes.
The complexity of some of our Medicaid contract provisions, imprecise language in those contracts, the desire of state Medicaid agencies in some circumstances to retroactively adjust for the acuity of the medical needs of our members, and state delays in processing rate changes, can create uncertainty around the amount of revenue we should recognize. Any circumstance such as those described above could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
Molina Healthcare, Inc. 2021 Form 10-K | 25
If, in the interest of long-term profitability, we decide to exit certain state contractual arrangements, make changes to our provider networks, or make changes to our administrative infrastructure, we may incur disruptions to our business that could in the short term materially reduce our premium revenues and our net income.
Decisions that we make with regard to retaining or exiting our portfolio of state or federal contracts, and changes to the manner in which we serve the members of those contracts, could generate substantial expenses associated with the run out of existing operations and the restructuring of those operations that remain. Such expenses could include, but would not be limited to, goodwill and intangible asset impairment charges, restructuring costs, additional medical costs incurred due to the inability to leverage long-term relationships with medical providers, and costs incurred to finish the run out of businesses that have ceased to generate revenue, all of which could materially reduce our premium revenues and net income. For example, following our exit from Puerto Rico in October 2020, significant accounts receivable under our Puerto Rico Medicaid contract remained, which we ultimately may never recover.
A failure to accurately estimate incurred but not paid medical care costs may negatively impact our results of operations.
Because of the lag in time between when medical services are actually rendered by our providers and when we receive, process, and pay a claim for those medical services, we must continually estimate our medical claims liability at particular points in time and establish claims reserves related to such estimates. Our estimated reserves for such incurred but not paid, or IBNP, medical care costs are based on numerous assumptions. We estimate our medical claims liabilities using actuarial methods based on historical data adjusted for claims receipt and payment experience (and variations in that experience), changes in membership, provider billing practices, healthcare service utilization trends, cost trends, product mix, seasonality, prior authorization of medical services, benefit changes, known incidence of disease, including COVID-19, or increased incidence of illness such as the flu, provider contract changes, changes to Medicaid fee schedules, and the incidence of high dollar or catastrophic claims. Our ability to accurately estimate claims for our newer lines of business or populations is negatively impacted by the more limited experience we have had with those newer lines of business or populations.
The IBNP estimation methods we use and the resulting reserves that we establish are reviewed and updated, and adjustments, if deemed necessary, are reflected in the current period. Given the numerous uncertainties inherent in such estimates, our actual claims liabilities for a particular quarter or other period could differ significantly from the amounts estimated and reserved for that quarter or period. Our actual claims liabilities have varied and will continue to vary from our estimates, particularly in times of significant changes in utilization, medical cost trends, and populations and markets served.
If our actual liability for claims payments is higher than previously estimated, our earnings in any particular quarter or annual period could be negatively affected. Our estimates of IBNP may be inadequate in the future, which would negatively affect our results of operations for the relevant time period. Furthermore, if we are unable to accurately estimate IBNP, our ability to take timely corrective actions may be limited, further exacerbating the extent of the negative impact on our results.
If we fail to accurately predict and effectively manage our medical care costs, our operating results could be materially and adversely affected.
Our profitability depends to a significant degree on our ability to accurately predict and effectively manage our medical care costs. Historically, our medical care ratio, meaning our medical care costs as a percentage of our premium revenue, has fluctuated substantially, and has varied across our health plans. Because the premium payments we receive are generally fixed in advance and we operate with a narrow profit margin, relatively small changes in our medical care ratio can create significant changes in our overall financial results. For example, if our overall medical care ratio of 88.3% for the year ended December 31, 2021, had been one percentage point higher, or 89.3%, our net income per diluted share for the year ended December 31, 2021 would have been approximately $7.76 rather than our actual net income per diluted share of $11.25, a difference of $3.49.
Many factors may affect our medical care costs, including:
•the level of utilization of healthcare services;
•the impact of the COVID-19 pandemic;
•changes in the underlying risk acuity of our membership;
•unexpected patterns in the annual flu season;
•increases in hospital costs;
Molina Healthcare, Inc. 2021 Form 10-K | 26
•increased incidences or acuity of high dollar claims related to catastrophic illnesses or medical conditions for which we do not have adequate reinsurance coverage;
•increased maternity costs;
•changes in state eligibility certification methodologies;
•relatively low levels of hospital and specialty provider competition in certain geographic areas;
•increases in the cost of pharmaceutical products and services;
•changes in healthcare regulations and practices;
•epidemics;
•new medical technologies; and
•other various external factors.
Many of these factors are beyond our control. The inability to forecast and manage our medical care costs or to establish and maintain a satisfactory medical care ratio, either with respect to a particular health plan or across the consolidated entity, could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
If we are unable to deliver quality care, and maintain good relations with the physicians, hospitals, and other providers with whom we contract, or if we are unable to enter into cost-effective contracts with such providers, our profitability could be adversely affected.
We contract with physicians, hospitals, and other providers as a means to ensure access to healthcare services for our members, to manage medical care costs and utilization, and to better monitor the quality of care being delivered. We compete with other health plans to contract with these providers. We believe providers select plans in which they participate based on criteria including reimbursement rates, timeliness and accuracy of claims payment, potential to deliver new patient volume and/or retain existing patients, effectiveness of resolution of calls and complaints, and other factors. There can be no assurance that we will be able to successfully attract and retain providers to maintain a competitive network in the geographic areas we serve. In addition, in any particular market, providers could refuse to contract with us, demand higher payments, or take other actions which could result in higher medical care costs, disruption to provider access for current members, a decline in our growth rate, or difficulty in meeting regulatory or accreditation requirements.
The Medicaid program generally pays doctors and hospitals at levels well below those of Medicare and private insurance. Large numbers of doctors, therefore, do not accept Medicaid patients. In the face of fiscal pressures, some states may reduce rates paid to providers, which may further discourage participation in the Medicaid program.
In some markets, certain providers, particularly hospitals and some specialists, may have significant market positions or even monopolies. If these providers refuse to contract with us or utilize their market position to negotiate favorable contracts which are disadvantageous to us, our profitability in those areas could be adversely affected.
Some providers that render services to our members are not contracted with our health plans. In those cases, there is no pre-established understanding between the provider and our health plan about the amount of compensation that is due to the provider. In some states, the amount of compensation is defined by law or regulation, but in most instances it is either not defined or it is established by a standard that is not clearly translatable into dollars. In such instances, providers may claim they are underpaid for their services and may either litigate or arbitrate their dispute with our health plan. The uncertainty of the amount to pay to such providers and the possibility of subsequent adjustment of the payment or litigation with the provider that results in an adverse decision could adversely affect our business, financial condition, cash flows, or results of operations.
We rely on the accuracy of eligibility lists provided by state governments. Inaccuracies in those lists would negatively affect our results of operations.
Premium payments to our health plans are based upon eligibility lists produced by state governments. From time to time, states require us to reimburse them for premiums paid to us based on an eligibility list that a state later discovers contains individuals who are not in fact eligible for a government sponsored program or are eligible for a different premium category or a different program. Alternatively, a state could fail to pay us for members for whom we are entitled to payment. Our results of operations would be adversely affected as a result of such reimbursement to the state if we make or have made related payments to providers and are unable to recoup such payments from the providers. Further, when a state implements new programs to determine eligibility, establishes new processes to assign or enroll eligible members into health plans, or chooses new subcontractors, there is an increased potential for an unanticipated impact on the overall number of members assigned to managed care health plans. Whenever a state effects an eligibility redetermination for any reason, there is generally an associated
Molina Healthcare, Inc. 2021 Form 10-K | 27
reduction in Medicaid membership, which could have an adverse effect on our premium revenues and results of operations.
The insolvency of a delegated provider could obligate us to pay its referral claims, which could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
Many of our primary care physicians and a small portion of our specialists and hospitals are paid on a capitated basis. Under capitation arrangements, we pay a fixed amount per member per month to the provider without regard to the frequency, extent, or nature of the medical services actually furnished. Due to insolvency or other circumstances, such providers may be unable or unwilling to pay claims they have incurred with third parties in connection with referral services provided to our members. The inability or unwillingness of delegated providers to pay referral claims presents us with both immediate financial risk and potential disruption to member care, as well as potential loss of members. Depending on states’ laws, we may be held liable for such unpaid referral claims even though the delegated provider has contractually assumed such risk. Additionally, competitive pressures or practical regulatory considerations may force us to pay such claims even when we have no legal obligation to do so; or we have already paid claims to a delegated provider and such payments cannot be recouped when the delegated provider becomes insolvent. Liabilities incurred or losses suffered as a result of provider insolvency or other circumstances could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
Receipt of inadequate or significantly delayed premiums could negatively affect our business, financial condition, cash flows, or results of operations.
Our premium revenues consist of fixed monthly payments per member, and supplemental payments for other services such as maternity deliveries. These premiums are fixed by contract, and we are obligated during the contract periods to provide healthcare services as established by the state governments. We use a large portion of our revenues to pay the costs of healthcare services delivered to our members. If premiums do not increase when expenses related to healthcare services rise, our medical margins will be compressed, and our earnings will be negatively affected. A state could increase hospital or other provider rates without making a commensurate increase in the rates paid to us, could lower our rates without making a commensurate reduction in the rates paid to hospitals or other providers, or could delay the processing of rate changes. In addition, if the actuarial assumptions made by a state in implementing a rate or benefit change are incorrect or are at variance with the particular utilization patterns of the members of one or more of our health plans, our medical margins could be reduced. Any of these rate adjustments in one or more of the states in which we operate could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
If a state fails to renew its federal waiver application for mandated Medicaid enrollment into managed care or such application is denied, our membership in that state will likely decrease.
States may only mandate Medicaid enrollment into managed care under federal waivers or demonstrations. Waivers and programs under demonstrations are approved for two- to five-year periods and can be renewed on an ongoing basis if the state applies and the waiver request is approved or renewed by CMS. We have no control over this renewal process. If a state in which we operate does not renew its mandated program or the federal government denies the state’s application for renewal, our business would suffer as a result of a likely decrease in membership.
Failure to attain profitability in any newly acquired health plans or new start-up operations could negatively affect our results of operations.
Start-up costs associated with a new business can be substantial. For example, to obtain a certificate of authority to operate as a health maintenance organization in most jurisdictions, we must first establish a provider network, have infrastructure and required systems in place, and demonstrate our ability to obtain a state contract and process claims. Often, we are also required to contribute significant capital to fund mandated net worth requirements, performance bonds or escrows, or contingency guaranties. If we are unsuccessful in obtaining the certificate of authority, winning the bid to provide services, or attracting members in sufficient numbers to cover our costs, the new business could fail.
The expenses associated with starting up a health plan in a new jurisdiction, expanding a health plan in an existing jurisdiction, or acquiring a new health plan, could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
Molina Healthcare, Inc. 2021 Form 10-K | 28
Our business depends on our information and medical management systems, and our inability to effectively integrate, manage, update, and keep secure our information and medical management systems could disrupt our operations.
Our business is dependent on effective and secure information systems that assist us in processing provider claims, monitoring utilization and other cost factors, supporting our medical management techniques, providing data to our regulators, and implementing our data security measures. Our members and providers also depend upon our information systems for enrollment, premium processing, primary care and specialist physician roster access, membership verifications, claims status, provider payments, and other information. If we experience a reduction in the performance, reliability, or availability of our information and medical management systems, our operations, ability to pay claims, ability to produce timely and accurate reports, and ability to maintain proper security measures could be adversely affected.
We have partnered with third parties to support our information technology systems. This makes our operations vulnerable to adverse effects if such third parties fail to perform adequately. For example, in February 2019, we entered into a master services agreement with a third party vendor who manages certain of our information technology infrastructure services including, among other things, our information technology operations, end-user services, and data centers. If any licensor or vendor of any technology which is integral to our operations were to become insolvent or otherwise fail to support the technology sufficiently, our operations could be negatively affected. Additionally, our operations are vulnerable to adverse effects if such third parties are unable to perform due to forces outside of their control, such as a natural disaster or serious weather event. For example, in 2021, our third party call center, located in the province of Cebu in the Philippines, suffered significant disruptions as a result of the destruction caused by Super Typhoon Rai.
Our encounter data may be inaccurate or incomplete, which could have a material adverse effect on our results of operations, financial condition, cash flows and ability to bid for, and continue to participate in, certain programs.
Our contracts require the submission of complete and correct encounter data. The accurate and timely reporting of encounter data is increasingly important to the success of our programs because more states are using encounter data to determine compliance with performance standards and to set premium rates. We have been, and continue to be, exposed to operating sanctions and financial fines and penalties for noncompliance. In some instances, our government clients have established retroactive requirements for the encounter data we must submit. There also may be periods of time in which we are unable to meet existing requirements. In either case, it may be prohibitively expensive or impossible for us to collect or reconstruct this historical data.
We have experienced challenges in obtaining complete and accurate encounter data, due to difficulties with providers and third-party vendors submitting claims in a timely fashion in the proper format, and with state agencies in coordinating such submissions. As states increase their reliance on encounter data, these difficulties could adversely affect the premium rates we receive and how membership is assigned to us and subject us to financial penalties, which could have a material adverse effect on our business, financial condition, cash flows, or results of operations, and on our ability to bid for, and continue to participate in, certain programs.
An impairment charge with respect to our recorded goodwill, or our finite-lived intangible assets, could have a material impact on our financial results.
As of December 31, 2021, the carrying amount of goodwill was $982 million, and intangible assets, net, were $270 million.
Goodwill represents the excess of the purchase consideration over the fair value of net assets acquired in business combinations. Goodwill is not amortized but is tested for impairment on an annual basis and more frequently if impairment indicators are present. Impairment indicators may include experienced or expected operating cash-flow deterioration or losses, significant losses of membership, loss of state funding, loss of state contracts, and other factors. Goodwill is impaired if the carrying amount of the reporting unit exceeds its estimated fair value. This excess is recorded as an impairment loss and adjusted if necessary for the impact of tax-deductible goodwill. The loss recognized may not exceed the total goodwill allocated to the reporting unit.
An event could occur that would cause us to revise our estimates and assumptions used in analyzing the value of our goodwill, and intangible assets, net. For example, if the responsive bid of one or more of our health plans is not successful, we will lose a contract in the applicable state or states and may be an indicator of impairment. If an event or events occur that would cause us to revise our estimates and assumptions used in analyzing the value of our goodwill and other intangible assets, such revision could result in a non-cash impairment charge that could have a material impact on our results of operations in the period in which the impairment occurs.
Molina Healthcare, Inc. 2021 Form 10-K | 29
GENERAL RISK FACTORS
We are dependent on the leadership of our chief executive officer and other executive officers and key employees.
The success of our business and the ability to execute our strategy are highly dependent on the efforts of Mr. Zubretsky, our chief executive officer, and our other key executive officers and employees. The loss of their leadership, expertise, and experience could negatively impact our operations. Our ability to replace them or any other key employee may be difficult and may take an extended period of time because of the limited number of individuals in the healthcare industry who have the breadth and depth of skills and experience necessary to operate and lead a business such as ours. Competition to hire from this limited pool is intense, and we may be unable to hire, train, retain, or motivate these personnel. If we are unsuccessful in recruiting, retaining, managing, and motivating such personnel, our business, financial condition, cash flows, or results of operations could be adversely affected.
We face claims related to litigation which could result in substantial monetary damages.
We are subject to a variety of legal actions, including provider claims, employment related disputes, healthcare regulatory law-based litigation and enforcement actions, breach of contract actions, qui tam or False Claims Act actions, and securities class actions. If we incur liability materially in excess of the amount for which we have insurance coverage, our profitability would suffer. Even if any claims brought against us are unsuccessful or without merit, we may have to defend ourselves against such claims. The defense of any such actions may be time-consuming and costly, and may distract our management’s attention. Such legal actions could have a material adverse effect on our business, financial condition, results of operations, or cash flows.
Because our corporate headquarters are located in Southern California, our business operations may be significantly disrupted as a result of a major earthquake or wildfire.
Our corporate headquarters are located in Long Beach, California. In addition, some of our health plans’ claims are processed in Long Beach, California. Southern California is exposed to a statistically greater risk of a major earthquake and wildfires than most other parts of the United States. If a major earthquake or wildfire were to strike Southern California, our corporate functions and claims processing could be significantly impaired for a substantial period of time. If there is a major Southern California earthquake or wildfire, there can be no assurances that our disaster recovery plan will be successful or that the business operations of our health plans, including those that are remote from any such event, would not be substantially impacted.
Failure to maintain effective internal controls over financial reporting could have a material adverse effect on our business, operating results, and stock price, and could subject us to sanctions by regulatory authorities.
A material weakness is a deficiency, or a combination of deficiencies, in internal control over financial reporting, such that there is a reasonable possibility that a material misstatement of the annual or interim financial statements will not be prevented or detected on a timely basis. We have identified material weaknesses in our internal control over financial reporting in the past, which have subsequently been remediated. If additional material weaknesses in our internal control over financial reporting are discovered or occur in the future, our consolidated financial statements may contain material misstatements and we could be required to restate our financial results.
Molina Healthcare, Inc. 2021 Form 10-K | 30
PROPERTIES
We own and lease certain real properties to support the business operations of our reportable segments. While we believe our current and anticipated facilities are adequate to meet our operational needs in the near term, we continually evaluate the adequacy of our properties for our anticipated future needs.
LEGAL PROCEEDINGS
Kentucky RFP. On September 4, 2020, Anthem Kentucky Managed Care Plan, Inc. brought an action in Franklin County Circuit Court against the Kentucky Finance and Administration Cabinet, the Kentucky Cabinet for Health and Family Services, and all of the five winning bidder health plans, including our Kentucky health plan. This matter remains subject to additional legal and appellate proceedings, and no assurances can be given regarding the ultimate outcome. Under the Court’s June 16, 2021 final Order, our Kentucky health plan will continue to operate for the foreseeable future under its current Medicaid contract and provide care to Kentucky Medicaid members.
Puerto Rico. On August 13, 2021, Molina Healthcare of Puerto, Inc. (“MHPR”) filed a complaint asserting, among other claims, breach of contract against Puerto Rico Health Insurance Administration (“ASES”). On September 13, 2021, in addition to filing its answer to MHPR’s complaint, ASES filed a counterclaim and a third-party complaint against MHPR and the Company. The counterclaim alleges that MHPR and the Company breached contractual obligations by failing to pay providers and, in addition to damages, seeks various equitable remedies. On October 8, 2021, MHPR filed its reply to the counterclaim, denying all the allegations, and on November 1, 2021, the Company filed its answer to the third-party complaint. On December 3, 2021, MHPR filed a request for disbursement of illegally withheld funds, and ASES filed its opposition. At a status hearing on January 19, 2022, the Company and ASES both argued MHPR’s request for disbursement. The court has not ruled. This matter is in its early stages, and no prediction can be made as to the outcome. No gain or loss is probable and reasonably estimable with regard to either MHPR’s complaint or the counterclaim of ASES.
Refer to the Notes to Consolidated Financial Statements, Note 15, “Commitments and Contingencies—Legal Proceedings,” for further information.
MARKET FOR REGISTRANT’S COMMON EQUITY, RELATED STOCKHOLDER MATTERS AND ISSUER PURCHASES OF EQUITY SECURITIES
STOCK REPURCHASE PROGRAMS
Purchases of common stock made by us, or on our behalf during the quarter ended December 31, 2021, including shares withheld by us to satisfy our employees’ income tax obligations, are set forth below:
| | | | | | | | | | | | | | | | | | | | | | | |
| Total Number of Shares Purchased (1) | | Average Price Paid per
Share | | Total Number of Shares Purchased as Part of Publicly Announced Plans or Programs (2) | | Approximate Dollar Value of Shares That May Yet Be Purchased Under the Plans or Programs (2) |
| October 1 — October 31 | 2,000 | | | $ | 273.61 | | | — | | | $ | 500,000,000 | |
| November 1 — November 30 | — | | | $ | — | | | — | | | $ | 500,000,000 | |
| December 1 — December 31 | — | | | $ | — | | | — | | | $ | 500,000,000 | |
| 2,000 | | | $ | 273.61 | | | — | | | |
_______________________
(1)During the three months ended December 31, 2021, we withheld approximately 2,000 shares of common stock to settle employee income tax obligations, for releases of awards granted under the Molina Healthcare, Inc. 2019 Equity Incentive Plan. For further information refer to Notes to Consolidated Financial Statements, Note 13, “Stockholders' Equity.”
(2)For further information on our stock repurchase programs, refer to Notes to Consolidated Financial Statements, Note 13, “Stockholders' Equity.”
Molina Healthcare, Inc. 2021 Form 10-K | 31
STOCK PERFORMANCE GRAPH
The following graph and related discussion are being furnished solely to accompany this Annual Report on Form 10-K pursuant to Item 201(e) of Regulation S-K and shall not be deemed to be “soliciting materials” or to be “filed” with the U.S. Securities and Exchange Commission (“SEC”) (other than as provided in Item 201) nor shall this information be incorporated by reference into any future filing under the Securities Act or the Exchange Act, whether made before or after the date hereof and irrespective of any general incorporation language contained therein, except to the extent that we specifically incorporate it by reference into a filing.
The following line graph compares the percentage change in the cumulative total return on our common stock against the cumulative total return of the Standard & Poor’s Corporation Composite 500 Index (the “S&P 500”) and a peer group index for the five-year period from December 31, 2016 to December 31, 2021. The comparison assumes $100 was invested on December 31, 2016, in our common stock and in each of the foregoing indices and assumes reinvestment of dividends. The stock performance shown on the graph below represents historical stock performance and is not necessarily indicative of future stock price performance.
The peer group index consists of Acadia Healthcare Company, Inc. (ACHC), Anthem, Inc. (ANTM), Centene Corporation (CNC), Cigna Corporation (CI), Community Health Systems, Inc. (CYH), HCA Healthcare, Inc. (HCA), Humana, Inc. (HUM), Laboratory Corporation of America Holdings (LH), Magellan Health, Inc. (MGLN), Quest Diagnostics Incorporated (DGX), Tenet Healthcare Corporation (THC) and Universal Health Services, Inc. (UHS).
Molina Healthcare, Inc. 2021 Form 10-K | 32
STOCK TRADING SYMBOL AND DIVIDENDS
Our common stock is listed on the New York Stock Exchange under the trading symbol “MOH.” As of February 11, 2022, there were 13 registered holders of record of our common stock, including Cede & Co. To date we have not paid cash dividends on our common stock. We currently intend to retain any future earnings to fund our projected business operations. However, we intend to periodically evaluate our cash position to determine whether to pay a cash dividend in the future. Our ability to pay dividends is partially dependent on, among other things, our receipt of cash dividends from our regulated subsidiaries. The ability of our regulated subsidiaries to pay dividends to us is limited by the state departments of insurance in the states in which we operate or may operate, as well as requirements of the government-sponsored health programs in which we participate. Additionally, the indentures governing our outstanding senior notes and credit agreement contain various covenants that limit our ability to pay dividends on our common stock. Any future determination to pay dividends will be at the discretion of our board of directors and will depend upon, among other factors, our results of operations, financial condition, capital requirements and contractual and regulatory restrictions. For more information regarding restrictions on the ability of our regulated subsidiaries to pay dividends to us, please see the Notes to Consolidated Financial Statements, Note 15, “Commitments and Contingencies—Regulatory Capital Requirements and Dividend Restrictions.”
Molina Healthcare, Inc. 2021 Form 10-K | 33
MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS (“MD&A”)
Management’s discussion and analysis of financial condition and results of operations as of and for the years ended December 31, 2021 and 2020, are presented in the sections that follow. Our MD&A as of and for the year ended December 31, 2019, may be found in our 2020 Annual Report on Form 10-K, which prior disclosure is incorporated by reference herein.
OVERVIEW
Molina Healthcare, Inc., a FORTUNE 500 company (currently ranked 155), provides managed healthcare services under the Medicaid and Medicare programs, and through the state insurance marketplaces (the “Marketplace”). We served approximately 5.2 million members as of December 31, 2021, located across 18 states.
2021 HIGHLIGHTS
Highlights of our 2021 results included the following:
•Net income for 2021 was $659 million, or $11.25 per diluted share, compared to $673 million, or $11.23 per diluted share, in 2020;
•Total revenue of $27.8 billion, which increased 43% compared to 2020;
•Premium revenue of $26.9 billion, which increased 47% compared to 2020;
•Consolidated medical care ratio (“MCR”) of 88.3%, compared to 86.5% in 2020;
•Membership, increased 1.2 million members year-over-year to 5.2 million at December 31, 2021;
•General and administrative expense ratio (“G&A ratio”) improved to 7.4%, compared to 7.6% in 2020; and
•After-tax margin of 2.4%.
The net effect of COVID decreased 2021 net income per diluted share by $3.50 per diluted share and decreased 2020 net income per diluted share by $2.30. The net effect of COVID impacted all three lines of business and increased the 2021 consolidated MCR by approximately 90 basis points, compared to an increase of approximately 50 basis points to the consolidated MCR in 2020. The net effect of COVID reflects COVID-related inpatient costs and COVID-related risk corridors enacted by a number of our state customers beginning in the second quarter of 2020, partially offset by a decrease in medical costs due to COVID-related utilization curtailment.
Growth Initiatives
We have made major strides related to our growth strategy. On October 7, 2021, we signed a definitive agreement to acquire the Medicaid Managed Long Term Care business of AgeWell New York. On October 25, 2021, we closed on the acquisition of Affinity Health Plan in New York. On January 1, 2022, we closed the acquisition of Cigna Corporation’s Texas Medicaid and Medicare-Medicaid Plan contracts, along with certain operating assets. Each of these acquisitions involve financially underperforming health plans, but with stable membership and revenue bases. We believe they provide attractive opportunities for margin improvement, operating leverage and membership growth. Our growth initiatives continue to be anchored by our capital allocation priorities: first, organic growth; second, inorganic growth through accretive acquisitions; and third, programmatically returning excess capital to stockholders.
Molina Healthcare, Inc. 2021 Form 10-K | 34
FINANCIAL RESULTS SUMMARY
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2021 | | 2020 |
| | | |
| (In millions, except per-share amounts) |
| Premium revenue | $ | 26,855 | | | $ | 18,299 | |
| Less: medical care costs | 23,704 | | | 15,820 | |
| Medical margin | 3,151 | | | 2,479 | |
MCR (1) | 88.3 | % | | 86.5 | % |
| | | |
| Other revenues: | | | |
| Premium tax revenue | 787 | | | 649 | |
| Health insurer fees reimbursed | — | | | 271 | |
| Marketplace risk corridor judgment | — | | | 128 | |
| Investment income | 52 | | | 59 | |
| Other revenue | 77 | | | 17 | |
| | | |
| General and administrative expenses | 2,068 | | | 1,480 | |
G&A ratio (2) | 7.4 | % | | 7.6 | % |
| | | |
| Premium tax expenses | 787 | | | 649 | |
| Health insurer fees | — | | | 277 | |
| Depreciation and amortization | 131 | | | 88 | |
| Other | 61 | | | 31 | |
| Operating income | 1,020 | | | 1,078 | |
| Interest expense | 120 | | | 102 | |
| Other expenses (income), net | 25 | | | 15 | |
| Income before income tax expense | 875 | | | 961 | |
| Income tax expense | 216 | | | 288 | |
| Net income | $ | 659 | | | $ | 673 | |
| | | |
| Net income per diluted share | $ | 11.25 | | | $ | 11.23 | |
| | | |
| Diluted weighted average shares outstanding | 58.6 | | | 59.9 | |
| | | |
| Other Key Statistics: | | | |
Ending Membership (4) | 5.2 | | | 4.0 | |
| Effective income tax rate | 24.7 | % | | 30.0 | % |
After-tax margin (3) | 2.4 | % | | 3.5 | % |
__________________
(1)MCR represents medical care costs as a percentage of premium revenue.
(2)G&A ratio represents general and administrative expenses as a percentage of total revenue.
(3)After-tax margin represents net income as a percentage of total revenue.
(4)Approximately 200,000 members, from the Magellan Complete Care acquisition that closed on December 31, 2020, are not included in the totals as of December 31, 2020.
Molina Healthcare, Inc. 2021 Form 10-K | 35
CONSOLIDATED RESULTS
NET INCOME AND OPERATING INCOME
Net income amounted to $659 million, or $11.25 per diluted share in 2021, compared with net income of $673 million, or $11.23 per diluted share, in 2020. We estimate that the net effect of COVID decreased net income by approximately $3.50 per diluted share in 2021. In 2020, the net effect of COVID decreased net income by approximately $2.30 per diluted share.
Operating income was $1,020 million in 2021, compared with $1,078 million in 2020. The decrease in operating income was mainly due to the increase in MCR, reflecting increases in all our segments, and the $128 million Marketplace risk corridor judgment received in 2020, partially offset by the favorable impact of membership growth and higher premium revenues.
Net income per share in 2021 was favorably impacted by the reduction in common shares outstanding as a result of our share repurchase programs in 2020. See further discussion and information in “Liquidity and Financial Condition,” below, and in the Notes to Consolidated Financial Statements, Note 3, “Net Income Per Share.”
PREMIUM REVENUE
Premium revenue increased $8.6 billion, or 47%, in 2021, when compared with 2020. The higher premium revenue mainly reflects growth in membership across all segments in 2021.
Membership increased by 1.2 million compared with December 31, 2020, which mainly reflected the impact of acquisitions that closed in the second half of 2020, including Magellan Complete Care and the Affinity acquisition that closed in the fourth quarter of 2021, and organic increases in the Medicaid and Marketplace segments. The lower impact of COVID-related risk corridors in 2021, that were enacted in several states beginning in the second quarter of 2020 in response to COVID-related utilization curtailment, also contributed to increase in premium revenue.
MEDICAL CARE RATIO
The consolidated MCR in 2021 increased to 88.3%, compared to 86.5% in 2020, and reflects increases in all our segments. The net effect of COVID increased the consolidated MCR by approximately 90 basis points in 2021, and reflects higher COVID inpatient costs, and lower COVID-related utilization curtailment, partially offset by a lower impact of COVID-related risk corridors. The net effect of COVID impacted all our segments, but the year-over-year change was unfavorable for our Medicare and Marketplace segments. In 2020, the net effect of COVID increased our consolidated MCR by approximately 50 basis points.
The prior year reserve development in 2021 was modestly favorable, but its impact on earnings was mostly absorbed by the COVID-related risk corridors.
PREMIUM TAX REVENUE AND EXPENSES
The premium tax ratio decreased to 2.8% in 2021, compared with 3.4% in 2020. The current year ratio decrease was mainly due to the changes in business mix resulting from the Magellan Complete Care and other acquisitions closed in the second half of 2020.
MARKETPLACE RISK CORRIDOR JUDGMENT
In June 2020, the U.S. Court of Federal Claims granted us judgment in the amount of $128 million for 2014, 2015, and 2016 Marketplace risk corridor claims, following a favorable U.S. Supreme Court decision in April 2020 which held section 1342 of the Affordable Care Act obligated the federal government to pay participating insurers the full Marketplace risk corridor amounts calculated by that statute. We received the judgment in October 2020 and, consistent with the timing of the cash receipt, the gain was recognized in our fourth quarter 2020 financial results and reported in “Marketplace risk corridor judgment” in our consolidated statements of income. The judgment did not create additional Minimum MLR rebates.
INVESTMENT INCOME
Investment income decreased to $52 million in 2021, compared with $59 million in 2020. The year-over-year decrease was due to the continued low interest rate environment and a temporarily higher allocation in shorter-term invested assets during the COVID-19 pandemic, which was rescinded effective for the second quarter of 2021.
Molina Healthcare, Inc. 2021 Form 10-K | 36
OTHER REVENUE
Other revenue increased to $77 million in 2021, compared with $17 million in 2020. Beginning in the first quarter of 2021, other revenue includes service revenue associated with the long-term services and supports consultative services we now provide in Wisconsin, as a result of our Magellan Complete Care acquisition.
GENERAL AND ADMINISTRATIVE (“G&A”) EXPENSES
The G&A expense ratio decreased slightly to 7.4% in 2021 compared with 7.6% in 2020. The year over year decrease reflects the benefits of scale produced by our growth and our disciplined cost management, partially offset by appropriate investments to support our business growth and increased acquisition-related expenses.
HEALTH INSURER FEES (“HIF”)
There were no HIF fees incurred or reimbursed in 2021, because the HIF was repealed effective for years after 2020.
DEPRECIATION AND AMORTIZATION
Depreciation and amortization increased to $131 million in 2021, compared with $88 million in 2020. The increase was due primarily to amortization associated with acquisitions completed in the second half of 2020 and 2021.
OTHER OPERATING EXPENSES
Other operating expenses increased to $61 million in the year ended December 31, 2021, compared with $31 million in the year ended December 31, 2020. Beginning in the first quarter of 2021, other operating expenses include service costs associated with the long-term services and supports consultative services we now provide in Wisconsin, as noted above.
INTEREST EXPENSE
Interest expense increased to $120 million in 2021, compared with $102 million in 2020, mainly due to higher levels of average outstanding debt, resulting from the net impact of financing activities in both 2020 and 2021.
OTHER EXPENSES (INCOME), NET
In 2021, we recognized a loss on debt repayment of $25 million in connection with early redemption of our 5.375% Notes. In 2020, we recognized a loss on debt repayment of $15 million, in connection with repayment of our term loan facility and other financing transactions.
INCOME TAXES
Income tax expense amounted to $216 million in 2021, or 24.7% of pretax income, compared with income tax expense of $288 million in 2020, or 30.0% of the pretax income. The effective tax rate is lower in 2021 mainly because the nondeductible HIF was repealed for years after 2020.
REPORTABLE SEGMENTS
As of December 31, 2021, we served approximately 5.2 million members eligible for Medicaid, Medicare, and other government-sponsored healthcare programs for low-income families and individuals, including Marketplace members, most of whom receive government premium subsidies.
In the first quarter of 2021, we realigned our reportable operating segments to reflect recent changes in our internal operating and reporting structure, which is now organized by government program. These reportable segments consist of: 1) Medicaid; 2) Medicare; 3) Marketplace; and 4) Other.
The Medicaid, Medicare, and Marketplace segments represent the government-funded or sponsored programs under which we offer managed healthcare services. The Other segment, which is insignificant to our consolidated results of operations, includes certain corporate amounts not associated with or allocated to the Medicaid, Medicare, or Marketplace segments. Additionally, the Other segment includes service revenues and service costs associated with the long-term services and supports consultative services we now provide in Wisconsin, as a result of the Magellan Complete Care acquisition on December 31, 2020.
Molina Healthcare, Inc. 2021 Form 10-K | 37
HOW WE ASSESS PERFORMANCE
We derive our revenues primarily from health insurance premiums. Our primary customers are state Medicaid agencies and the federal government.
The key metrics used to assess the performance of our Medicaid, Medicare, and Marketplace segments are premium revenue, medical margin and MCR. MCR represents the amount of medical care costs as a percentage of premium revenue. Therefore, the underlying medical margin, or the amount earned by the Medicaid, Medicare, and Marketplace segments after medical costs are deducted from premium revenue, represents the most important measure of earnings reviewed by management, and is used by our chief executive officer to review results, assess performance, and allocate resources. The key metric used to assess the performance of our Other segment is service margin. The service margin is equal to service revenue minus cost of service revenue.
Management’s discussion and analysis of the change in medical margin is discussed below under “Segment Financial Performance.” For more information, see Notes to Consolidated Financial Statements, Note 16, “Segments.”
TRENDS AND UNCERTAINTIES
For a discussion of the trends, uncertainties and other developments that affected our reportable segments during the year, refer to “Item 1. Business—Our Business,” “—COVID-19 Pandemic,” “—Legislative and Political Environment,” “—Operations—Medical Management,” and “—Regulation.”
SEGMENT FINANCIAL PERFORMANCE
The following table summarizes our membership by segment as of the dates indicated:
| | | | | | | | | | | |
| As of December 31, |
| 2021 | | 2020 |
| | | |
| | | |
| | | |
| Medicaid | 4,329,000 | | | 3,599,000 | |
| | | |
| | | |
| Medicare | 142,000 | | | 115,000 | |
| | | |
| Marketplace | 728,000 | | | 318,000 | |
Total (1) | 5,199,000 | | | 4,032,000 | |
____________________
(1)Approximately 200,000 members, from the Magellan Complete Care acquisition that closed on December 31, 2020, are not included in the totals as of December 31, 2020.
The tables below summarize premium revenue, medical margin, and MCR by segment for the periods indicated (dollars in millions):
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 |
| Premium Revenue | | Medical Margin | | MCR | | Premium Revenue | | Medical Margin | | MCR |
| | | | | |
| Medicaid | $ | 20,461 | | | $ | 2,322 | | | 88.7 | % | | $ | 14,265 | | | $ | 1,804 | | | 87.4 | % |
| Medicare | 3,361 | | | 430 | | | 87.2 | | | 2,512 | | | 351 | | | 86.0 | |
| Marketplace | 3,033 | | | 399 | | | 86.9 | | | 1,522 | | | 324 | | | 78.7 | |
| Total | $ | 26,855 | | | $ | 3,151 | | | 88.3 | % | | $ | 18,299 | | | $ | 2,479 | | | 86.5 | % |
Medicaid
Medicaid premium revenue increased $6.2 billion in 2021, when compared with 2020, mainly due to the impact from the Magellan Complete Care, and other acquisitions closed in the second half of 2020, the Affinity acquisition that closed in the fourth quarter of 2021, and organic membership growth. Excluding acquisitions, membership growth occurred across nearly all our states and was mainly driven by the extension of the PHE period and the associated suspension of membership redeterminations. Also contributing to the overall premium revenue increase was a lower impact of COVID-related risk corridors in 2021 compared to 2020.
As described in “Item 1. Business—COVID-19 Pandemic,” we recognized approximately $323 million in 2021, for the impact of COVID-related risk corridors enacted in most states in 2020, mainly related to Medicaid, in response
Molina Healthcare, Inc. 2021 Form 10-K | 38
to the lower utilization of medical services resulting from COVID-19. We recognized $564 million related to COVID-related risk corridors in 2020, mainly related to Medicaid.
The Medical Margin of our Medicaid program increased $518 million, or 29%, in 2021 when compared with 2020. The increase was driven by increased premium revenues and margin associated with the membership growth discussed above, partially offset by the MCR increase discussed below.
The Medicaid MCR increased to 88.7% in 2021, from 87.4% in 2020, or 130 basis points. The increase in the Medicaid MCR in 2021 was mainly due to business mix changes, partially offset by continued medical cost management and a year-over-year decrease in the net effect of COVID. The year-over-year change in impact of the net effect of COVID reflects the decrease in COVID-related risk corridors discussed above, partially offset by an increase in COVID-related inpatient costs, and lower COVID-related utilization curtailment. The Medicaid MCR is consistent with our long-term target despite the net effect of COVID.
Medicare
Medicare premium revenue increased $849 million in 2021, when compared with 2020, primarily due to the impact of higher membership, mainly from the Magellan Complete Care acquisition, and higher premium revenue PMPM.
The Medical Margin for Medicare increased $79 million, or 23%, in 2021 when compared with 2020. The year-over-year increase in margin is driven by the increase in premium revenue from higher volume, partially offset by the MCR increase discussed below.
The Medicare MCR increased to 87.2% in 2021, from 86.0% in 2020, or 120 basis points. The increase was primarily driven by the net effect of COVID, including higher direct COVID medical costs, resulting from higher infection rates in our Medicare population. The net effect of COVID had a negligible impact on the MCR in 2020. The Medicare MCR is in line with our long-term target despite the net effect of COVID.
Marketplace
Marketplace premium revenue increased $1.5 billion in 2021, when compared with 2020, mainly due to higher membership, partially offset by a decrease in premium revenue PMPM. Our Marketplace membership as of December 31, 2021, amounted to 728,000 members, representing growth of 410,000 members year over year, and substantially exceeding our expectations. This improvement resulted from several factors, including strong product design and competitive pricing, better than expected natural attrition rates, and the extended special enrollment period. The decrease in premium revenue PMPM was mainly driven by changes in business mix, with an increase of members in the bronze metal tier.
The Marketplace Medical Margin increased $75 million in 2021, primarily due to the increase in membership and premiums, mostly offset by an increase in the MCR compared to 2020.
The Marketplace MCR increased to 86.9% in 2021, compared to 78.7% in 2020, or 820 basis points. The increase in MCR resulted mainly from a higher net effect of COVID, due to continued COVID utilization pressure in our largest Marketplace geographies, and increased non-COVID medical costs by members enrolled through the special enrollment period. Special Enrollment Period membership grew to almost 40% of our Marketplace book by the fourth quarter, and many of the new members that we attracted in 2021 were in regions disproportionately affected by COVID, particularly in Texas. Moreover, we attracted a large number of members through the special enrollment period, and those members experienced higher non-COVID utilization in addition to COVID-related costs.
Other
The Other segment includes service revenues and costs associated with the long-term services and supports consultative services we now provide in Wisconsin as a result of our Magellan Complete Care acquisition, and also includes certain corporate amounts not allocated to the Medicaid, Medicare, or Marketplace segments. Such amounts were immaterial to our consolidated results of operations for 2021 and 2020.
LIQUIDITY AND FINANCIAL CONDITION
LIQUIDITY
We manage our cash, investments, and capital structure to meet the short- and long-term obligations of our business while maintaining liquidity and financial flexibility. We forecast, analyze, and monitor our cash flows to enable prudent investment management and financing within the confines of our financial strategy.
Molina Healthcare, Inc. 2021 Form 10-K | 39
We maintain liquidity at two levels: 1) the regulated health plan subsidiaries; and 2) the parent company.
Our regulated health plan subsidiaries’ primary liquidity requirements include payment of medical claims and other health care services; payment of certain settlements with our state and federal customers, such as MLR and risk corridors and Marketplace risk transfers on behalf of CMS; general and administrative costs directly incurred or paid through an administrative services agreement to the parent company; and federal tax payments to the parent company under an intercompany tax sharing agreement. Our regulated health plan subsidiaries meet their liquidity needs by generating cash flows from operating activities, primarily from premium revenue; cash flows from investing activities, including investment income and sales of investments; and capital contributions received from our parent company.
Our regulated health plan subsidiaries generally receive premiums in advance of payments of claims for medical and other health care services; however, cash and cash equivalents in regulated health plan subsidiaries can fluctuate significantly in a particular period depending on the timing of receipts for premiums from our government partners. Any decline or delay in receipt of premium revenue could have a negative impact on our liquidity. We did not experience noticeable delays to, or changes in, the timing or level of premium receipts in 2021 as a result of the COVID-19 pandemic, but there can be no assurance that we will not experience such delays in the future. See further discussion below in “Future Sources and Uses of Liquidity—Future Uses—Potential Impact of COVID-19 Pandemic.”
Our regulated health plan subsidiaries are each subject to applicable state regulations that, among other things, require the maintenance of minimum levels of capital and surplus. We continue to maintain appropriate levels of aggregate excess statutory capital and surplus in our regulated health plan subsidiaries. See further discussion under “Regulatory Capital and Dividend Restrictions” below. When available and as permitted by applicable regulations, cash in excess of the capital needs of our regulated health plan subsidiaries is generally paid in the form of dividends to our parent company to be used for general corporate purposes. The regulated health plan subsidiaries paid dividends to the parent company amounting to $564 million in 2021 and $635 million in 2020.
Parent company liquidity requirements generally consist of payment of administrative costs not directly incurred by our regulated operations, including, but not limited to, staffing costs, lease payments, branding and certain information technology services; capital contributions paid to our regulated health plan subsidiaries, including funding for newer health plans; capital expenditures; debt service; funding for common stock purchases, acquisitions and other growth-related activities; and federal tax payments. The parent company contributed capital of $440 million and $107 million in 2021 and 2020, respectively, to our regulated health plan subsidiaries to satisfy statutory capital and surplus requirements. The increased contributions in 2021 were mainly attributed to fund growth in our New York and Kentucky health plans. Our parent company normally meets its liquidity requirements by earning administrative services fees under administrative services agreements; dividends received from our regulated subsidiaries; collecting federal tax payments from the regulated subsidiaries; proceeds from issuance of debt and equity securities; and cash flows from investing activities, including investment income and sales of investments.
Cash, cash equivalents and investments at the parent company amounted to $348 million and $644 million as of December 31, 2021, and 2020, respectively. The decrease in 2021 was due to cash used for acquisitions and share repurchases, partially offset by dividends received from regulated health plan subsidiaries. In the first quarter of 2021, we purchased an aggregate of approximately 577,000 shares for $122 million, and we also paid $6 million to settle shares purchased in late December 2020.
Investments
After considering expected cash flows from operating activities, we generally invest cash of regulated subsidiaries that exceeds our expected short-term obligations in longer term, investment-grade, and marketable debt securities to improve our overall investment return. These investments are made pursuant to board-approved investment policies which conform to applicable state laws and regulations.
Our investment policies are designed to provide liquidity, preserve capital, and maximize total return on invested assets, all in a manner consistent with state requirements that prescribe the types of instruments in which our subsidiaries may invest. These investment policies require that our investments have final maturities of less than 10 years, or less than 10 years average life for structured securities. Professional portfolio managers operating under documented guidelines manage our investments and a portion of our cash equivalents. Our portfolio managers must obtain our prior approval before selling investments where the loss position of those investments exceeds certain levels.
Molina Healthcare, Inc. 2021 Form 10-K | 40
We believe that the risks of the COVID-19 pandemic, as they relate to our investments, are minimal. The overall rating of our portfolio is AA. Our investment policy has directives in conjunction with state guidelines to minimize risks and exposures in volatile markets. Additionally, our portfolio managers assist us in navigating the current volatility in the capital markets.
Our restricted investments are invested principally in cash, cash equivalents, and U.S. Treasury securities; we have the ability to hold such restricted investments until maturity. All of our unrestricted investments are classified as current assets.
Cash Flow Activities
Our cash flows are summarized as follows:
| | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | Change |
| | | | | |
| (In millions) |
| Net cash provided by operating activities | $ | 2,119 | | | $ | 1,898 | | | $ | 221 | |
| Net cash used in investing activities | (1,653) | | | (400) | | | (1,253) | |
| Net cash (used in) provided by financing activities | (183) | | | 217 | | | (400) | |
| Net increase (decrease) in cash, cash equivalents, and restricted cash and cash equivalents | $ | 283 | | | $ | 1,715 | | | $ | (1,432) | |
Operating Activities
We typically receive capitation payments monthly, in advance of payments for medical claims; however, government payors may adjust their payment schedules, positively or negatively impacting our reported cash flows from operating activities in any given period. For example, government payors may delay our premium payments, or they may prepay the following month’s premium payment.
Net cash provided by operations was $2.1 billion in 2021, compared with $1.9 billion of net cash provided in 2020. The $221 million increase in cash flow was due to the growth in operations and the net impact of timing differences in government receivables and payables.
Investing Activities
Net cash used in investing activities was $1.7 billion in 2021, compared with $400 million of net cash used in 2020, a decrease in year-over-year cash flow of $1.3 billion. This change in cash flow was primarily due to increased purchases of investments in 2021, after a temporarily higher allocation in shorter-term invested assets during the COVID-19 pandemic was rescinded in the second quarter of 2021.
Financing Activities
Net cash used in financing activities was $183 million in 2021, compared with $217 million of net cash provided by 2020, a decrease in year-over-year cash flow of $400 million. In 2021, cash inflows included $740 million from the issuance of the 3.875% Notes due 2032, and cash outflows included $723 million in repayment of the 5.375% Notes due 2022, common stock purchases of $128 million and $53 million for common stock withheld to settle employee tax obligations. Additionally, we paid $23 million to settle contingent consideration liabilities relating to our Kentucky Passport acquisition that closed in 2020, $20 million of which has been presented as a financing cash outflow. In the year ended December 31, 2020, financing cash inflows included $1,429 million from the issuance of the 4.375% Notes due 2028 and 3.875% Notes due 2030 and $380 million borrowed under the term loan facility. Cash outflows included the $600 million repayment of the term loan facility, common stock purchases of $606 million, which included $7 million to settle shares purchased in late December 2019, and net cash paid for the senior notes-related transactions amounting to $380 million.
FINANCIAL CONDITION
We believe that our cash resources, borrowing capacity available under our Credit Agreement as discussed further below in “Future Sources and Uses of Liquidity—Future Sources,” and internally generated funds will be sufficient to support our operations, regulatory requirements, debt repayment obligations and capital expenditures for at least the next 12 months.
On a consolidated basis, as of December 31, 2021, our working capital was $3.0 billion compared with $2.9 billion as of December 31, 2020. At December 31, 2021, our cash and investments amounted to $7.9 billion, compared with $6.2 billion of cash and investments at December 31, 2020.
Molina Healthcare, Inc. 2021 Form 10-K | 41
Because of the statutory restrictions that inhibit the ability of our health plan subsidiaries to transfer net assets to us, the amount of retained earnings readily available to pay dividends to our stockholders is generally limited to cash, cash equivalents and investments held by our unregulated parent. For more information, see the “Liquidity” discussion presented above.
Regulatory Capital and Dividend Restrictions
Each of our regulated, wholly owned subsidiaries must maintain a minimum amount of statutory capital determined by statute or regulations. Such statutes, regulations and capital requirements also restrict the timing, payment and amount of dividends and other distributions, loans or advances that may be paid to us as the sole stockholder. To the extent our subsidiaries must comply with these regulations, they may not have the financial flexibility to transfer funds to us. Based upon current statutes and regulations, the minimum capital and surplus requirement for these subsidiaries was estimated to be approximately $2.1 billion at December 31, 2021, compared with $1.5 billion at December 31, 2020. The aggregate capital and surplus of our wholly owned subsidiaries was in excess of these minimum capital requirements as of both dates.
Under applicable regulatory requirements, the amount of dividends that may be paid by our wholly owned subsidiaries without prior approval by regulatory authorities as of December 31, 2021, was approximately $197 million in the aggregate. The subsidiaries may pay dividends over this amount, but only after approval is granted by the regulatory authorities.
Based on our cash and investments balances as of December 31, 2021, management believes that our regulated wholly owned subsidiaries remain well capitalized and exceed their regulatory minimum requirements. We have the ability, and have committed to provide, additional capital to each of our health plans as necessary to ensure compliance with statutory capital and surplus requirements.
Capital Structure
In September 2021, our board of directors authorized the purchase of up to $500 million, in the aggregate, of our common stock. This new program immediately supersedes the stock purchase program previously approved by our board of directors in September 2020. This new program will be funded with cash on hand and extends through December 31, 2022.
As debt held by the parent company comes due, we typically engage in a new private offering of debt to retire and replace the prior issuance. Over the last several years we have seen a continued decline in interest rates, which has benefited our overall cost of capital during that time. There is no guarantee that the interest rate environment will continue to see declines in interest rates in the future, and future refinancing may occur at a higher rate than those we have achieved historically. This could increase our cost of capital in the future or cause us to pursue alternative financing sources, should the need arise.
We are not a party to any off-balance sheet financing arrangements.
Debt Ratings
Each of our senior notes is rated “BB-” by Standard & Poor’s, and “Ba3” by Moody’s Investor Service, Inc. A downgrade in our ratings could adversely affect our borrowing capacity and increase our borrowing costs.
Financial Covenants
The Credit Agreement contains customary non-financial and financial covenants, including a net leverage ratio and an interest coverage ratio. Such ratios are computed as defined by the terms of the Credit Agreement.
In addition, the indentures governing each of our outstanding senior notes contain cross-default provisions that are triggered upon default by us or any of our subsidiaries on any indebtedness in excess of the amount specified in the applicable indenture. As of December 31, 2021, we were in compliance with all financial and non-financial covenants under the Credit Agreement and other long-term debt.
FUTURE SOURCES AND USES OF LIQUIDITY
Future Sources
Our regulated subsidiaries generate significant cash flows from premium revenue, which is generally received a short time before related healthcare services are paid. Premium revenue is our primary source of liquidity. Thus, any decline in the receipt of premium revenue, and our profitability, could have a negative impact on our liquidity.
Molina Healthcare, Inc. 2021 Form 10-K | 42
Potential Impact of COVID-19 Pandemic. Excluding acquisitions and our exit from Puerto Rico, we have added approximately 750,000 new Medicaid members since March 31, 2020, when we first began to report on the impacts of the pandemic. We believe this membership increase was mainly due to the suspension of redeterminations for Medicaid eligibility. We expect Medicaid enrollment to continue to benefit from the extension of the PHE period, and the associated pause on membership redeterminations, at least through mid-April 2022.
Dividends from Subsidiaries. When available and as permitted by applicable regulations, cash in excess of the capital needs of our regulated health plans is generally paid in the form of dividends to our unregulated parent company to be used for general corporate purposes. As a result of the COVID-19 pandemic, state regulators could restrict the ability of our regulated health plan subsidiaries to pay dividends to the parent company, which could reduce the liquidity of the parent company. For more information on our regulatory capital requirements and dividend restrictions, refer to Notes to Consolidated Financial Statements, Note 15, “Commitments and Contingencies—Regulatory Capital Requirements and Dividend Restrictions,” and Note 17, “Condensed Financial Information of Registrant—Note C - Dividends and Capital Contributions.”
Credit Agreement Borrowing Capacity. As of December 31, 2021, we had available borrowing capacity of $1 billion under the revolving credit facility of our Credit Agreement. In addition, the Credit Agreement provides for a $15 million swingline sub-facility and a $100 million letter of credit sub-facility, as well as incremental term loans available to finance certain acquisitions up to $500 million, plus an unlimited amount of such term loans as long as we maintain a minimum consolidated net leverage ratio. See further discussion in the Notes to Consolidated Financial Statements, Note 11, “Debt.”
Future Uses
Common Stock Purchases. In September 2021, our board of directors authorized the purchase of up to $500 million, in the aggregate, of our common stock. This new program immediately supersedes the stock purchase program previously approved by our board of directors in September 2020. This new program will be funded with cash on hand and extends through December 31, 2022. The exact timing and amount of any repurchase is determined by management based on market conditions and share price, in addition to other factors, and subject to the restrictions relating to volume, price, and timing under applicable law. As of February 14, 2022, $500 million remained available to purchase our common stock under this program through December 31, 2022. See further information in the Notes to Consolidated Financial Statements, Note 13, “Stockholders' Equity.”
Acquisitions. We have a disciplined and steady approach to growth. Organic growth, which includes leveraging our existing health plan portfolio and winning new territories, is our highest priority. In addition to organic growth, we will consider targeted acquisitions that are a strategic fit that we believe will leverage operational synergies, and lead to incremental earnings accretion. For further information on our acquisitions, refer to the Notes to Consolidated Financial Statements, Note 4, “Business Combinations.”
On October 7, 2021, we announced a definitive agreement to acquire the Medicaid Managed Long Term Care business of AgeWell New York. As of August 31, 2021, AgeWell served approximately 13,000 managed long-term services and supports members, with full-year 2020 premium revenue of approximately $700 million. The purchase price for the transaction is approximately $106 million, net of certain tax benefits and target allocation of required regulatory capital, which we intend to fund with cash on hand. The transaction is subject to applicable federal and state regulatory approvals and the satisfaction of other customary closing conditions. We currently expect the transaction to close by the third quarter of 2022.
Potential Impact of COVID-19 Pandemic. As described in “Item 1. Business—COVID-19 Pandemic,” we have been subject to Medicaid risk corridors as a result of the pandemic. Beginning in 2020, through December 31, 2021, various states enacted temporary risk corridors in response to the reduced demand for medical services stemming from COVID-19, which have resulted in a reduction of our medical margin, primarily in the Medicaid segment. In some cases, these risk corridors were retroactive to earlier periods in 2020, or as early as the beginning of the states’ fiscal years in 2019. Beginning in the second quarter of 2020, we have recognized retroactive risk corridors that we believe to be probable, and where the ultimate premium amount is reasonably estimable. We recognized approximately $323 million, in the aggregate, related to such risk corridors, in 2021, and approximately $564 million, in the aggregate, was recognized in 2020.
It is possible that certain states could change the structure of existing risk corridors, implement new risk corridors in the future or discontinue existing risk corridors. Due to these uncertainties, the ultimate outcomes could differ materially from our estimates as a result of changes in facts or further developments, which could have an adverse effect on our consolidated financial position, results of operations, or cash flows.
Molina Healthcare, Inc. 2021 Form 10-K | 43
Regulatory Capital Requirements and Dividend Restrictions. We have the ability, and have committed to provide, additional capital to each of our health plans as necessary to ensure compliance with minimum statutory capital requirements.
The Molina Healthcare Charitable Foundation. In August 2020, we announced our commitment of $150 million to fund The Molina Healthcare Charitable Foundation (the “Foundation”), an independent not-for-profit charitable foundation. We contributed $15 million to the Foundation in the fourth quarter of 2020.
Contractual Obligations. We are party to various contractual obligations that we will be required to satisfy over the short and long term. The majority are discussed in the Notes to Consolidated Financial Statements and primarily include the following: medical claims and benefits payable, amounts due to government agencies, principal and interest on our debt and leases. Some items are based on management’s estimates and assumptions about obligations, including duration, the possibility of renewal, anticipated actions by third parties, and other factors. Because these estimates and assumptions are necessarily subjective, the contractual obligations we will actually pay in future periods may vary. Additionally, we have a variety of other contractual agreements related to acquiring services used in our operations. However, we believe these other agreements do not contain material non-cancelable commitments.
CRITICAL ACCOUNTING ESTIMATES
When we prepare our consolidated financial statements, we use estimates and assumptions that may affect reported amounts and disclosures. Actual results could differ from these estimates, and some differences could be material. Our most significant accounting estimates, which include a higher degree of judgment and/or complexity, include the following:
•Medical claims and benefits payable. See discussion below, and refer to the Notes to Consolidated Financial Statements, Notes 2, “Significant Accounting Policies,” and 10, “Medical Claims and Benefits Payable” for more information.
•Contractual provisions that may adjust or limit revenue or profit. For a discussion of this topic, including amounts recorded in our consolidated financial statements, refer to the Notes to Consolidated Financial Statements, Note 2, “Significant Accounting Policies.”
•Quality incentives. For a discussion of this topic, refer to the Notes to Consolidated Financial Statements, Note 2, “Significant Accounting Policies.”
•Business Combinations, and Goodwill and intangible assets, net. For a comprehensive discussion of this topic, including amounts recorded in our consolidated financial statements, refer to the Notes to Consolidated Financial Statements, Note 2, “Significant Accounting Policies,” Note 4, “Business Combinations,” and Note 9, “Goodwill and Intangible Assets, Net.”
MEDICAL CARE COSTS, MEDICAL CLAIMS AND BENEFITS PAYABLE
Medical care costs are recognized in the period in which services are provided and include fee-for-service claims, pharmacy benefits, capitation payments to providers, and various other medically-related costs. Under fee-for-service claims arrangements with providers, we retain the financial responsibility for medical care provided and incur costs based on actual utilization of hospital and physician services. Such medical care costs include amounts paid by us as well as estimated medical claims and benefits payable for costs that were incurred but not paid as of the reporting date (“IBNP”). Pharmacy benefits represent payments for members' prescription drug costs, net of rebates from drug manufacturers. We estimate pharmacy rebates based on historical and current utilization of prescription drugs and contractual provisions. Capitation payments represent monthly contractual fees paid to providers, who are responsible for providing medical care to members, which could include medical or ancillary costs like dental, vision and other supplemental health benefits. Such capitation costs are fixed in advance of the periods covered and are not subject to significant accounting estimates. Other medical care costs include all medically-related administrative costs, amounts due to providers pursuant to risk-sharing or other incentive arrangements, provider claims, and other healthcare expenses. Examples of medically-related administrative costs include expenses relating to health education, quality assurance, case management, care coordination, disease management, and 24-hour on-call nurses. Additionally, we include an estimate for the cost of settling claims incurred through the reporting date in our medical claims and benefits payable liability.
Molina Healthcare, Inc. 2021 Form 10-K | 44
The following table illustrates consolidated medical care costs by type for the periods indicated:
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2021 | | 2020 |
| Amount | | PMPM | | % of
Total | | Amount | | PMPM | | % of
Total |
| | | | | | | | | | | |
| (In millions, except PMPM amounts) |
| Fee-for-service | $ | 17,433 | | | $ | 303.80 | | | 73.5 | % | | $ | 11,590 | | | $ | 261.30 | | | 73.3 | % |
| Pharmacy | 3,831 | | | 66.77 | | | 16.2 | | | 2,012 | | | 45.37 | | | 12.7 | |
| Capitation | 1,471 | | | 25.64 | | | 6.2 | | | 1,459 | | | 32.88 | | | 9.2 | |
| Other | 969 | | | 16.88 | | | 4.1 | | | 759 | | | 17.10 | | | 4.8 | |
| Total | $ | 23,704 | | | $ | 413.09 | | | 100.0 | % | | $ | 15,820 | | | $ | 356.65 | | | 100.0 | % |
Medical claims and benefits payable consist mainly of fee-for-service IBNP, unpaid pharmacy claims, capitation costs, other medical costs, including amounts payable to providers pursuant to risk-sharing or other incentive arrangements and amounts payable to providers on behalf of certain state agencies for certain state assessments in which we assume no financial risk. IBNP includes the costs of claims incurred as of the balance sheet date which have been reported to us, and our best estimate of the cost of claims incurred but not yet reported to us. We also include an additional reserve to ensure that our overall IBNP liability is sufficient under moderately adverse conditions. We reflect changes in these estimates in the consolidated results of operations in the period in which they are determined.
The estimation of the IBNP liability requires a significant degree of judgment in applying actuarial methods, determining the appropriate assumptions and considering numerous factors. Of those factors, we consider estimated completion factors (measures the cumulative percentage of claims expense that will ultimately be paid for a given month of service based on historical payment patterns) and the assumed healthcare cost trend (the year-over-year change in per-member per-month medical care costs) to be the most critical assumptions. Other relevant factors also include, but are not limited to, healthcare service utilization trends, claim inventory levels, changes in membership, product mix, seasonality, benefit changes or changes in fee schedules, provider contract changes, prior authorizations and the incidence of catastrophic or pandemic cases.
For claims incurred more than three months before the financial statement date, we mainly use estimated completion factors to estimate the ultimate cost of those claims. Completion factors measure the cumulative percentage of claims expense that will ultimately be paid for a given month of service based on historical claims payment patterns. We analyze historical claims payment patterns by comparing claim incurred dates to claim payment dates to estimate completion factors. The estimated completion factors are then applied to claims paid through the financial statement date to estimate the ultimate claims cost for a given month’s incurred claim activity. The difference between the estimated ultimate claims cost and the claims paid through the financial statement date represents our estimate of claims remaining to be paid as of the financial statement date and is included in our IBNP liability.
For claims incurred within three months before the financial statement date, actual claims paid are a less reliable measure of our ultimate cost since a large portion of medical claims are not submitted to us until several months after services have been submitted. Accordingly, we estimate our IBNP liability for claims incurred during these months based on a blend of estimated completion factors and assumed medical care cost trend. The assumed medical care cost trend represents the year-over-year change in per-member per-month medical care costs, which can be affected by many factors including, but not limited to, our ability and practices to manage medical and pharmaceutical costs, changes in level and mix of services utilized, mix of benefits offered, including the impact of co-pays and deductibles, changes in medical practices, changes in member demographics, catastrophes and epidemics, and other relevant factors.
Actuarial standards of practice generally require a level of confidence such that our overall best estimate of the IBNP liability has a greater probability of being adequate versus being insufficient, where the liability is sufficient to account for moderately adverse conditions. Adverse conditions are situations that may cause actual claims to be higher than the otherwise estimated value of such claims at the time of the estimate, such as changes in the magnitude or severity of claims, uncertainties related to our entry into new geographical markets or provision of services to new populations, changes in state-controlled fee schedules, and modifications or upgrades to our claims processing systems and practices. Therefore, in many situations, the claim amounts ultimately settled will be less than the estimate that satisfies the actuarial standards of practice.
Molina Healthcare, Inc. 2021 Form 10-K | 45
When subsequent actual claims payments are less than we estimated, we recognize a benefit for favorable prior period development that is reported as part of “Components of medical care costs related to: “Prior years” in the table presented in Note 10, “Medical Claims and Benefits Payable.” Our reserving practice is to consistently recognize the actuarial best estimate including a provision for moderately adverse conditions for each current period. This provision is reported as part of “Components of medical care costs related to: Current year” in the table presented in Note 10. Assuming stability in the size of our membership, the use of this consistent methodology, during any given period, usually results in the replenishment of reserves at a level that generally offsets the benefit of favorable prior period development in that period. In the case of material growth or decline of membership, replenishment can exceed or fall short of the favorable development, assuming all other factors remain unchanged.
Because of the significant degree of judgment involved in estimation of our IBNP liability, there is considerable variability and uncertainty inherent in such estimates. The following table reflects the hypothetical change in our estimate of claims liability as of December 31, 2021 that would result if we change our completion factors for the fourth through the twelfth months preceding December 31, 2021, by the percentages indicated. A reduction in the completion factor results in an increase in medical claims liabilities. Dollar amounts are in millions.
| | | | | |
| Increase (Decrease) in Estimated Completion Factors | Increase
(Decrease)
in Medical Claims
and
Benefits Payable |
| (6)% | $ | 811 | |
| (4)% | 541 | |
| (2)% | 270 | |
| 2% | (270) | |
| 4% | (541) | |
| 6% | (811) | |
The following table reflects the hypothetical change in our estimate of claims liability as of December 31, 2021 that would result if we alter our assumed medical care cost trend factors by the percentages indicated. An increase in the PMPM costs results in an increase in medical claims liabilities. Dollar amounts are in millions.
| | | | | |
| (Decrease) Increase in Trended Per Member Per Month Cost Estimates | (Decrease)
Increase
in Medical Claims
and
Benefits Payable |
| (6)% | $ | (285) | |
| (4)% | (190) | |
| (2)% | (95) | |
| 2% | 95 | |
| 4% | 190 | |
| 6% | 285 | |
There are many related factors working in conjunction with one another that determine the accuracy of our estimates, some of which are qualitative in nature rather than quantitative. Therefore, we are seldom able to quantify the impact that any single factor has on a change in estimate. Given the variability inherent in the reserving process, we will only be able to identify specific factors if they represent a significant departure from expectations. As a result, we do not expect to be able to fully quantify the impact of individual factors on changes in estimates.
RECENTLY ISSUED ACCOUNTING STANDARDS
Refer to the Notes to Consolidated Financial Statements, Note 2, “Significant Accounting Policies,” for a discussion of recent accounting pronouncements that affect us.
Molina Healthcare, Inc. 2021 Form 10-K | 46
QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT MARKET RISK
Our earnings and financial position are exposed to financial market risk relating to changes in interest rates, and the resulting impact on investment income and interest expense.
Substantially all of our investments and restricted investments are subject to interest rate risk and will decrease in value if market interest rates increase. Assuming a hypothetical and immediate 1% increase in market interest rates at December 31, 2021, the fair value of our fixed income investments would decrease by approximately $69 million. Declines in interest rates over time will reduce our investment income.
For further information on fair value measurements and our investment portfolio, please refer to the Notes to Consolidated Financial Statements, Note 5, “Fair Value Measurements,” and Note 6, “Investments.”
Borrowings under the Credit Agreement bear interest based, at our election, on a base rate or other defined rate, plus, in each case, the applicable margin. For further information, see Notes to Consolidated Financial Statements, Note 11, “Debt.”
Molina Healthcare, Inc. 2021 Form 10-K | 47
MOLINA HEALTHCARE, INC.
FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA
Molina Healthcare, Inc. 2021 Form 10-K | 48
CONSOLIDATED STATEMENTS OF INCOME
| | | | | | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2021 | | 2020 | | 2019 |
| | | | | |
| | (In millions, except per-share data) |
| Revenue: | | | | | |
| Premium revenue | $ | 26,855 | | | $ | 18,299 | | | $ | 16,208 | |
| Premium tax revenue | 787 | | | 649 | | | 489 | |
| Health insurer fees reimbursed | — | | | 271 | | | — | |
| Marketplace risk corridor judgment | — | | | 128 | | | — | |
| Investment income | 52 | | | 59 | | | 115 | |
| Other revenue | 77 | | | 17 | | | 17 | |
| Total revenue | 27,771 | | | 19,423 | | | 16,829 | |
| Operating expenses: | | | | | |
| Medical care costs | 23,704 | | | 15,820 | | | 13,905 | |
| General and administrative expenses | 2,068 | | | 1,480 | | | 1,296 | |
| Premium tax expenses | 787 | | | 649 | | | 489 | |
| Health insurer fees | — | | | 277 | | | — | |
| Depreciation and amortization | 131 | | | 88 | | | 89 | |
| Other | 61 | | | 31 | | | 6 | |
| Total operating expenses | 26,751 | | | 18,345 | | | 15,785 | |
| Operating income | 1,020 | | | 1,078 | | | 1,044 | |
| Other expenses, net: | | | | | |
| Interest expense | 120 | | | 102 | | | 87 | |
| Other expenses (income), net | 25 | | | 15 | | | (15) | |
| Total other expenses, net | 145 | | | 117 | | | 72 | |
| Income before income tax expense | 875 | | | 961 | | | 972 | |
| Income tax expense | 216 | | | 288 | | | 235 | |
| Net income | $ | 659 | | | $ | 673 | | | $ | 737 | |
| | | | | |
| Net income per share: | | | | | |
| Basic | $ | 11.40 | | | $ | 11.40 | | | $ | 11.85 | |
| Diluted | $ | 11.25 | | | $ | 11.23 | | | $ | 11.47 | |
| Weighted average shares outstanding: | | | | | |
| Basic | 57.8 | | | 59.0 | | | 62.2 | |
| Diluted | 58.6 | | | 59.9 | | | 64.2 | |
CONSOLIDATED STATEMENTS OF COMPREHENSIVE INCOME
| | | | | | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2021 | | 2020 | | 2019 |
| | | | | |
| | (In millions) |
| Net income | $ | 659 | | | $ | 673 | | | $ | 737 | |
| Other comprehensive (loss) income: | | | | | |
| Unrealized investment (loss) income | (55) | | | 44 | | | 16 | |
Less: effect of income taxes | (13) | | | 11 | | | 4 | |
| Other comprehensive (loss) income, net of tax | (42) | | | 33 | | | 12 | |
| Comprehensive income | $ | 617 | | | $ | 706 | | | $ | 749 | |
See accompanying notes.
Molina Healthcare, Inc. 2021 Form 10-K | 49
CONSOLIDATED BALANCE SHEETS
| | | | | | | | | | | |
| December 31, |
| 2021 | | 2020 |
| | | |
| (Dollars in millions,
except per-share amounts) |
| ASSETS |
| Current assets: | | | |
| Cash and cash equivalents | $ | 4,438 | | | $ | 4,154 | |
| Investments | 3,202 | | | 1,875 | |
| Receivables | 2,177 | | | 1,672 | |
| Prepaid expenses and other current assets | 247 | | | 175 | |
| Total current assets | 10,064 | | | 7,876 | |
| Property, equipment, and capitalized software, net | 396 | | | 391 | |
| Goodwill and intangible assets, net | 1,252 | | | 941 | |
| Restricted investments | 212 | | | 136 | |
| Deferred income taxes | 106 | | | 69 | |
| Other assets | 179 | | | 119 | |
| Total assets | $ | 12,209 | | | $ | 9,532 | |
| | | |
| LIABILITIES AND STOCKHOLDERS’ EQUITY |
| Current liabilities: | | | |
| Medical claims and benefits payable | $ | 3,363 | | | $ | 2,696 | |
| Amounts due government agencies | 2,472 | | | 1,253 | |
| Accounts payable, accrued liabilities and other | 842 | | | 641 | |
| Deferred revenue | 370 | | | 375 | |
| Total current liabilities | 7,047 | | | 4,965 | |
| Long-term debt | 2,173 | | | 2,127 | |
| Finance lease liabilities | 219 | | | 225 | |
| Other long-term liabilities | 140 | | | 119 | |
| Total liabilities | 9,579 | | | 7,436 | |
| Stockholders’ equity: | | | |
Common stock, $0.001 par value per share; 150 million shares authorized; outstanding: 58 million shares at December 31, 2021, and 59 million at December 31, 2020 | — | | | — | |
Preferred stock, $0.001 par value per share; 20 million shares authorized, no shares issued and outstanding | — | | | — | |
| Additional paid-in capital | 236 | | | 199 | |
| Accumulated other comprehensive (loss) income | (5) | | | 37 | |
| Retained earnings | 2,399 | | | 1,860 | |
| Total stockholders’ equity | 2,630 | | | 2,096 | |
| Total liabilities and stockholders’ equity | $ | 12,209 | | | $ | 9,532 | |
See accompanying notes.
Molina Healthcare, Inc. 2021 Form 10-K | 50
CONSOLIDATED STATEMENTS OF STOCKHOLDERS’ EQUITY
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Common Stock | | Additional
Paid-in
Capital | | Accumulated
Other
Comprehensive (Loss) Income | | Retained
Earnings | | Total |
| Outstanding | | Amount | | | | |
| | | | | | | | | | | |
| (In millions) |
| Balance at December 31, 2018 | 62 | | | $ | — | | | $ | 643 | | | $ | (8) | | | $ | 1,012 | | | $ | 1,647 | |
| Net income | — | | | — | | | — | | | — | | | 737 | | | 737 | |
| Common stock purchases | — | | | — | | | (1) | | | — | | | (53) | | | (54) | |
| Adoption of new accounting standards | — | | | — | | | — | | | — | | | 85 | | | 85 | |
| Partial termination of warrants | — | | | — | | | (514) | | | — | | | — | | | (514) | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Other comprehensive income, net | — | | | — | | | — | | | 12 | | | — | | | 12 | |
| Share-based compensation | — | | | — | | | 47 | | | — | | | — | | | 47 | |
| Balance at December 31, 2019 | 62 | | | — | | | 175 | | | 4 | | | 1,781 | | | 1,960 | |
| Net income | — | | | — | | | — | | | — | | | 673 | | | 673 | |
| Common stock purchases | (4) | | | — | | | (11) | | | — | | | (594) | | | (605) | |
| Termination of warrants | — | | | — | | | (30) | | | — | | | — | | | (30) | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Other comprehensive income, net | — | | | — | | | — | | | 33 | | | — | | | 33 | |
| Share-based compensation | 1 | | | — | | | 65 | | | — | | | — | | | 65 | |
| Balance at December 31, 2020 | 59 | | | — | | | 199 | | | 37 | | | 1,860 | | | 2,096 | |
| Net income | — | | | — | | | — | | | — | | | 659 | | | 659 | |
| Common stock purchases | (1) | | | — | | | (2) | | | — | | | (120) | | | (122) | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Other comprehensive loss, net | — | | | — | | | — | | | (42) | | | — | | | (42) | |
| Share-based compensation | — | | | — | | | 39 | | | — | | | — | | | 39 | |
| Balance at December 31, 2021 | 58 | | | $ | — | | | $ | 236 | | | $ | (5) | | | $ | 2,399 | | | $ | 2,630 | |
See accompanying notes.
Molina Healthcare, Inc. 2021 Form 10-K | 51
CONSOLIDATED STATEMENTS OF CASH FLOWS
| | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | |
| (In millions) |
| Operating activities: | | | | | |
| Net income | $ | 659 | | | $ | 673 | | | $ | 737 | |
| Adjustments to reconcile net income to net cash provided by operating activities: | | | | | |
| Depreciation and amortization | 131 | | | 88 | | | 89 | |
| Deferred income taxes | (24) | | | (19) | | | 10 | |
| Share-based compensation | 72 | | | 57 | | | 39 | |
| Loss (gain) on debt repayment | 25 | | | 15 | | | (15) | |
| Other, net | 33 | | | 12 | | | — | |
| Changes in operating assets and liabilities, net of the effect of acquisitions: | | | | | |
| Receivables | (415) | | | (100) | | | (76) | |
| Prepaid expenses and other current assets | (19) | | | (16) | | | 28 | |
| Medical claims and benefits payable | 471 | | | 544 | | | (107) | |
| Amounts due government agencies | 1,046 | | | 446 | | | (303) | |
| Accounts payable, accrued liabilities and other | 138 | | | 86 | | | 9 | |
| Deferred revenue | (5) | | | 126 | | | 38 | |
| Income taxes | 7 | | | (14) | | | (15) | |
| Net cash provided by operating activities | 2,119 | | | 1,898 | | | 434 | |
| Investing activities: | | | | | |
| Purchases of investments | (2,713) | | | (670) | | | (2,536) | |
| Proceeds from sales and maturities of investments | 1,329 | | | 1,097 | | | 2,302 | |
| Net cash paid in business combinations | (129) | | | (755) | | | — | |
| Purchases of property, equipment and capitalized software | (77) | | | (74) | | | (57) | |
| Other, net | (63) | | | 2 | | | (2) | |
| Net cash used in investing activities | (1,653) | | | (400) | | | (293) | |
| Financing activities: | | | | | |
| Proceeds from senior notes offerings, net of issuance costs | 740 | | | 1,429 | | | — | |
| Repayment of senior notes | (723) | | | (338) | | | — | |
Common stock purchases | (128) | | | (606) | | | (47) | |
| Common stock withheld to settle employee tax obligations | (53) | | | (8) | | | (7) | |
| Contingent consideration liabilities settled | (20) | | | — | | | — | |
| Repayment of term loan facility | — | | | (600) | | | — | |
Proceeds from borrowings under term loan facility | — | | | 380 | | | 220 | |
Cash paid for partial termination of warrants | — | | | (30) | | | (514) | |
Cash paid for partial settlement of conversion option | — | | | (27) | | | (578) | |
Cash received for partial settlement of call option | — | | | 27 | | | 578 | |
Repayment of principal amount of convertible senior notes | — | | | (12) | | | (240) | |
| Other, net | 1 | | | 2 | | | 29 | |
| Net cash (used in) provided by financing activities | (183) | | | 217 | | | (559) | |
| Net increase (decrease) in cash and cash equivalents, and restricted cash and cash equivalents | 283 | | | 1,715 | | | (418) | |
Cash and cash equivalents, and restricted cash and cash equivalents at beginning of period | 4,223 | | | 2,508 | | | 2,926 | |
Cash and cash equivalents, and restricted cash and cash equivalents at end of period | $ | 4,506 | | | $ | 4,223 | | | $ | 2,508 | |
See accompanying notes.
Molina Healthcare, Inc. 2021 Form 10-K | 52
CONSOLIDATED STATEMENTS OF CASH FLOWS
(continued)
| | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | |
| (In millions) |
| Supplemental cash flow information: | | | | | |
| Cash paid during the period for: | | | | | |
| Income taxes | $ | 235 | | | $ | 321 | | | $ | 239 | |
| Interest | $ | 127 | | | $ | 112 | | | $ | 78 | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
See accompanying notes.
Molina Healthcare, Inc. 2021 Form 10-K | 53
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
1. Organization and Basis of Presentation
Organization and Operations
Molina Healthcare, Inc. provides managed healthcare services under the Medicaid and Medicare programs, and through the state insurance marketplaces (the “Marketplace”). In the first quarter of 2021, we realigned our reportable operating segments to reflect recent changes in our internal operating and reporting structure, which is now organized by government program. These reportable segments consist of: 1) Medicaid; 2) Medicare; 3) Marketplace; and 4) Other. For further information, refer to Note 16, “Segments.”
As of December 31, 2021, we served approximately 5.2 million members eligible for government-sponsored healthcare programs, located across 18 states.
Our state Medicaid contracts typically have terms of three to five years, contain renewal options exercisable by the state Medicaid agency, and allow either the state or the health plan to terminate the contract with or without cause. Such contracts are subject to risk of loss in states that issue requests for proposal (“RFP”) open to competitive bidding by other health plans. If one of our health plans is not a successful responsive bidder to a state RFP, its contract may not be renewed.
In addition to contract renewal, our state Medicaid contracts may be periodically amended to include or exclude certain health benefits (such as pharmacy services, behavioral health services, or long-term care services); populations such as the aged, blind or disabled (“ABD”); and regions or service areas.
Recent Developments
Texas Acquisition — Medicaid and Medicare. On January 1, 2022, we closed on our acquisition of Cigna Corporation’s Texas Medicaid and Medicare-Medicaid Plan (“MMP”) contracts, along with certain operating assets. See Note 4, “Business Combinations,” for further information.
New York Acquisition — Medicaid. On October 25, 2021, we closed on our acquisition of substantially all of the assets of Affinity Health Plan, Inc., a Medicaid health plan in New York. As a result, we added approximately 310,000 members in New York. See Note 4, “Business Combinations,” for further information.
New York Acquisition—Medicaid. On October 7, 2021, we announced a definitive agreement to acquire the Medicaid Managed Long Term Care business of AgeWell New York (“AgeWell”). As of August 31, 2021, AgeWell served approximately 13,000 managed long-term services and supports members, with full-year 2020 premium revenue of approximately $700 million. The purchase price for the transaction is approximately $106 million, net of certain tax benefits and target allocation of required regulatory capital, which we intend to fund with cash on hand. The transaction is subject to applicable federal and state regulatory approvals and the satisfaction of other customary closing conditions. We currently expect the transaction to close by the third quarter of 2022.
Nevada Procurement—Medicaid. On August 17, 2021, we announced that our Nevada health plan subsidiary was selected as an awardee in Clark and Washoe Counties. This new contract commenced on January 1, 2022, and offers health coverage to TANF, CHIP and Medicaid Expansion beneficiaries. The four year contract with a possible two year extension was ratified in September 2021.
Ohio Procurement—Medicaid. On April 13, 2021, we announced that our Ohio health plan subsidiary was selected as an awardee in all three regions across the state pursuant to the Medicaid managed care request for award issued on September 30, 2020, by the Ohio Department of Medicaid. This new contract is expected to begin July 1, 2022, and will offer health care coverage to Medicaid beneficiaries through the state of Ohio’s Covered Family and Children, Expansion, and ABD programs.
Consolidation and Presentation
The consolidated financial statements include the accounts of Molina Healthcare, Inc., and its subsidiaries. All significant inter-company balances and transactions have been eliminated in consolidation. Financial information related to subsidiaries acquired during any year is included only for periods subsequent to their acquisition. In the opinion of management, all adjustments considered necessary for a fair presentation of the results as of the date and for the periods presented have been included; such adjustments consist of normal recurring adjustments.
Molina Healthcare, Inc. 2021 Form 10-K | 54
Reclassifications
Consistent with the change in reportable segments described above, certain prior year disclosures in Note 9, “Goodwill and Intangible Assets, Net,” Note 10, “Medical Claims and Benefits Payable,” and Note 16, “Segments,” have been recast to conform to the current year presentation.
Certain immaterial amounts presented in the accompanying consolidated statement of cash flows for the years ended December 31, 2020 and 2019, have been reclassified to conform to the current year presentation.
Use of Estimates
The preparation of consolidated financial statements in conformity with U.S. generally accepted accounting principles (“GAAP”) requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities. Estimates also affect the reported amounts of revenues and expenses during the reporting period. Actual results could differ from these estimates.
2. Significant Accounting Policies
Cash and Cash Equivalents
Cash and cash equivalents consist of cash and short-term, highly liquid investments that are both readily convertible into known amounts of cash and have a maturity of three months or less on the date of purchase. The following table provides a reconciliation of cash, cash equivalents, and restricted cash and cash equivalents reported within the accompanying consolidated balance sheets that sum to the total of the same such amounts presented in the accompanying consolidated statements of cash flows. The restricted cash and cash equivalents presented below are included in “Restricted investments” in the accompanying consolidated balance sheets.
| | | | | | | | | | | | | | | | | |
| December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | |
| (In millions) |
| Cash and cash equivalents | $ | 4,438 | | | $ | 4,154 | | | $ | 2,452 | |
| Restricted cash and cash equivalents | 68 | | | 69 | | | 56 | |
Total cash and cash equivalents, and restricted cash and cash equivalents presented in the consolidated statements of cash flows | $ | 4,506 | | | $ | 4,223 | | | $ | 2,508 | |
Investments
Our investments are principally held in debt securities, which are grouped into two separate categories for accounting and reporting purposes: available-for-sale securities, and held-to-maturity securities. Available-for-sale (“AFS”) securities are recorded at fair value and unrealized gains and losses, if any, are recorded in stockholders’ equity as other comprehensive income, net of applicable income taxes. Held-to-maturity (“HTM”) securities are recorded at amortized cost, which approximates fair value, and unrealized holding gains or losses are not generally recognized. Realized gains and losses and unrealized losses arising from credit-related factors with respect to AFS and HTM securities are included in the determination of net income. The cost of securities sold is determined using the specific-identification method.
Our investment policy requires that all of our investments have final maturities of less than 10 years, or less than 10 years average life for structured securities. Investments and restricted investments are subject to interest rate risk and will decrease in value if market rates increase. Declines in interest rates over time will reduce our investment income.
In general, our AFS securities are classified as current assets without regard to the securities’ contractual maturity dates because they may be readily liquidated. We monitor our investments for credit-related impairment. For comprehensive discussions of the fair value and classification of our investments, see Note 5, “Fair Value Measurements,” and Note 6, “Investments.”
Accrued interest receivable relating to our AFS and HTM securities is presented within “Prepaid expenses and other current assets” in the accompanying consolidated balance sheets, and amounted to $11 million and $10 million at December 31, 2021, and 2020, respectively. We do not measure an allowance for credit losses on accrued interest receivable. Instead, we write off accrued interest receivable that has not been collected within 90 days of the interest payment due date. We recognize such write offs as a reversal of interest income. No accrued interest was written off during the year ended December 31, 2021.
Molina Healthcare, Inc. 2021 Form 10-K | 55
Receivables
Receivables consist primarily of premium amounts due from government agencies, which are subject to potential retroactive adjustments. Because substantially all of our receivable amounts are readily determinable and substantially all of our creditors are governmental authorities, our allowance for credit losses is insignificant. Any amounts determined to be uncollectible are charged to expense when such determination is made.
| | | | | | | | | | | |
| December 31, |
| 2021 | | 2020 |
| | | |
| (In millions) |
| Government receivables | $ | 1,566 | | | $ | 969 | |
| Pharmacy rebate receivables | 276 | | | 178 | |
| Health insurer fee reimbursement receivables | — | | | 104 | |
| Other | 335 | | | 255 | |
| Magellan Complete Care acquisition opening balance | — | | | 166 | |
| Total | $ | 2,177 | | | $ | 1,672 | |
Business Combinations
We account for business combinations using the acquisition method of accounting, which requires us to recognize the assets acquired and the liabilities assumed at their acquisition date fair values. As discussed below, the excess of the purchase consideration transferred over the fair value of the net tangible and intangible assets acquired is recorded as goodwill. While we use our best estimates and assumptions to accurately value assets acquired and liabilities assumed at the acquisition date, our estimates are inherently uncertain and subject to refinement. As a result, during the measurement period, which may be up to one year from the acquisition date, we may record adjustments to the assets acquired and liabilities assumed with the corresponding offset to goodwill. Upon the conclusion of the final determination of the values of assets acquired or liabilities assumed, or one year after the date of acquisition, whichever comes first, any subsequent adjustments are recorded within our consolidated results of operations.
The purchase price for the acquisition of certain assets of Passport Health Plan, Inc. in 2020 included contingent consideration payable to seller relating to guarantees for minimum operating income in the post-acquisition period in 2020 and minimum membership targets in 2021. The liabilities are recorded at fair value on a recurring basis, which totaled $47 million as of December 31, 2021. The contingent purchase consideration paid is presented primarily in “Financing activities” in the accompanying consolidated statements of cash flows for the year ended December 31, 2021, with the balance reflected in “Operating activities.” We expect to pay the remaining balance of the liabilities, reported in “Accounts payable, accrued liabilities and other” in the accompanying consolidated balance sheets, in 2022.
Refer to Note 4, “Business Combinations,” and Note 9, “Goodwill and Intangible Assets, Net,” for further details.
Long-Lived Assets, including Intangible Assets
Long-lived assets consist primarily of property, equipment, capitalized software (see Note 7, “Property, Equipment, and Capitalized Software, Net”), and intangible assets resulting from acquisitions. Finite-lived, separately-identified intangible assets acquired in business combinations are assets that represent future expected benefits but lack physical substance (such as purchased contract rights and provider contracts). Intangible assets are initially recorded at fair value and are then amortized on a straight-line basis over their expected useful lives, generally between five and 16 years.
Determining the fair value of identifiable assets acquired, particularly intangible assets, and liabilities assumed, requires management to make estimates, which are based on all available information and in some cases assumptions with respect to the timing and amount of future revenues and expenses associated with an asset. Determining the useful life of an intangible asset also requires judgment, as different types of intangible assets will have different useful lives. The most significant intangible asset we typically record in a business combination is contract rights associated with membership assumed. In determining the estimated fair value of the intangible assets, we typically apply the income approach, which discounts the projected future net cash flows using an appropriate discount rate that reflects the risk associated with such projected future cash flows. The most critical assumptions used in determining the fair value of contract rights include forecasted operating margins and the weighted average cost of capital.
Molina Healthcare, Inc. 2021 Form 10-K | 56
Our intangible assets are subject to impairment tests when events or circumstances indicate that a finite-lived intangible asset’s (or asset group’s) carrying value may not be recoverable. Consideration is given to a number of potential impairment indicators, including the ability of our health plan subsidiaries to obtain the renewal by amendment of their contracts in each state prior to the actual expiration of their contracts. However, there can be no assurance that these contracts will continue to be renewed. Following the identification of any potential impairment indicators, to determine whether an impairment exists, we would compare the carrying amount of a finite-lived intangible asset with the greater of the undiscounted cash flows that are expected to result from the use of the asset or related group of assets, or its value under the asset liquidation method. If it is determined that the carrying amount of the asset is not recoverable, the amount by which the carrying value exceeds the estimated fair value is recorded as an impairment. Refer to Note 9, “Goodwill and Intangible Assets, Net,” for further details.
Goodwill
Goodwill represents the excess of the purchase consideration over the fair value of net assets acquired in business combinations. Goodwill is not amortized but is tested for impairment on an annual basis and more frequently if impairment indicators are present. Impairment indicators may include experienced or expected operating cash-flow deterioration or losses, significant losses of membership, loss of state funding, loss of state contracts, and other factors. Goodwill is impaired if the carrying amount of the reporting unit exceeds its estimated fair value. This excess is recorded as an impairment loss and adjusted if necessary for the impact of tax-deductible goodwill. The loss recognized may not exceed the total goodwill allocated to the reporting unit.
When testing goodwill for impairment, we may first assess qualitative factors, such as industry and market factors, the dynamic economic and political environments in which we operate, cost factors, and changes in overall performance, to determine if it is more likely than not that the carrying value of our reporting units exceed their estimated fair values. If our qualitative assessment indicates that it is more likely than not that the carrying value of a reporting unit exceeds its estimated fair value, we perform the quantitative assessment. We may also elect to bypass the qualitative assessment and proceed directly to the quantitative assessment. We performed a qualitative goodwill assessment of our reporting units, which resulted in no goodwill impairment losses in the year ended December 31, 2021.
If performing a quantitative assessment, we generally estimate the fair values of our reporting units by applying the income approach, using discounted cash flows. The base year in the reporting units’ discounted cash flows is derived from the annual financial planning cycle, which commences in the fourth quarter of the year. As part of a quantitative assessment, we may also apply the asset liquidation method to estimate the fair value of individual reporting units, which is computed as total assets minus total liabilities, excluding intangible assets and deferred taxes. Finally, we apply a market approach to reconcile the value of our reporting units to our consolidated market value. Under the market approach, we consider publicly traded comparable company information to determine revenue and earnings multiples which are used to estimate our reporting units’ fair values. The assumptions used are consistent with those used in our long-range business plan and annual planning process. However, if these assumptions differ from actual results, the outcome of our goodwill impairment tests could be adversely affected.
Leases
Right-of-use (“ROU”) assets represent our right to use the underlying assets over the lease term, and lease liabilities represent our obligation for lease payments arising from the related leases. ROU assets and lease liabilities are recognized at the lease commencement date based on the present value of lease payments over the lease term. Lease terms may include options to extend or terminate the lease when we believe it is reasonably certain that we will exercise such options. If applicable, we account for lease and non-lease components within a lease as a single lease component.
Because most of our leases do not provide an implicit interest rate, we generally use our incremental borrowing rate to determine the present value of lease payments. Lease expenses for operating lease payments are recognized on a straight-line basis over the lease term, and the related ROU assets and liabilities are reduced to the present value of the remaining lease payments at the end of each period. Finance lease payments reduce finance lease liabilities, the related ROU assets are amortized on a straight-line basis over the lease term, and interest expense is recognized using the effective interest method.
The significant majority of our operating leases consist of long-term operating leases for office space. Short-term leases (those with terms of 12 months or less) are not recorded as ROU assets or liabilities in the consolidated balance sheets. For certain leases that represent a portfolio of similar assets, such as a fleet of vehicles, we apply a portfolio approach to account for the related ROU assets and liabilities, rather than account for such assets and the related liabilities individually. A nominal number of our lease agreements include rental payments that adjust
Molina Healthcare, Inc. 2021 Form 10-K | 57
periodically for inflation. Our lease agreements do not contain any material residual value guarantees or material restrictive covenants.
For further information, including the amount and location of the ROU assets and lease liabilities recognized in the accompanying consolidated balance sheets, see Note 8, “Leases.”
Medical Claims and Benefits Payable
Medical care costs are recognized in the period in which services are provided and include fee-for-service claims, pharmacy benefits, capitation payments to providers, and various other medically-related costs. Under fee-for-service claims arrangements with providers, we retain the financial responsibility for medical care provided and incur costs based on actual utilization of hospital and physician services. Such medical care costs include amounts paid by us as well as estimated medical claims and benefits payable for costs that were incurred but not paid as of the reporting date (“IBNP”). Pharmacy benefits represent payments for members' prescription drug costs, net of rebates from drug manufacturers. We estimate pharmacy rebates based on historical and current utilization of prescription drugs and contractual provisions. Capitation payments represent monthly contractual fees paid to providers, who are responsible for providing medical care to members, which could include medical or ancillary costs like dental, vision and other supplemental health benefits. Such capitation costs are fixed in advance of the periods covered and are not subject to significant accounting estimates. Other medical care costs include all medically-related administrative costs, amounts due to providers pursuant to risk-sharing or other incentive arrangements, provider claims, and other healthcare expenses. Examples of medically-related administrative costs include expenses relating to health education, quality assurance, case management, care coordination, disease management, and 24-hour on-call nurses. Additionally, we include an estimate for the cost of settling claims incurred through the reporting date in our medical claims and benefits payable liability.
Medical claims and benefits payable consist mainly of fee-for-service IBNP, unpaid pharmacy claims, capitation costs, other medical costs, including amounts payable to providers pursuant to risk-sharing or other incentive arrangements and amounts payable to providers on behalf of certain state agencies for certain state assessments in which we assume no financial risk. IBNP includes the costs of claims incurred as of the balance sheet date which have been reported to us, and our best estimate of the cost of claims incurred but not yet reported to us. We also include an additional reserve to ensure that our overall IBNP liability is sufficient under moderately adverse conditions. We reflect changes in these estimates in the consolidated results of operations in the period in which they are determined.
The estimation of the IBNP liability requires a significant degree of judgment in applying actuarial methods, determining the appropriate assumptions and considering numerous factors. Of those factors, we consider estimated completion factors and the assumed healthcare cost trend to be the most critical assumptions. Other relevant factors also include, but are not limited to, healthcare service utilization trends, claim inventory levels, changes in membership, product mix, seasonality, benefit changes or changes in Medicaid fee schedules, provider contract changes, prior authorizations and the incidence of catastrophic or pandemic cases.
Because of the significant degree of judgment involved in estimation of our IBNP liability, there is considerable variability and uncertainty inherent in such estimates. Each reporting period, the recognized IBNP liability represents our best estimate of the total amount of unpaid claims incurred as of the balance sheet date using a consistent methodology in estimating our IBNP liability. We believe our current estimates are reasonable and adequate; however, the development of our estimate is a continuous process that we monitor and update as more complete claims payment information and healthcare cost trend data becomes available. Actual medical care costs may be less than we previously estimated (favorable development) or more than we previously estimated (unfavorable development), and any differences could be material. Any adjustments to reflect favorable development would be recognized as a decrease to medical care costs, and any adjustments to reflect unfavorable development would be recognized as an increase to medical care costs, in the period in which the adjustments are determined.
Refer to Note 10, “Medical Claims and Benefits Payable,” for a table presenting the components of the change in our medical claims and benefits payable, for all periods presented in the accompanying consolidated financial statements.
Premium Revenue Recognition and Amounts Due Government Agencies
Premium revenue is generated from our contracts with state and federal agencies, in connection with our participation in the Medicaid, Medicare, and Marketplace programs. Premium revenue is generally received based on per member per month (“PMPM”) rates established in advance of the periods covered. These premium revenues are recognized in the month that members are entitled to receive healthcare services, and premiums collected in advance are deferred. State Medicaid programs and the federal Medicare program periodically adjust premium
Molina Healthcare, Inc. 2021 Form 10-K | 58
rates.
Certain components of premium revenue are subject to accounting estimates and are described below, under “Contractual Provisions That May Adjust or Limit Revenue or Profit,” and “Quality Incentives.”
Contractual Provisions That May Adjust or Limit Revenue or Profit
Many of our contracts contain provisions that may adjust or limit revenue or profit, as described below. Consequently, we recognize premium revenue as it is earned under such provisions. Liabilities accrued for premiums to be returned under such provisions are reported in the aggregate as “Amounts due government agencies” in the accompanying consolidated balance sheets. Categorized by program, such amounts due government agencies included the following:
| | | | | | | | | | | |
| December 31, |
| 2021 | | 2020 |
| | | |
| (In millions) |
| Medicaid program: | | | |
| Minimum MLR and profit sharing | $ | 1,016 | | | $ | 513 | |
| Other | 263 | | | 76 | |
| Medicare program: | | | |
| Risk adjustment and Part D risk sharing | 89 | | | 45 | |
| Minimum MLR and profit sharing | 101 | | | 62 | |
| Other | 35 | | | 30 | |
| Marketplace program: | | | |
| Risk adjustment | 902 | | | 326 | |
| Minimum MLR | 18 | | | 37 | |
| Other | 48 | | | 21 | |
| Magellan Complete Care acquisition opening balance | — | | | 143 | |
| Total amounts due government agencies | $ | 2,472 | | | $ | 1,253 | |
Medicaid Program
Minimum MLR and Medical Cost Corridors. A portion of our premium revenue may be returned if certain minimum amounts are not spent on defined medical care costs. Under certain medical cost corridor provisions, the health plans may receive additional premiums if amounts spent on medical care costs exceed a defined maximum threshold.
Profit Sharing. Our contracts with certain states contain profit sharing provisions under which we refund amounts to the states if our health plans generate profit above a certain specified percentage. In some cases, we are limited in the amount of administrative costs that we may deduct in calculating the refund, if any.
Retroactive Premium Adjustments. State Medicaid programs periodically adjust premium rates on a retroactive basis. In these cases, we adjust our premium revenue in the period in which we determine that the adjustment is probable and reasonably estimable, based on our best estimate of the ultimate premium we expect to realize for the period being adjusted.
Beginning in 2020, through December 31, 2021, various states enacted temporary risk corridors in response to the reduced demand for medical services stemming from COVID-19, which have resulted in a reduction of our medical margin, primarily in the Medicaid segment. In some cases, these risk corridors were retroactive to earlier periods in 2020, or as early as the beginning of the states’ fiscal years in 2019. Beginning in the second quarter of 2020, we have recognized retroactive risk corridors that we believe to be probable, and where the ultimate premium amount is reasonably estimable. We recognized approximately $323 million related to such risk corridors in 2021, primarily in the Medicaid segment. Approximately $564 million related to these COVID-related risk corridors, in the aggregate, were recognized in 2020, including $37 million related to MMP plans.
It is possible that certain states could change the structure of existing risk corridors, implement new risk corridors in the future or discontinue existing risk corridors. Due to these uncertainties, the ultimate outcomes could differ materially from our estimates as a result of changes in facts or further developments, which could have an adverse effect on our consolidated financial position, results of operations, or cash flows.
Molina Healthcare, Inc. 2021 Form 10-K | 59
Medicare Program
Risk Adjustment. Our Medicare premiums are subject to retroactive increase or decrease based on the health status of our Medicare members (as measured by member risk score). We estimate our members’ risk scores and the related amount of Medicare revenue that will ultimately be realized for the periods presented based on our knowledge of our members’ health status, risk scores and Centers for Medicare & Medicaid Services (“CMS”) practices.
Minimum MLR. The Affordable Care Act (“ACA”) established a minimum annual medical loss ratio (“Minimum MLR”) of 85% for Medicare. The medical loss ratio represents medical costs as a percentage of premium revenue. Federal regulations define what constitutes medical costs and premium revenue. If the Minimum MLR is not met, we may be required to pay rebates to the federal government. We recognize estimated rebates under the Minimum MLR as an adjustment to premium revenue in our consolidated statements of income.
Marketplace Program
Risk Adjustment. Under this program, our health plans’ composite risk scores are compared with the overall average risk score for the relevant state and market pool. Generally, our health plans will make a risk adjustment payment into the pool if their composite risk scores are below the average risk score (risk adjustment payable), and will receive a risk adjustment payment from the pool if their composite risk scores are above the average risk score (risk adjustment receivable). We estimate our ultimate premium based on insurance policy year-to-date experience, and recognize estimated premiums relating to the risk adjustment program as an adjustment to premium revenue in our consolidated statements of income. As of December 31, 2021, Marketplace risk adjustment payables amounted to $902 million and related receivables amounted to $7 million, for a net payable of $895 million. As of December 31, 2020, Marketplace risk adjustment payables amounted to $326 million and related receivables amounted to $20 million, for a net payable of $306 million.
Minimum MLR. The ACA has established a Minimum MLR of 80% for the Marketplace. If the Minimum MLR is not met, we may be required to pay rebates to our Marketplace policyholders. The Marketplace risk adjustment program is taken into consideration when computing the Minimum MLR. We recognize estimated rebates under the Minimum MLR as an adjustment to premium revenue in our consolidated statements of income.
Quality Incentives
At many of our health plans, revenue ranging from approximately 1% to 4% of certain health plan premiums is earned only if certain performance measures are met. Such performance measures are generally found in our Medicaid and MMP contracts. Recognition of quality incentive premium revenue is subject to the use of estimates.
Reinsurance
We bear underwriting and reserving risks associated with our health plan subsidiaries. In certain cases, we limit our risk of significant catastrophic losses by maintaining high deductible reinsurance coverage with a highly-rated, unaffiliated insurance company (the “third-party reinsurer”). Because we remain liable for losses in the event the third-party reinsurer is unable to pay its portion of the losses, we continually monitor the third-party reinsurer’s financial condition, including its ability to maintain high credit ratings. Intercompany transactions with our captive are eliminated in consolidation.
We report reinsurance premiums as a reduction to premium revenue, while related reinsurance recoveries are reported as a reduction to medical care costs. Reinsurance premiums amounted to $2 million, $9 million, and $17 million for the years ended December 31, 2021, 2020, and 2019, respectively. Reinsurance recoveries amounted to $33 million, $23 million, and $18 million for the years ended December 31, 2021, 2020, and 2019, respectively. Reinsurance recoverable of $51 million, $30 million, and $21 million, as of December 31, 2021, 2020, and 2019, respectively, is included in “Receivables” in the accompanying consolidated balance sheets.
Premium Deficiency Reserves on Loss Contracts
We assess the profitability of our contracts to determine if it is probable that a loss will be incurred in the future by reviewing current results and forecasts. For purposes of this assessment, contracts are grouped in a manner consistent with our method of acquiring, servicing and measuring the profitability of such contracts. A premium deficiency reserve (“PDR”) is recognized if anticipated future medical care and administrative costs exceed anticipated future premium revenue, investment income and reinsurance recoveries.
Molina Healthcare, Inc. 2021 Form 10-K | 60
Income Taxes
We account for income taxes under the asset and liability method. Deferred tax assets and liabilities are determined based on the difference between the financial statement and tax bases of assets and liabilities using enacted tax rates expected to be in effect during the year in which the basis differences reverse. Valuation allowances are established when management determines it is more likely than not that some portion, or all, of the deferred tax assets will not be realized. For further discussion and disclosure, see Note 12, “Income Taxes.”
Taxes Based on Premiums
Health Insurer Fee (“HIF”). Under the Affordable Care Act, the federal government imposed an annual fee, or excise tax, on health insurers for each calendar year (the “HIF”). The Further Consolidated Appropriations Act, 2020 repealed the HIF effective for years after 2020.
Premium and Use Tax. Certain of our health plans are assessed a tax based on premium revenue collected. The premium revenues we receive from these states include reimbursement for the premium tax assessment. We have reported these taxes on a gross basis, as premium tax revenue and as premium tax expenses in the consolidated statements of income.
Concentrations of Credit Risk
Financial instruments that potentially subject us to concentrations of credit risk consist primarily of cash and cash equivalents, investments, receivables, and restricted investments. Our investments and a portion of our cash equivalents are managed by professional portfolio managers operating under documented investment guidelines. Our portfolio managers must obtain our prior approval before selling investments where the loss position of those investments exceeds certain levels. Our investments consist primarily of investment-grade debt securities with final maturities of less than 10 years, or less than 10 years average life for structured securities. Restricted investments are invested principally in cash, cash equivalents and U.S. Treasury securities. Concentration of credit risk with respect to accounts receivable is limited because our payors consist principally of the federal government, and governments of each state in which our health plan subsidiaries operate.
Risks and Uncertainties
Our profitability depends in large part on our ability to accurately predict and effectively manage medical care costs. We continually review our medical costs in light of our underlying claims experience and revised actuarial data. However, several factors could adversely affect medical care costs. These factors, which include changes in healthcare practices, inflation, new technologies, major epidemics, natural disasters, and malpractice litigation, are beyond our control and may have an adverse effect on our ability to accurately predict and effectively control medical care costs. Costs in excess of those anticipated could have a material adverse effect on our financial condition, results of operations, or cash flows.
We operate health plans primarily as a direct contractor with the states, and in Los Angeles County, California, as a subcontractor to another health plan holding a direct contract with the state. We are therefore dependent upon a relatively small number of contracts to support our revenue. The loss of any one of those contracts could have a material adverse effect on our financial position, results of operations, or cash flows. In addition, our ability to arrange for the provision of medical services to our members is dependent upon our ability to develop and maintain adequate provider networks. Our inability to develop or maintain such networks might, in certain circumstances, have a material adverse effect on our financial position, results of operations, or cash flows.
Molina Healthcare, Inc. 2021 Form 10-K | 61
The following table summarizes premium revenue by state health plan for the periods presented:
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| Amount | | % of Total | | Amount | | % of Total | | Amount | | % of Total |
| | | | | | | | | | | |
| (Dollars in millions) |
| California | $ | 2,402 | | | 8.9 | % | | $ | 2,109 | | | 11.5 | % | | $ | 2,266 | | | 14.0 | % |
| Florida | 970 | | | 3.6 | | | 643 | | | 3.5 | | | 734 | | | 4.5 | |
| Illinois | 1,860 | | | 6.9 | | | 1,328 | | | 7.3 | | | 1,002 | | | 6.2 | |
| Kentucky | 1,977 | | | 7.4 | | | 654 | | | 3.6 | | | — | | | — | |
| Michigan | 1,915 | | | 7.1 | | | 1,587 | | | 8.7 | | | 1,624 | | | 10.0 | |
| New York | 1,429 | | | 5.3 | | | 309 | | | 1.7 | | | 179 | | | 1.1 | |
| Ohio | 3,172 | | | 11.8 | | | 2,962 | | | 16.2 | | | 2,553 | | | 15.8 | |
| Texas | 3,959 | | | 14.8 | | | 3,085 | | | 16.9 | | | 2,991 | | | 18.5 | |
| Washington | 4,420 | | | 16.5 | | | 3,169 | | | 17.3 | | | 2,695 | | | 16.6 | |
Other (1) | 4,751 | | | 17.7 | | | 2,453 | | | 13.3 | | | 2,164 | | | 13.3 | |
| Total | $ | 26,855 | | | 100.0 | % | | $ | 18,299 | | | 100.0 | % | | $ | 16,208 | | | 100.0 | % |
_______________________
(1)“Other” includes the Idaho, Mississippi, New Mexico, Puerto Rico, South Carolina, Utah and Wisconsin health plans, which were individually immaterial to our consolidated results of operations.
Recent Accounting Pronouncements
Recent accounting pronouncements issued by the FASB (including its Emerging Issues Task Force), the American Institute of Certified Public Accountants, and the Securities and Exchange Commission (“SEC”) did not have, nor does management expect such pronouncements to have, a significant impact on our present or future consolidated financial statements.
3. Net Income Per Share
The following table sets forth the calculation of basic and diluted net income per share:
| | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | |
| (In millions, except net income per share) |
| Numerator: | | | | | |
| Net income | $ | 659 | | | $ | 673 | | | $ | 737 | |
| Denominator: | | | | | |
| Shares outstanding at the beginning of the period | 58.0 | | | 61.9 | | | 62.1 | |
| Weighted-average number of shares issued: | | | | | |
| Stock purchases | (0.5) | | | (3.0) | | | — | |
| Stock-based compensation | 0.3 | | | 0.1 | | | 0.1 | |
| Denominator for basic net income per share | 57.8 | | | 59.0 | | | 62.2 | |
Effect of dilutive securities: (1) | | | | | |
| Stock-based compensation | 0.8 | | | 0.9 | | | 0.6 | |
| Warrants | — | | | — | | | 1.4 | |
| Denominator for diluted net income per share | 58.6 | | | 59.9 | | | 64.2 | |
| | | | | |
Net income per share - Basic (2) | $ | 11.40 | | | $ | 11.40 | | | $ | 11.85 | |
Net income per share - Diluted (2) | $ | 11.25 | | | $ | 11.23 | | | $ | 11.47 | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
_______________________________
Molina Healthcare, Inc. 2021 Form 10-K | 62
(1) The dilutive effect of all potentially dilutive common shares is calculated using the treasury stock method. Certain potentially dilutive common shares issuable are not included in the computation of diluted net income per share because to do so would have been anti-dilutive.
(2) Source data for calculations in thousands.
4. Business Combinations
In the fourth quarter of 2021, we closed on one business combination in the Medicaid segment, consistent with our strategy to grow in our existing markets. For this transaction, we applied the acquisition method of accounting, where the total purchase price was allocated, or preliminarily allocated, to the tangible and intangible assets acquired and liabilities assumed, based on their fair values as of the acquisition date. We expect to complete the final determination of the purchase price allocation as soon as practicable, but no later than one year following the acquisition’s closing date in accordance with Accounting Standards Codification Topic 805, Business Combinations. Measurement period adjustments will be recorded in the period in which they are determined, as if they had been completed at the acquisition date.
Acquisition costs amounted to $34 million in the aggregate for the year ended December 31, 2021, and were recorded as “General and administrative expenses” in the accompanying consolidated statements of income.
Affinity. On October 25, 2021, we closed on our acquisition of substantially all of the assets of Affinity Health Plan, Inc., a Medicaid health plan in New York, for initial purchase consideration of approximately $176 million. Finalization of purchase price adjustments as provided in the asset purchase agreement is expected to occur in the second half of 2022.
Goodwill is calculated as the excess of the consideration transferred over the net assets recognized and represents the estimated future economic benefits arising from other assets acquired that could not be individually identified and separately recognized. Such assets include synergies we expect to achieve, such as the use of our existing infrastructure to support the added membership, and future economic benefits arising from the assembled workforce. Approximately 100% of the goodwill is deductible for income tax purposes. The following table summarizes the provisional fair values assigned to assets acquired and liabilities assumed, in millions.
| | | | | |
| |
| |
| |
| Assets acquired: | |
| Current assets | $ | 234 | |
| Goodwill | 280 | |
| Intangible assets | 69 | |
| Other long-term assets | 8 | |
| Liabilities assumed: | |
| Medical claims and benefits payable | (224) | |
| Amounts due government agencies | (155) | |
| Accounts payable, accrued and other long-term liabilities | (36) | |
| Net consideration transferred | $ | 176 | |
| |
The table below presents intangible assets acquired, by major class, for the Affinity acquisition. The weighted-average amortization period, in the aggregate, is 5.4 years.
| | | | | | | | | | | |
| Fair Value | | Life |
| | | |
| | (In millions) | | (Years) |
| Contract rights - member list | $ | 56 | | | 5 |
| Provider network | 9 | | | 10 |
| Trade name | 4 | | | 1.5 |
| $ | 69 | | | |
| | | |
Magellan Complete Care. On December 31, 2020, we closed on our acquisition of 100% of the outstanding equity interests of the Magellan Complete Care line of business of Magellan Health, Inc., for initial purchase consideration of approximately $1,037 million. In the fourth quarter of 2021, we paid additional purchase consideration of $28 million as a result of final purchase price adjustments as provided in the stock and asset purchase agreement. In the year ended December 31, 2021, we recorded various measurement period adjustments, including a decrease
Molina Healthcare, Inc. 2021 Form 10-K | 63
of $7 million to “Receivables,” a decrease of $27 million to “Medical claims and benefits payable,” and an increase of $18 million to “Amounts due government agencies.” In the aggregate, we recorded a net increase of $10 million to goodwill for these measurement period adjustments and purchase price adjustments, which has been finalized as of December 31, 2021.
Cigna. As described in Note 1, “Organization and Basis of Presentation,” we announced this acquisition closed on January 1, 2022. Because the closing date fell on a holiday, the $58 million purchase price was paid on December 31, 2021 and was recorded to prepaid expenses and other assets. Such amounts are reported in investing activities in the accompanying consolidated statements of cash flows. The initial accounting for this transaction is incomplete.
5. Fair Value Measurements
We consider the carrying amounts of current assets and current liabilities to approximate their fair values because of the relatively short period of time between the origination of these instruments and their expected realization or payment. For our financial instruments measured at fair value on a recurring basis, we prioritize the inputs used in measuring fair value according to a three-tier fair value hierarchy as follows:
Level 1 — Observable Inputs. Level 1 financial instruments are actively traded and therefore the fair value for these securities is based on quoted market prices for identical securities in active markets.
Level 2 — Directly or Indirectly Observable Inputs. Fair value for these investments is determined using a market approach based on quoted prices for similar securities in active markets or quoted prices for identical securities in inactive markets.
Level 3 — Unobservable Inputs. Level 3 financial instruments are valued using unobservable inputs that represent management’s best estimate of what market participants would use in pricing the financial instrument at the measurement date. As of December 31, 2021 and 2020, our Level 3 financial instruments consisted of contingent consideration liabilities.
The net changes in fair value of Level 3 financial instruments are reported in “Other” operating expenses in our consolidated statements of income. In the years ended December 31, 2021 and 2020, we recognized a loss of $24 million and $6 million, respectively, primarily for the increase in the fair value of the contingent consideration liability described below.
Our financial instruments measured at fair value on a recurring basis at December 31, 2021, were as follows:
| | | | | | | | | | | | | | | | | | | | | | | |
| Total | | Level 1 | | Level 2 | | Level 3 |
| | | | | | | |
| | (In millions) |
| Corporate debt securities | $ | 1,833 | | | $ | — | | | $ | 1,833 | | | $ | — | |
| Mortgage-backed securities | 614 | | | — | | | 614 | | | — | |
| U.S. Treasury notes | 353 | | | — | | | 353 | | | — | |
| Asset-backed securities | 247 | | | — | | | 247 | | | — | |
| Municipal securities | 123 | | | — | | | 123 | | | — | |
| | | | | | | |
| | | | | | | |
Other | 32 | | | — | | | 32 | | | — | |
| Total assets | $ | 3,202 | | | $ | — | | | $ | 3,202 | | | $ | — | |
| | | | | | | |
| Contingent consideration liabilities | $ | 47 | | | $ | — | | | $ | — | | | $ | 47 | |
| Total liabilities | $ | 47 | | | $ | — | | | $ | — | | | $ | 47 | |
Molina Healthcare, Inc. 2021 Form 10-K | 64
Our financial instruments measured at fair value on a recurring basis at December 31, 2020, were as follows:
| | | | | | | | | | | | | | | | | | | | | | | |
| Total | | Level 1 | | Level 2 | | Level 3 |
| | | | | | | |
| | (In millions) |
| Corporate debt securities | $ | 1,256 | | | $ | — | | | $ | 1,256 | | | $ | — | |
| Mortgage-backed securities | 392 | | | — | | | 392 | | | — | |
| U.S. Treasury notes | 27 | | | — | | | 27 | | | — | |
| Asset-backed securities | 132 | | | — | | | 132 | | | — | |
| Municipal securities | 68 | | | — | | | 68 | | | — | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| Total assets | $ | 1,875 | | | $ | — | | | $ | 1,875 | | | $ | — | |
| | | | | | | |
| Contingent consideration liabilities | $ | 46 | | | $ | — | | | $ | — | | | $ | 46 | |
| Total liabilities | $ | 46 | | | $ | — | | | $ | — | | | $ | 46 | |
Level 3 Contingent Consideration Liabilities
Our Level 3 financial instruments at December 31, 2021 are comprised solely of contingent consideration liabilities of $47 million, in connection with our 2020 acquisition of certain assets of Passport Health Plan, Inc., a Medicaid health plan in Kentucky. Refer to Note 2, “Significant Accounting Policies—Business Combinations”, for further details. The liabilities are recorded at fair value on a recurring basis. In 2021, the estimated fair value of contingent purchase consideration increased by approximately $24 million, mainly relating to an operating income guarantee, and was essentially offset by $23 million paid to the seller for half the consideration due for minimum member enrollment targets in 2021. In January 2022, we paid the remaining half of the consideration due for minimum member enrollment targets of $23 million.
Fair Value Measurements – Disclosure Only
The carrying amounts and estimated fair values of our notes payable are classified as Level 2 financial instruments. Fair value for these securities is determined using a market approach based on quoted market prices for similar securities in active markets or quoted prices for identical securities in inactive markets.
| | | | | | | | | | | | | | | | | | | | | | | |
| | December 31, 2021 | | December 31, 2020 |
| | Carrying
Amount | | Fair Value | | Carrying
Amount | | Fair Value |
| | | | | | | |
| | (In millions) |
5.375% Notes due 2022 (1) | $ | — | | | $ | — | | | $ | 697 | | | $ | 742 | |
4.375% Notes due 2028 | 791 | | | 829 | | | 789 | | | 843 | |
3.875% Notes due 2030 | 642 | | | 675 | | | 641 | | | 691 | |
3.875% Notes due 2032 | 740 | | | 760 | | | — | | | — | |
| Total | $ | 2,173 | | | $ | 2,264 | | | $ | 2,127 | | | $ | 2,276 | |
_______________________________
(1) For more information on debt repayments, refer to Note 11, “Debt.”
Molina Healthcare, Inc. 2021 Form 10-K | 65
6. Investments
Available-for-Sale
We consider all of our investments classified as current assets to be available-for-sale. The following tables summarize our current investments as of the dates indicated:
| | | | | | | | | | | | | | | | | | | | | | | |
| December 31, 2021 |
| Amortized
Cost | | Gross
Unrealized | | Estimated
Fair Value |
| | Gains | | Losses | |
| | | | | | | |
| (In millions) |
| Corporate debt securities | $ | 1,836 | | | $ | 9 | | | $ | 12 | | | $ | 1,833 | |
| Mortgage-backed securities | 616 | | | 2 | | | 4 | | | 614 | |
U.S. Treasury notes | 353 | | | — | | | — | | | 353 | |
| Asset-backed securities | 248 | | | — | | | 1 | | | 247 | |
| Municipal securities | 123 | | | 1 | | | 1 | | | 123 | |
| | | | | | | |
| | | | | | | |
| Other | 32 | | | — | | | — | | | 32 | |
| Total | $ | 3,208 | | | $ | 12 | | | $ | 18 | | | $ | 3,202 | |
| | | | | | | | | | | | | | | | | | | | | | | |
| December 31, 2020 |
| Amortized
Cost | | Gross
Unrealized | | Estimated
Fair Value |
| | Gains | | Losses | |
| | | | | | | |
| (In millions) |
| Corporate debt securities | $ | 1,220 | | | $ | 36 | | | $ | — | | | $ | 1,256 | |
| Mortgage-backed securities | 383 | | | 10 | | | 1 | | | 392 | |
U.S. Treasury notes | 27 | | | — | | | — | | | 27 | |
| Asset-backed securities | 130 | | | 2 | | | — | | | 132 | |
| Municipal securities | 66 | | | 2 | | | — | | | 68 | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| Total | $ | 1,826 | | | $ | 50 | | | $ | 1 | | | $ | 1,875 | |
The contractual maturities of our current investments as of December 31, 2021 are summarized below:
| | | | | | | | | | | |
| Amortized
Cost | | Estimated
Fair Value |
| | | |
| (In millions) |
| Due in one year or less | $ | 665 | | | $ | 667 | |
| Due after one year through five years | 1,667 | | | 1,662 | |
| Due after five years through ten years | 335 | | | 335 | |
| Due after ten years | 541 | | | 538 | |
| Total | $ | 3,208 | | | $ | 3,202 | |
Gross realized gains and losses from sales of available-for-sale securities are calculated under the specific identification method and are included in investment income. Gross realized investment gains amounted to $10 million, $6 million and $13 million in the years ended December 31, 2021, 2020 and 2019, respectively. Gross realized investment losses were insignificant in the years ended December 31, 2021, 2020 and 2019.
We have determined that unrealized losses at December 31, 2021 and 2020 primarily resulted from fluctuating interest rates, rather than a deterioration of the creditworthiness of the issuers. Therefore, we determined that an allowance for credit losses was not necessary. So long as we maintain the intent and ability to hold these securities to maturity, we are unlikely to experience losses. In the event that we dispose of these securities before maturity, we expect that realized losses, if any, will be insignificant.
Molina Healthcare, Inc. 2021 Form 10-K | 66
The following table summarizes those available-for-sale investments that have been in a continuous loss position for less than 12 months. No investments have been in a continuous loss position for 12 months or more as of December 31, 2021, and 2020.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| In a Continuous Loss Position for Less than 12 Months as of December 31, 2021 | | In a Continuous Loss Position for Less than 12 Months as of December 31, 2020 |
| Estimated
Fair Value | | Unrealized
Losses | | Total Number of Positions | | Estimated
Fair Value | | Unrealized
Losses | | Total Number of Positions |
| | | | | | | | | | | |
| | (Dollars in millions) |
| Corporate debt securities | $ | 1,063 | | | $ | 12 | | | 395 | | | $ | — | | | $ | — | | | — | |
Mortgage-backed securities | 408 | | | 4 | | | 146 | | | 77 | | | 1 | | | 21 | |
| Asset-backed securities | 166 | | | 1 | | | 75 | | | — | | | — | | | — | |
| | | | | | | | | | | |
| Municipal securities | 69 | | | 1 | | | 61 | | | — | | | — | | | — | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Total | $ | 1,706 | | | $ | 18 | | | 677 | | | $ | 77 | | | $ | 1 | | | 21 | |
Restricted Investments Held-to-Maturity
Pursuant to the regulations governing our state health plan subsidiaries, we maintain statutory deposits and deposits required by government authorities primarily in cash, cash equivalents, and U.S. Treasury securities. We also maintain restricted investments as protection against the insolvency of certain capitated providers. The use of these funds is limited as required by regulations in the various states in which we operate, or as needed in the event of insolvency of capitated providers. Therefore, such investments are reported as “Restricted investments” in the accompanying consolidated balance sheets.
We have the ability to hold these restricted investments until maturity, and as a result, we would not expect the value of these investments to decline significantly due to a sudden change in market interest rates. Our held-to-maturity restricted investments are carried at amortized cost, which approximates fair value, of which $142 million will mature in one year or less, and $70 million will mature in one through five years.
The following table presents the balances of restricted investments:
| | | | | | | | | | | |
| December 31, |
| 2021 | | 2020 |
| | | |
| (In millions) |
| Cash and cash equivalents | $ | 68 | | | $ | 63 | |
| U.S. Treasury notes | 144 | | | 24 | |
| Magellan Complete Care acquisition opening balance | — | | | 49 | |
| Total restricted investments | $ | 212 | | | $ | 136 | |
7. Property, Equipment, and Capitalized Software, Net
Property and equipment are stated at historical cost. Replacements and major improvements are capitalized, and repairs and maintenance are charged to expense as incurred. Software developed for internal use is capitalized. Furniture and equipment are generally depreciated using the straight-line method over estimated useful lives ranging from three to seven years. Software is generally amortized over its estimated useful life of three years. Leasehold improvements are amortized over the term of the lease, or over their useful lives from five to 10 years, whichever is shorter. Buildings are depreciated over their estimated useful lives of 31.5 to 40 years.
Molina Healthcare, Inc. 2021 Form 10-K | 67
A summary of property, equipment, and capitalized software is as follows:
| | | | | | | | | | | |
| | December 31, |
| | 2021 | | 2020 |
| | | |
| | (In millions) |
| Capitalized software | $ | 547 | | | $ | 475 | |
| Furniture and equipment | 237 | | | 221 | |
| Building and improvements | 37 | | | 49 | |
| Land | 1 | | | 4 | |
| Magellan Complete Care acquisition opening balance | — | | | 3 | |
| Total cost | 822 | | | 752 | |
| Less: accumulated amortization - capitalized software | (427) | | | (385) | |
Less: accumulated depreciation and amortization - furniture, equipment, building, and improvements | (205) | | | (192) | |
| Total accumulated depreciation and amortization | (632) | | | (577) | |
| ROU assets - finance leases | 206 | | | 216 | |
| Property, equipment, and capitalized software, net | $ | 396 | | | $ | 391 | |
The following table presents all depreciation and amortization recognized in our consolidated statements of income:
| | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | |
| (In millions) |
| Recorded in depreciation and amortization: | | | | | |
| Amortization of intangible assets | $ | 49 | | | $ | 15 | | | $ | 18 | |
| Amortization of capitalized software | 41 | | | 38 | | | 33 | |
| Amortization of finance leases | 25 | | | 19 | | | 17 | |
| Depreciation and amortization of furniture, equipment, building, and improvements | 16 | | | 16 | | | 21 | |
| Total depreciation and amortization recognized | $ | 131 | | | $ | 88 | | | $ | 89 | |
8. Leases
We are a party to operating and finance leases primarily for our corporate and health plan offices. Our operating leases have remaining lease terms up to 14 years, some of which include options to extend the leases for up to 10 years. As of December 31, 2021, the weighted average remaining operating lease term is 8 years.
Our finance leases have remaining lease terms up to 17 years, some of which include options to extend the leases for up to 25 years. As of December 31, 2021, the weighted average remaining finance lease term is 14 years.
As of December 31, 2021, the weighted-average discount rate used to compute the present value of lease payments was 4.3% for operating lease liabilities, and 6.4% for finance lease liabilities. The components of lease expense for the years ended December 31, 2021, and 2020, are presented in the following table.
| | | | | | | | | | | | | |
| | | Year Ended December 31, |
| | | 2021 | | 2020 |
| | | | | |
| | | (In millions) |
| Operating lease expense | | | $ | 34 | | | $ | 28 | |
| | | | | |
| Finance lease expense: | | | | | |
| Amortization of ROU assets | | | $ | 25 | | | $ | 19 | |
| Interest on lease liabilities | | | 15 | | | 15 | |
| Total finance lease expense | | | $ | 40 | | | $ | 34 | |
Molina Healthcare, Inc. 2021 Form 10-K | 68
Supplemental consolidated cash flow information related to leases follows:
| | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 |
| | | |
| (In millions) |
| Cash used in operating activities: | | | |
| Operating leases | $ | 33 | | | $ | 30 | |
| Finance leases | 15 | | | 15 | |
| Cash used in financing activities: | | | |
| Finance leases | 18 | | | 9 | |
| ROU assets recognized in exchange for lease obligations: | | | |
| Operating leases | 86 | | | 28 | |
| Finance leases | $ | 18 | | | $ | 7 | |
Supplemental information related to leases, including location of amounts reported in the accompanying consolidated balance sheets, follows:
| | | | | | | | | | | |
| December 31, |
| 2021 | | 2020 |
| | | |
| (In millions) |
| Operating leases: | | | |
| ROU assets | | | |
| Other assets | $ | 128 | | | $ | 58 | |
| Other assets - Magellan Complete Care acquisition opening balance | — | | | 13 | |
| Total other assets | $ | 128 | | | $ | 71 | |
| Lease liabilities | | | |
| Accounts payable and accrued liabilities (current) | $ | 35 | | | $ | 21 | |
| Other long-term liabilities (non-current) | 99 | | | 42 | |
| Magellan Complete Care acquisition opening balance | — | | | 13 | |
| Total operating lease liabilities | $ | 134 | | | $ | 76 | |
| Finance leases: | | | |
| ROU assets | | | |
| Property, equipment, and capitalized software, net | $ | 206 | | | $ | 216 | |
| Lease liabilities | | | |
| Accounts payable and accrued liabilities (current) | $ | 15 | | | $ | 12 | |
| Finance lease liabilities (non-current) | 219 | | | 225 | |
Total finance lease liabilities | $ | 234 | | | $ | 237 | |
Molina Healthcare, Inc. 2021 Form 10-K | 69
Maturities of lease liabilities as of December 31, 2021, were as follows:
| | | | | | | | | | | |
| Operating | | Finance |
| Leases | | Leases |
| | | |
| (In millions) |
| 2022 | $ | 30 | | | $ | 29 | |
| 2023 | 26 | | | 27 | |
| 2024 | 20 | | | 24 | |
| 2025 | 16 | | | 22 | |
| 2026 | 10 | | | 23 | |
| Thereafter | 61 | | | 243 | |
| Subtotal - undiscounted lease payments | 163 | | | 368 | |
| Less imputed interest | (29) | | | (134) | |
| Total | $ | 134 | | | $ | 234 | |
9. Goodwill and Intangible Assets, Net
Goodwill
The following table presents the changes in the carrying amounts of goodwill by segment, for the periods presented.
| | | | | | | | | | | | | | | | | | | | | | | |
| Medicaid | | Medicare | | Other | | Consolidated |
| | | | | | | |
| (In millions) |
Balance, December 31, 2019 | $ | 143 | | | $ | — | | | $ | — | | | $ | 143 | |
| Acquisitions and measurement period adjustments | 346 | | | 161 | | | 42 | | | 549 | |
| Dispositions | — | | | — | | | — | | | — | |
| Impairment | — | | | — | | | — | | | — | |
Balance, December 31, 2020 | 489 | | | 161 | | | 42 | | | 692 | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| Acquisitions and measurement period adjustments | 280 | | | 8 | | | 2 | | | 290 | |
| Dispositions | — | | | — | | | — | | | — | |
| Impairment | — | | | — | | | — | | | — | |
Balance, December 31, 2021 | 769 | | | 169 | | | 44 | | | 982 | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
The changes in the carrying amounts of both goodwill and intangible assets, net, in 2021, were due to the purchase price adjustments and acquisitions described in Note 4, “Business Combinations.”
Intangible Assets, Net
The following table provides the details of identified intangible assets, by major class, for the periods presented.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| December 31, 2021 | | December 31, 2020 |
| Cost | | Accumulated
Amortization | | Carrying Amount | | Cost | | Accumulated
Amortization | | Carrying Amount |
| | | | | | | | | | | |
| | (In millions) |
| Contract rights and licenses | $ | 426 | | | $ | 210 | | | $ | 216 | | | $ | 370 | | | $ | 168 | | | $ | 202 | |
| Provider networks | 56 | | | 19 | | | 37 | | | 47 | | | 15 | | | 32 | |
| Trade name | 19 | | | 2 | | | 17 | | | 15 | | | — | | | 15 | |
| Total | $ | 501 | | | $ | 231 | | | $ | 270 | | | $ | 432 | | | $ | 183 | | | $ | 249 | |
As of December 31, 2021, we estimate that our intangible asset amortization will be approximately $59 million in 2022, $57 million in 2023, $56 million in 2024, $55 million in 2025, and $15 million in 2026.
Molina Healthcare, Inc. 2021 Form 10-K | 70
10. Medical Claims and Benefits Payable
The following table provides the details of our medical claims and benefits payable as of the dates indicated.
| | | | | | | | | | | | | | | | | |
| December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | |
| (In millions) |
| Fee-for-service claims incurred but not paid (“IBNP”) | $ | 2,486 | | | $ | 1,647 | | | $ | 1,406 | |
| Pharmacy payable | 219 | | | 157 | | | 126 | |
| Capitation payable | 82 | | | 70 | | | 55 | |
| Other | 576 | | | 528 | | | 267 | |
| Magellan Complete Care acquisition opening balance | — | | | 294 | | | — | |
| Total | $ | 3,363 | | | $ | 2,696 | | | $ | 1,854 | |
“Other” medical claims and benefits payable include amounts payable to certain providers for which we act as an intermediary on behalf of various government agencies without assuming financial risk. Such receipts and payments do not impact our consolidated statements of income. Non-risk provider payables amounted to $226 million, $235 million and $132 million, as of December 31, 2021, 2020, and 2019, respectively.
The following tables present the components of the change in our medical claims and benefits payable for the periods indicated, with the prior periods recast to conform to current year presentation.
| | | | | | | | | | | | | | | | | | | | | | | |
| Year Ended December 31, 2021 |
| Medicaid | | Medicare | | Marketplace | | Consolidated |
| | | | | | | |
| | (In millions) |
| Medical claims and benefits payable, beginning balance | $ | 2,129 | | | $ | 392 | | | $ | 175 | | | $ | 2,696 | |
| Components of medical care costs related to: | | | | | | | |
| Current year | 18,321 | | | 2,970 | | | 2,652 | | | 23,943 | |
| Prior years | (182) | | | (39) | | | (18) | | | (239) | |
| Total medical care costs | 18,139 | | | 2,931 | | | 2,634 | | | 23,704 | |
| Payments for medical care costs related to: | | | | | | | |
| Current year | 16,284 | | | 2,573 | | | 2,291 | | | 21,148 | |
| Prior years | 1,601 | | | 340 | | | 139 | | | 2,080 | |
| Total paid | 17,885 | | | 2,913 | | | 2,430 | | | 23,228 | |
| Acquired balances, net of post-acquisition adjustments | 205 | | | (8) | | | — | | | 197 | |
| Change in non-risk and other provider payables | (8) | | | 2 | | | — | | | (6) | |
| Medical claims and benefits payable, ending balance | $ | 2,580 | | | $ | 404 | | | $ | 379 | | | $ | 3,363 | |
| | | | | | | |
Molina Healthcare, Inc. 2021 Form 10-K | 71
| | | | | | | | | | | | | | | | | | | | | | | |
| Year Ended December 31, 2020 |
| Medicaid | | Medicare | | Marketplace | | Consolidated |
| | | | | | | |
| | (In millions) |
| Medical claims and benefits payable, beginning balance | $ | 1,465 | | | $ | 267 | | | $ | 122 | | | $ | 1,854 | |
| Components of medical care costs related to: | | | | | | | |
| Current year | 12,545 | | | 2,189 | | | 1,205 | | | 15,939 | |
| Prior years | (84) | | | (28) | | | (7) | | | (119) | |
| Total medical care costs | 12,461 | | | 2,161 | | | 1,198 | | | 15,820 | |
| Payments for medical care costs related to: | | | | | | | |
| Current year | 10,940 | | | 1,884 | | | 1,047 | | | 13,871 | |
| Prior years | 1,176 | | | 233 | | | 98 | | | 1,507 | |
| Total paid | 12,116 | | | 2,117 | | | 1,145 | | | 15,378 | |
| Acquired balances, net of post-acquisition adjustments | 215 | | | 79 | | | — | | | 294 | |
| Change in non-risk and other provider payables | 104 | | | 2 | | | — | | | 106 | |
| Medical claims and benefits payable, ending balance | $ | 2,129 | | | $ | 392 | | | $ | 175 | | | $ | 2,696 | |
| | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
| Year Ended December 31, 2019 |
| Medicaid | | Medicare | | Marketplace | | Consolidated |
| | | | | | | |
| | (In millions) |
| Medical claims and benefits payable, beginning balance | $ | 1,554 | | | $ | 253 | | | $ | 154 | | | $ | 1,961 | |
| Components of medical care costs related to: | | | | | | | |
| Current year | 11,191 | | | 1,934 | | | 1,051 | | | 14,176 | |
| Prior years | (222) | | | (21) | | | (28) | | | (271) | |
| Total medical care costs | 10,969 | | | 1,913 | | | 1,023 | | | 13,905 | |
| Payments for medical care costs related to: | | | | | | | |
| Current year | 9,936 | | | 1,676 | | | 942 | | | 12,554 | |
| Prior years | 1,145 | | | 224 | | | 113 | | | 1,482 | |
| Total paid | 11,081 | | | 1,900 | | | 1,055 | | | 14,036 | |
| Acquired balances, net of post-acquisition adjustments | — | | | — | | | — | | | — | |
| Change in non-risk and other provider payables | 23 | | | 1 | | | — | | | 24 | |
| Medical claims and benefits payable, ending balance | $ | 1,465 | | | $ | 267 | | | $ | 122 | | | $ | 1,854 | |
| | | | | | | |
The amounts presented for “Components of medical care costs related to: Prior years” represent the amount by which our original estimate of medical claims and benefits payable at the beginning of the year varied from the actual liabilities, based on information (principally the payment of claims) developed since those liabilities were first reported.
Our estimates of medical claims and benefits payable recorded at December 31, 2021, 2020 and 2019 developed favorably by approximately $239 million, $119 million and $271 million in 2021, 2020 and 2019, respectively. The favorable prior year development recognized in 2021 was primarily due to lower than expected utilization of medical services by our Medicaid members, and to a lesser extent our Medicare and Marketplace members, and improved operating performance. Consequently, the ultimate costs recognized in 2021 were lower than our original estimates in 2020, which was not discernible until additional information was provided, and as claims payments were processed.
The favorable prior year development recognized in 2020 was primarily due to lower than expected utilization of medical services by our Medicaid members, and improved operating performance. Consequently, the ultimate costs recognized in 2020 were lower than our original estimates in 2019, which was not discernible until additional information was provided, and as claims payments were processed.
The favorable prior year development recognized in 2019 was primarily due to lower than expected utilization of medical services by our Medicaid members, and improved operating performance. Consequently, the ultimate costs recognized in 2019 were lower than our original estimates in 2018, which was not discernible until additional information was provided, and as claims payments were processed.
Molina Healthcare, Inc. 2021 Form 10-K | 72
The following tables provide information about our consolidated incurred and paid claims development as of December 31, 2021, as well as cumulative claims frequency and the total of incurred but not paid claims liabilities. The pattern of incurred and paid claims development is consistent across each of our segments. The cumulative claim frequency is measured by claim event, and includes claims covered under capitated arrangements.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Incurred Claims and Allocated Claims Adjustment Expenses | | Total IBNP | | Cumulative number of reported claims |
| Benefit Year | | 2019 | | 2020 | | 2021 | |
| | | | | | | | | | |
| | (Unaudited) | | (Unaudited) | | | | | | |
| | (In millions) |
| 2019 | | $ | 14,176 | | | $ | 14,083 | | | $ | 14,040 | | | $ | 12 | | | 105 | |
| 2020 | | | | 16,233 | | | 16,056 | | | 52 | | | 140 | |
| 2021 | | | | | | 23,943 | | | 2,416 | | | 181 | |
| | | | | | $ | 54,039 | | | $ | 2,480 | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
| Cumulative Paid Claims and Allocated Claims Adjustment Expenses | |
| Benefit Year | | 2019 | | 2020 | | 2021 | |
| | | | | | | |
| | (Unaudited) | | (Unaudited) | | | |
| | (In millions) | |
| 2019 | | $ | 12,554 | | | $ | 14,056 | | | $ | 14,028 | | |
| 2020 | | | | 13,871 | | | 16,004 | | |
| 2021 | | | | | | 21,148 | | |
| | | | | | $ | 51,180 | | |
The following table represents a reconciliation of claims development to the aggregate carrying amount of the liability for medical claims and benefits payable.
| | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | 2021 | |
| | | | | | | |
| | | | | | (In millions) | |
| Incurred claims and allocated claims adjustment expenses | | $ | 54,039 | | |
| Less: cumulative paid claims and allocated claims adjustment expenses | | (51,180) | | |
| All outstanding liabilities before 2019 | | 6 | | |
| Acquired balances | | 224 | | |
| Non-risk and other provider payables | | 274 | | |
| Medical claims and benefits payable | | $ | 3,363 | | |
11. Debt
Contractual maturities of debt, as of December 31, 2021, are illustrated in the following table. All amounts represent the principal amounts of the debt instruments outstanding.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Total | | 2022 | | 2023 | | 2024 | | 2025 | | 2026 | | Thereafter |
| | | | | | | | | | | | | |
| (In millions) |
4.375% Notes due 2028 | $ | 800 | | | $ | — | | | $ | — | | | $ | — | | | $ | — | | | $ | — | | | $ | 800 | |
3.875% Notes due 2030 | 650 | | | — | | | — | | | — | | | — | | | — | | | 650 | |
3.875% Notes due 2032 | 750 | | | — | | | — | | | — | | | — | | | — | | | 750 | |
| Total | $ | 2,200 | | | $ | — | | | $ | — | | | $ | — | | | $ | — | | | $ | — | | | $ | 2,200 | |
Molina Healthcare, Inc. 2021 Form 10-K | 73
All our debt is held at the parent which is reported in the Other segment. The following table summarizes our outstanding debt obligations, all of which are non-current as of the dates reported below:
| | | | | | | | | | | |
| December 31, |
| 2021 | | 2020 |
| | | |
| (In millions) |
| | | |
| | | |
| | | |
| | | |
| Non-current portion of long-term debt: | | | |
5.375% Notes due 2022 | $ | — | | | $ | 700 | |
4.375% Notes due 2028 | 800 | | | 800 | |
3.875% Notes due 2030 | 650 | | | 650 | |
3.875% Notes due 2032 | 750 | | | — | |
| Less: debt issuance costs | (27) | | | (23) | |
| Total | $ | 2,173 | | | $ | 2,127 | |
Credit Agreement
We are party to a credit agreement (the “Credit Agreement”) which includes a revolving credit facility (“Credit Facility”) of $1.0 billion, among other provisions. The Credit Agreement has a term of five years, and all amounts outstanding will be due and payable on June 8, 2025. Borrowings under the Credit Agreement bear interest based, at our election, on a base rate or other defined rate, plus in each case, the applicable margin. In addition to interest payable on the principal amount of indebtedness outstanding from time to time under the Credit Agreement, we are required to pay a quarterly commitment fee.
The Credit Agreement contains customary non-financial and financial covenants. As of December 31, 2021, we were in compliance with all financial and non-financial covenants under the Credit Agreement and other long-term debt. As of December 31, 2021, no amounts were outstanding under the Credit Facility.
Senior Notes
Our senior notes are described below. Each of these notes are senior unsecured obligations of Molina and rank equally in right of payment with all existing and future senior debt, and senior to all existing and future subordinated debt of Molina. In addition, each of the notes contain customary non-financial covenants and change of control provisions.
The indentures governing the senior notes contain cross-default provisions that are triggered upon default by us or any of our subsidiaries on any indebtedness in excess of the amount specified in the applicable indenture.
5.375% Notes due 2022. In December 2021, we completed the early redemption of the entire $700 million aggregate principal amount of senior notes (the “5.375% Notes”) that would have been due November 15, 2022. In accordance with the indenture governing such notes, the 5.375% Notes were settled at 100% of par, plus an early redemption premium which amounted to $23 million, plus accrued and unpaid interest. In conjunction with the redemption we wrote off $2 million in unamortized deferred issuance costs directly related to the 5.375% Notes.
4.375% Notes due 2028. We have $800 million aggregate principal amount of senior notes (the “4.375% Notes”) outstanding as of December 31, 2021, which are due June 15, 2028, unless earlier redeemed. Interest, at a rate of 4.375% per annum, is payable semiannually in arrears on June 15 and December 15.
3.875% Notes due 2030. We have $650 million aggregate principal amount of senior notes (the “3.875% Notes due 2030”) outstanding as of December 31, 2021, which are due November 15, 2030, unless earlier redeemed. Interest, at a rate of 3.875% per annum, is payable semiannually in arrears on May 15 and November 15.
3.875% Notes due 2032. On November 16, 2021, we completed the private offering of $750 million aggregate principal amount of senior notes (the “3.875% Notes due 2032”) due May 15, 2032, unless earlier redeemed. The 3.875% Notes due 2032 contain optional early redemption provisions, with redemption prices in excess of par. Interest, at a rate of 3.875% per annum, is payable semiannually in arrears on May 15 and November 15 of each year, commencing on May 15, 2022. A large majority of the net proceeds from the 3.875% Notes due 2032 offering was used to repay $700 million principal amount outstanding under the 5.375% Notes, and the balance is intended to be used for general corporate purposes. Deferred issuance costs amounted to $10 million.
In 2021, we recognized an aggregate loss on debt repayment of $25 million including costs incurred in the early redemption of the 5.375% Notes described above. In 2020, we recognized an aggregate loss on debt repayment of $15 million including costs incurred in repayment of the term loan facility, the early redemption of the entire
Molina Healthcare, Inc. 2021 Form 10-K | 74
$330 million aggregate principal amount of our senior notes that would have been due in June 2025, and other financing transactions. These costs are located within other expenses (income), net within our consolidated statements of income.
12. Income Taxes
Income tax expense for continuing operations consisted of the following:
| | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | |
| (In millions) |
| Current: | | | | | |
| Federal | $ | 209 | | | $ | 281 | | | $ | 204 | |
| State | 31 | | | 26 | | | 12 | |
| Foreign | — | | | — | | | 9 | |
| Total current | 240 | | | 307 | | | 225 | |
| Deferred: | | | | | |
| Federal | (17) | | | (13) | | | 5 | |
| State | (7) | | | (7) | | | 6 | |
| Foreign | — | | | 1 | | | (1) | |
| Total deferred | (24) | | | (19) | | | 10 | |
| Income tax expense | $ | 216 | | | $ | 288 | | | $ | 235 | |
A reconciliation of the U.S. federal statutory income tax rate to the combined effective income tax rate for continuing operations is as follows:
| | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| Statutory federal tax (benefit) rate | 21.0 | % | | 21.0 | % | | 21.0 | % |
| State income provision (benefit), net of federal benefit | 2.2 | | | 1.6 | | | 1.4 | |
| | | | | |
| Nondeductible health insurer fee (“HIF”) | — | | | 6.1 | | | — | |
| Nondeductible compensation | 1.5 | | | 1.1 | | | 1.2 | |
| | | | | |
| Other | — | | | 0.2 | | | 0.6 | |
| Effective tax expense rate | 24.7 | % | | 30.0 | % | | 24.2 | % |
The effective tax rate was not impacted by the HIF in 2019 given the HIF moratorium. HIF was repealed for years after 2020. Our effective tax rate is based on expected income, statutory tax rates, and tax planning opportunities available to us in the various jurisdictions in which we operate. Management estimates and judgments are required in determining our effective tax rate. We are routinely under audit by federal, state, or local authorities regarding the timing and amount of deductions, nexus of income among various tax jurisdictions, and compliance with federal, state, foreign, and local tax laws.
Molina Healthcare, Inc. 2021 Form 10-K | 75
Deferred tax assets and liabilities are classified as non-current. Significant components of our deferred tax assets and liabilities as of December 31, 2021 and 2020 were as follows:
| | | | | | | | | | | |
| December 31, |
| 2021 | | 2020 |
| | | |
| (In millions) |
| Accrued expenses and reserve liabilities | $ | 57 | | | $ | 52 | |
| Other accrued medical costs | 23 | | | 15 | |
| Net operating losses | 13 | | | 11 | |
| | | |
| Unearned premiums | 17 | | | 18 | |
| Lease financing obligation | 9 | | | 8 | |
| Tax credit carryover | 5 | | | 7 | |
| Other | 6 | | | 4 | |
| Valuation allowance | (10) | | | (17) | |
| Total deferred income tax assets, net of valuation allowance | 120 | | | 98 | |
| Fixed assets and intangibles | (1) | | | (7) | |
| Prepaid expenses | (13) | | | (10) | |
| Unrealized gains and losses | — | | | (12) | |
| | | |
| Total deferred income tax liabilities | (14) | | | (29) | |
| Net deferred income tax asset | $ | 106 | | | $ | 69 | |
At December 31, 2021, we had state net operating loss carryforwards of $177 million, which begin expiring in 2036.
At December 31, 2021, we had foreign net operating loss carryforwards of $9 million, which expire in 2032.
At December 31, 2021, we had foreign tax credit carryovers of $5 million, which expire in 2030.
We evaluate the need for a valuation allowance taking into consideration the ability to carry back and carry forward tax credits and losses, available tax planning strategies and future income, including reversal of temporary differences. We have determined that as of December 31, 2021, $10 million of deferred tax assets did not satisfy the recognition criteria. Therefore, we decreased our valuation allowance by $7 million, from $17 million at December 31, 2020, to $10 million as of December 31, 2021.
We recognize tax benefits only if the tax position is more likely than not to be sustained. We are subject to income taxes in the United States, Puerto Rico, and numerous state jurisdictions. Significant judgment is required in evaluating our tax positions and determining our provision for income taxes. During the ordinary course of business, there are many transactions and calculations for which the ultimate tax determination is uncertain. We establish reserves for tax-related uncertainties based on estimates of whether, and the extent to which, additional taxes will be due. These reserves are established when we believe that certain positions might be challenged despite our belief that our tax return positions are fully supportable. We adjust these reserves in light of changing facts and circumstances, such as the outcome of tax audits. The provision for income taxes includes the impact of reserve provisions and changes to reserves that are considered appropriate.
The roll forward of our unrecognized tax benefits is as follows:
| | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | |
| (In millions) |
| Gross unrecognized tax benefits at beginning of period | $ | (20) | | | $ | (20) | | | $ | (20) | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| Settlements | 5 | | | — | | | — | |
| | | | | |
| Gross unrecognized tax benefits at end of period | $ | (15) | | | $ | (20) | | | $ | (20) | |
The total amount of unrecognized tax benefits at December 31, 2021, 2020 and 2019 that, if recognized, would affect the effective tax rates is $15 million, $20 million, and $20 million, respectively. We expect that during the next 12 months it is reasonably possible that unrecognized tax benefit liabilities may decrease by as much as $10 million as a result of the expiration of statutes of limitations.
Molina Healthcare, Inc. 2021 Form 10-K | 76
Our continuing practice is to recognize interest and/or penalties related to unrecognized tax benefits in income tax expense. Amounts accrued for the payment of interest and penalties as of December 31, 2021, 2020 and 2019 were insignificant.
The U.S. Internal Revenue Service (IRS) completed exams for years 2017 and prior. We may be subject to examination by the IRS for calendar years after 2017. With a few exceptions, which are immaterial in the aggregate, we no longer are subject to state, local, and Puerto Rico tax examinations for years before 2017.
13. Stockholders' Equity
Stock Purchase Programs
In September 2021, our board of directors authorized the purchase of up to $500 million, in the aggregate, of our common stock. This new program immediately supersedes the stock purchase program previously approved by our board of directors in September 2020, as described below. This new program will be funded with cash on hand and extends through December 31, 2022. The exact timing and amount of any repurchase is determined by management based on market conditions and share price, in addition to other factors, and subject to the restrictions relating to volume, price, and timing under applicable law. As of February 14, 2022, no shares had been purchased under this stock purchase program.
In September 2020, our board of directors authorized the purchase of up to $500 million, in the aggregate, of our common stock. This program was funded with cash on hand. Under this program, pursuant to a Rule 10b5-1 trading plan, we purchased approximately 577,000 shares of our common stock for $122 million in January and February 2021 (average cost of $211.65). In November and December 2020, we purchased 766,000 shares of our common stock for $159 million (average cost of $208.37), including approximately 29,000 shares purchased for $6 million in late December 2020, and settled in early January 2021.
Share-Based Compensation
In connection with our employee stock plans, approximately 429,000 shares and 244,000 shares of common stock were issued, net of shares used to settle employees’ income tax obligations, during the years ended December 31, 2021, and 2020, respectively. Total share-based compensation expense is reported in “General and administrative expenses” in the accompanying consolidated statements of income, and summarized below.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | | | | | | | |
| (In millions) |
| Pretax
Charges | | Net-of-Tax
Amount | | Pretax
Charges | | Net-of-Tax
Amount | | Pretax
Charges | | Net-of-Tax
Amount |
| RSAs, PSAs and PSUs (defined below) | $ | 66 | | | $ | 62 | | | $ | 47 | | | $ | 44 | | | $ | 29 | | | $ | 28 | |
Employee stock purchase plan and stock options | 6 | | | 6 | | | 10 | | | 9 | | | 10 | | | 9 | |
| Total | $ | 72 | | | $ | 68 | | | $ | 57 | | | $ | 53 | | | $ | 39 | | | $ | 37 | |
Equity Incentive Plan
At December 31, 2021, we had employee equity incentives outstanding under our 2019 Equity Incentive Plan (the “2019 EIP”). The 2019 EIP provides for awards, in the form of restricted and performance stock awards (“RSAs” and “PSAs”), performance units (“PSUs”), stock options, and other stock– or cash–based awards, to eligible persons who perform services for us. The 2019 EIP provides for the issuance of up to 2.9 million shares of our common stock.
Stock-based awards. RSAs, PSAs and PSUs are granted with a fair value equal to the market price of our common stock on the date of grant, and generally vest in equal annual installments over periods up to four years from the date of grant. Certain PSUs may vest in their entirety at the end of three-year performance periods, if their performance conditions are met. We generally recognize expense for RSAs, PSAs and PSUs on a straight-line basis. Activity for stock-based awards in the year ended December 31, 2021, is summarized below.
Molina Healthcare, Inc. 2021 Form 10-K | 77
| | | | | | | | | | | | | | | | | | | | | | | |
| RSAs | | Weighted
Average
Grant Date
Fair Value | | PSUs | | Weighted
Average
Grant Date
Fair Value |
Unvested balance, December 31, 2020 | 585,084 | | | $ | 118.07 | | | 471,909 | | | $ | 111.04 | |
| Granted | 289,227 | | | 224.63 | | | 160,670 | | | 74.52 | |
| Vested | (232,896) | | | 112.62 | | | (321,340) | | | 74.52 | |
| Forfeited | (102,298) | | | 161.36 | | | (36,189) | | | 129.19 | |
Unvested balance, December 31, 2021 | 539,117 | | | $ | 169.39 | | | 275,050 | | | $ | 129.99 | |
| | | | | | | |
As of December 31, 2021, total unrecognized compensation expense related to unvested RSAs and PSUs was $55 million, and $12 million, respectively, which we expect to recognize over a remaining weighted-average period of 2.1 years, and 0.8 years, respectively. This unrecognized compensation cost assumes an estimated forfeiture rate of 11.3% for non-executive employees as of December 31, 2021, based on actual forfeitures over the last 4 years.
During the year ended December 31, 2021, we granted 127,102 PSUs which vest in a range from 0% to 200% of the number of target units awarded, depending on the Company’s level of achievement with respect to the financial performance goal, after three years. We have not recognized stock compensation expense for these PSUs during the year ended December 31, 2021 as the complete performance conditions have not been determined as of December 31, 2021. We expect the performance conditions to be determined during the third year of vesting. At December 31, 2021, 116,172 PSUs were outstanding.
The total grant date fair value of awards granted and vested is presented in the following table.
| | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | |
| (In millions) |
| Granted: | | | | | |
| RSAs | $ | 65 | | | $ | 44 | | | $ | 33 | |
| PSUs | — | | | 23 | | | 20 | |
| Total granted | $ | 65 | | | $ | 67 | | | $ | 53 | |
| Vested: | | | | | |
| RSAs | $ | 53 | | | $ | 22 | | | $ | 19 | |
| PSUs | 71 | | | 1 | | | 2 | |
| Total vested | $ | 124 | | | $ | 23 | | | $ | 21 | |
Stock Options. Stock option awards generally have an exercise price equal to the fair market value of our common stock on the date of grant, vest in equal annual installments over periods up to four years from the date of grant, and have a maximum term of ten years from the date of grant. Stock option activity for the year ended December 31, 2021, is summarized below.
| | | | | | | | | | | | | | | | | | | | | | | |
| Number of Shares | | Weighted Average Exercise Price | | Aggregate Intrinsic Value | | Weighted Average Remaining Contractual term |
| | | | | | | |
| | | (Per share) | | (In millions) | | (Years) |
Stock options outstanding as of December 31, 2020 | 405,000 | | | $ | 64.79 | | | | | |
| Exercised | (10,000) | | | 33.02 | | | | | |
Stock options outstanding, vested, and exercisable as of December 31, 2021 | 395,000 | | | 65.59 | | | $ | 100 | | | 5.5 |
| | | | | | | |
| | | | | | | |
No stock options were granted in 2021, 2020, or 2019, and no stock options were exercised in 2020, or 2019. As of December 31, 2021, there was no unrecognized compensation expense related to unvested stock options.
Employee Stock Purchase Plans (“ESPP”)
Under our ESPP, eligible employees may purchase common shares at 85% of the lower of the fair market value of our common stock on either the first or last trading day of each six-month offering period. Each participant is limited to a maximum purchase of $25,000 (as measured by the fair value of the stock acquired) per year through payroll
Molina Healthcare, Inc. 2021 Form 10-K | 78
deductions. We estimate the fair value of the stock issued using a standard option pricing model. For the years ended December 31, 2021, 2020, and 2019, the inputs to this model were as follows: risk-free interest rates of approximately 0.1% to 2.3%; expected volatility of approximately 35% to 54%, dividend yields of 0%, and an average expected life of 0.5 years.
14. Employee Benefit Plans
We sponsor defined contribution 401(k) plans that cover substantially all employees of our company and its subsidiaries. Eligible employees are permitted to contribute up to the maximum amount allowed by law. We match up to the first 4% of compensation contributed by employees. Expense recognized in connection with our contributions to the 401(k) plans amounted to $41 million, $28 million, and $28 million in the years ended December 31, 2021, 2020, and 2019, respectively.
We also have a non-qualified deferred compensation plan for certain key employees. Under this plan, eligible participants may defer portions of their base salary and bonus to provide tax-deferred growth. The deferrals are distributable based upon termination of employment or other periods, as elected under the plan and were $23 million and $17 million as of December 31, 2021 and 2020, respectively.
15. Commitments and Contingencies
Regulatory Capital Requirements and Dividend Restrictions
Our health plans, which are generally operated by our respective wholly owned subsidiaries in those states in which our health plans operate, are subject to state laws and regulations that, among other things, require the maintenance of minimum levels of statutory capital, as defined by each state. The National Association of Insurance Commissioners (“NAIC”), has adopted rules which, if implemented by the states, set minimum capitalization requirements for insurance companies, HMOs, and other entities bearing risk for healthcare coverage. The requirements take the form of risk-based capital (“RBC”) rules which may vary from state to state. Regulators in some states may also enforce capital requirements that require the retention of net worth in excess of amounts formally required by statute or regulation.
All of the states in which our health plans operate, except California, Florida, Massachusetts and New York, have adopted the RBC rules. The RBC rules, if adopted by California, Florida, Massachusetts or New York, could increase the minimum capital required for those states. Our Massachusetts health plan maintains a $35 million performance bond, effective through December 31, 2022, to partially satisfy minimum net worth requirements in that state.
Statutes, regulations and informal capital requirements also restrict the timing, payment, and amount of dividends and other distributions that may be paid to us as the sole stockholder. To the extent our subsidiaries must comply with these regulations, they may not have the financial flexibility to transfer funds to us. Based on current statutes and regulations, the net assets in these subsidiaries, which may not be transferable to us in the form of loans, advances, or cash dividends was approximately $2.7 billion at December 31, 2021. Because of the statutory restrictions that inhibit the ability of our health plans to transfer net assets to us, the amount of retained earnings readily available to pay dividends to our stockholders is generally limited to cash, cash equivalents and investments held by the parent company—Molina Healthcare, Inc. Such cash, cash equivalents and investments amounted to $348 million and $644 million as of December 31, 2021 and 2020, respectively.
As of December 31, 2021, our health plans had aggregate statutory capital and surplus of approximately $2.9 billion, which was in excess of the required minimum aggregate statutory capital and surplus of approximately $2.1 billion. We have the ability and commitment to provide additional capital to each of our health plans when necessary to ensure that statutory capital and surplus continue to meet regulatory requirements.
COVID-19 Pandemic
We continue to monitor and assess the estimated operating and financial impact of the COVID-19 pandemic, and as it evolves, we continue to process, assemble, and assess member utilization information. We believe that our cash resources, borrowing capacity available under the Credit Agreement, and cash flow generated from operations will be sufficient to withstand the financial impact of the pandemic, and will enable us to continue to support our
Molina Healthcare, Inc. 2021 Form 10-K | 79
operations, regulatory requirements, debt repayment obligations, and capital expenditures for the foreseeable future.
Legal Proceedings
The healthcare industry is subject to numerous laws and regulations of federal, state, and local governments. Compliance with these laws and regulations can be subject to government review and interpretation, as well as regulatory actions unknown and unasserted at this time. Penalties associated with violations of these laws and regulations include significant fines and penalties, exclusion from participating in publicly funded programs, and the repayment of previously billed and collected revenues.
We are involved in legal actions in the ordinary course of business including, but not limited to, various employment claims, vendor disputes and provider claims. Some of these legal actions seek monetary damages, including claims for punitive damages, which may not be covered by insurance. We review legal matters and update our estimates of reasonably possible losses and related disclosures, as necessary. We have accrued liabilities for legal matters for which we deem the loss to be both probable and reasonably estimable. These liability estimates could change as a result of further developments of the matters. The outcome of legal actions is inherently uncertain. An adverse determination in one or more of these pending matters could have an adverse effect on our consolidated financial position, results of operations, or cash flows.
Kentucky RFP. On September 4, 2020, Anthem Kentucky Managed Care Plan, Inc. brought an action in Franklin County Circuit Court against the Kentucky Finance and Administration Cabinet, the Kentucky Cabinet for Health and Family Services, and all of the five winning bidder health plans, including our Kentucky health plan. This matter remains subject to additional legal and appellate proceedings, and no assurances can be given regarding the ultimate outcome. Under the Court’s June 16, 2021 final Order, our Kentucky health plan will continue to operate for the foreseeable future under its current Medicaid contract and provide care to Kentucky Medicaid members.
Puerto Rico. On August 13, 2021, Molina Healthcare of Puerto, Inc. (“MHPR”) filed a complaint asserting, among other claims, breach of contract against Puerto Rico Health Insurance Administration (“ASES”). On September 13, 2021, in addition to filing its answer to MHPR’s complaint, ASES filed a counterclaim and a third-party complaint against MHPR and the Company. The counterclaim alleges that MHPR and the Company breached contractual obligations by failing to pay providers and, in addition to damages, seeks various equitable remedies. On October 8, 2021, MHPR filed its reply to the counterclaim, denying all the allegations, and on November 1, 2021, the Company filed its answer to the third-party complaint. On December 3, 2021, MHPR filed a request for disbursement of illegally withheld funds, and ASES filed its opposition. At a status hearing on January 19, 2022, the Company and ASES both argued MHPR’s request for disbursement. The court has not ruled. This matter is in its early stages, and no prediction can be made as to the outcome. No gain or loss is probable and reasonably estimable with regard to either MHPR’s complaint or the counterclaim of ASES.
Professional Liability Insurance
We carry medical professional liability insurance for healthcare services rendered in the primary care institutions that we manage. In addition, we carry managed care errors and omissions insurance for all managed care services that we provide.
16. Segments
In the first quarter of 2021, we realigned our reportable operating segments to reflect recent changes in our internal operating and reporting structure, which is now organized by government program. The revised reporting structure reflects the reporting and review process used by our chief executive officer (who is our chief operating decision maker) to assess performance and allocate resources, and is consistent with how we currently manage the business and view the markets we serve. These reportable segments consist of: 1) Medicaid; 2) Medicare; 3) Marketplace; and 4) Other.
The Medicaid, Medicare, and Marketplace segments represent the government-funded or sponsored programs under which we offer managed healthcare services. The Other segment, which is insignificant to our consolidated results of operations, includes certain corporate amounts not associated with or allocated to the Medicaid, Medicare, or Marketplace segments. Additionally, the Other segment includes service revenues and service costs associated with the long-term services and supports consultative services we now provide in Wisconsin, as a result of the Magellan Complete Care acquisition on December 31, 2020.
Molina Healthcare, Inc. 2021 Form 10-K | 80
The key metrics used to assess the performance of our Medicaid, Medicare, and Marketplace segments are premium revenue, medical margin and MCR. MCR represents the amount of medical care costs as a percentage of premium revenue. Therefore, the underlying medical margin, or the amount earned by the Medicaid, Medicare, and Marketplace segments after medical costs are deducted from premium revenue, represents the most important measure of earnings reviewed by management, and is used by our chief executive officer to review results, assess performance, and allocate resources. The key metric used to assess the performance of our Other segment is service margin. The service margin is equal to service revenue minus cost of service revenue. We do not report total assets by segment since this is not a metric used to assess segment performance or allocate resources.
For all tables presented below, the prior period disclosures have been recast to conform to the current period segment presentation.
The following table presents total revenue by segment. Inter-segment revenue was insignificant for all periods presented.
| | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | |
| (In millions) |
| Total revenue: | | | | | |
| Medicaid | $ | 21,231 | | | $ | 15,217 | | | $ | 13,026 | |
| Medicare | 3,379 | | | 2,529 | | | 2,265 | |
| Marketplace | 3,091 | | | 1,677 | | | 1,538 | |
| Other | 70 | | | — | | | — | |
| Consolidated | $ | 27,771 | | | $ | 19,423 | | | $ | 16,829 | |
The following table reconciles margin by segment to consolidated income before income tax expense:
| | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | |
| (In millions) |
| Margin: | | | | | |
| Medicaid | $ | 2,322 | | | $ | 1,804 | | | $ | 1,496 | |
| Medicare | 430 | | | 351 | | | 331 | |
| Marketplace | 399 | | | 324 | | | 476 | |
| Other | 14 | | | — | | | — | |
| Total margin | 3,165 | | | 2,479 | | | 2,303 | |
Add: other operating revenues (1) | 846 | | | 1,124 | | | 621 | |
Less: other operating expenses (2) | (2,991) | | | (2,525) | | | (1,880) | |
| Operating income | 1,020 | | | 1,078 | | | 1,044 | |
| Less: other expenses, net | 145 | | | 117 | | | 72 | |
| Income before income tax expense | $ | 875 | | | $ | 961 | | | $ | 972 | |
______________________
(1)Other operating revenues include premium tax revenue, health insurer fees reimbursed, Marketplace risk corridor judgment, investment income and other revenue.
(2)Other operating expenses include general and administrative expenses, premium tax expenses, health insurer fees, depreciation and amortization, and other costs.
Molina Healthcare, Inc. 2021 Form 10-K | 81
17. Condensed Financial Information of Registrant
The condensed balance sheets as of December 31, 2021 and 2020, and the related condensed statements of income, comprehensive income and cash flows for each of the three years in the period ended December 31, 2021 for our parent company Molina Healthcare, Inc. (the “Registrant”), are presented below.
Condensed Balance Sheets
| | | | | | | | | | | |
| | December 31, |
| | 2021 | | 2020 |
| | | |
| | (In millions, except per-share data) |
| ASSETS |
| Current assets: | | | |
| Cash and cash equivalents | $ | 274 | | | $ | 575 | |
| Investments | 74 | | | 69 | |
| Receivables | — | | | 2 | |
| Due from affiliates | 74 | | | 114 | |
| Prepaid expenses and other current assets | 142 | | | 65 | |
| Total current assets | 564 | | | 825 | |
| Property, equipment, and capitalized software, net | 349 | | | 339 | |
| Goodwill and intangible assets, net | 699 | | | 369 | |
| Investments in subsidiaries | 3,772 | | | 3,228 | |
| Deferred income taxes | (18) | | | 5 | |
| Advances to related parties and other assets | 68 | | | 83 | |
| Total assets | $ | 5,434 | | | $ | 4,849 | |
| LIABILITIES AND STOCKHOLDERS’ EQUITY |
| Current liabilities: | | | |
| Accounts payable, accrued liabilities and other | $ | 378 | | | $ | 338 | |
| Total current liabilities | 378 | | | 338 | |
| Long-term debt | 2,173 | | | 2,127 | |
| Finance lease liabilities | 219 | | | 225 | |
| Other long-term liabilities | 34 | | | 63 | |
| Total liabilities | 2,804 | | | 2,753 | |
| Stockholders’ equity: | | | |
Common stock, $0.001 par value; 150 million shares authorized; outstanding: 58 million shares at December 31, 2021, and 59 million at December 31, 2020 | — | | | — | |
Preferred stock, $0.001 par value; 20 million shares authorized, no shares issued and outstanding | — | | | — | |
| Additional paid-in capital | 236 | | | 199 | |
| Accumulated other comprehensive (loss) income | (5) | | | 37 | |
| Retained earnings | 2,399 | | | 1,860 | |
| Total stockholders’ equity | 2,630 | | | 2,096 | |
| Total liabilities and stockholders’ equity | $ | 5,434 | | | $ | 4,849 | |
See accompanying notes.
Molina Healthcare, Inc. 2021 Form 10-K | 82
Condensed Statements of Income
| | | | | | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2021 | | 2020 | | 2019 |
| | | | | |
| | (In millions) |
| Revenue: | | | | | |
| Administrative services fees | $ | 1,496 | | | $ | 1,208 | | | $ | 1,038 | |
| Investment income and other revenue | 11 | | | 13 | | | 18 | |
| Total revenue | 1,507 | | | 1,221 | | | 1,056 | |
| Expenses: | | | | | |
| General and administrative expenses | 1,424 | | | 1,089 | | | 937 | |
| Depreciation and amortization | 98 | | | 67 | | | 63 | |
| Other | 5 | | | 24 | | | 4 | |
| Total operating expenses | 1,527 | | | 1,180 | | | 1,004 | |
| Operating (loss) income | (20) | | | 41 | | | 52 | |
| Interest expense | 120 | | | 102 | | | 87 | |
| Other expenses (income), net | 25 | | | 15 | | | (15) | |
| Total other expenses, net | 145 | | | 117 | | | 72 | |
| Loss before income tax (benefit) expense and equity in net earnings of subsidiaries | (165) | | | (76) | | | (20) | |
| Income tax (benefit) expense | (21) | | | (5) | | | 9 | |
| Net loss before equity in net earnings of subsidiaries | (144) | | | (71) | | | (29) | |
| Equity in net earnings of subsidiaries | 803 | | | 744 | | | 766 | |
| Net income | $ | 659 | | | $ | 673 | | | $ | 737 | |
Condensed Statements of Comprehensive Income
| | | | | | | | | | | | | | | | | |
| Year Ended December 31, |
| 2021 | | 2020 | | 2019 |
| | | | | |
| (In millions) |
| Net income | $ | 659 | | | $ | 673 | | | $ | 737 | |
| Other comprehensive (loss) income: | | | | | |
| Unrealized investment (loss) income | (55) | | | 44 | | | 16 | |
| Less: effect of income taxes | (13) | | | 11 | | | 4 | |
| Other comprehensive (loss) income, net of tax | (42) | | | 33 | | | 12 | |
| Comprehensive income | $ | 617 | | | $ | 706 | | | $ | 749 | |
See accompanying notes.
Molina Healthcare, Inc. 2021 Form 10-K | 83
Condensed Statements of Cash Flows
| | | | | | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2021 | | 2020 | | 2019 |
| | | | | |
| | (In millions) |
| Operating activities: | | | | | |
| Net cash provided by operating activities | $ | 60 | | | $ | 67 | | | $ | 71 | |
| Investing activities: | | | | | |
| Capital contributions to subsidiaries | (440) | | | (107) | | | (43) | |
| Dividends received from subsidiaries | 564 | | | 635 | | | 1,373 | |
| Purchases of investments | (27) | | | (188) | | | (152) | |
| Proceeds from sales and maturities of investments | 21 | | | 282 | | | 93 | |
| Purchases of property, equipment and capitalized software | (70) | | | (74) | | | (56) | |
| Net cash paid in business combinations | (263) | | | (1,028) | | | — | |
| Change in amounts due to/from affiliates | 40 | | | (68) | | | 38 | |
| Other, net | (3) | | | 3 | | | 1 | |
| Net cash (used in) provided by investing activities | (178) | | | (545) | | | 1,254 | |
| Financing activities: | | | | | |
| Proceeds from senior notes offering, net of issuance costs | 740 | | | 1,429 | | | — | |
| Repayment of senior notes | (723) | | | (338) | | | — | |
Common stock purchases | (128) | | | (606) | | | (47) | |
| Common stock withheld to settle employee tax obligations | (53) | | | (8) | | | (7) | |
| Contingent consideration liabilities settled | (20) | | | — | | | — | |
| Repayment of term loan facility | — | | | (600) | | | — | |
Proceeds from borrowings under term loan facility | — | | | 380 | | | 220 | |
Cash paid for partial termination of warrants | — | | | (30) | | | (514) | |
Cash paid for partial settlement of conversion option | — | | | (27) | | | (578) | |
Cash received for partial settlement of call option | — | | | 27 | | | 578 | |
Repayment of principal amount of convertible notes | — | | | (12) | | | (240) | |
| Other, net | 1 | | | 2 | | | 29 | |
| Net cash (used in) provided by financing activities | (183) | | | 217 | | | (559) | |
Net (decrease) increase in cash and cash equivalents | (301) | | | (261) | | | 766 | |
Cash and cash equivalents at beginning of period | 575 | | | 836 | | | 70 | |
Cash and cash equivalents at end of period | $ | 274 | | | $ | 575 | | | $ | 836 | |
See accompanying notes.
Notes to Condensed Financial Information of Registrant
Note A - Basis of Presentation
The Registrant was incorporated in 2002. Prior to that date, Molina Healthcare of California (formerly known as Molina Medical Centers) operated as a California health plan and as the parent company for three other state health plans. In June 2003, the employees and operations of the corporate entity were transferred from Molina Healthcare of California to the Registrant.
The Registrant’s investment in subsidiaries is stated at cost plus equity in undistributed earnings of subsidiaries since the date of acquisition. The accompanying condensed financial information of the Registrant should be read in conjunction with the consolidated financial statements and accompanying notes.
Note B - Transactions with Subsidiaries
The Registrant provides certain centralized medical and administrative services to our subsidiaries pursuant to administrative services agreements that include, but are not limited to, information technology, product development
Molina Healthcare, Inc. 2021 Form 10-K | 84
and administration, underwriting, claims processing, customer service, certain care management services, human resources, marketing, purchasing, risk management, actuarial, finance, accounting, compliance, legal and public relations. Fees are based on the fair market value of services rendered and are recorded as operating revenue. Payment is subordinated to the subsidiaries’ ability to comply with minimum capital and other restrictive financial requirements of the states in which they operate. Charges in 2021, 2020, and 2019 for these services amounted to $1,496 million, $1,208 million, and $1,038 million, respectively, and are included in operating revenue.
The Registrant and its subsidiaries are included in the consolidated federal and state income tax returns filed by the Registrant. Income taxes are allocated to each subsidiary in accordance with an intercompany tax allocation agreement. The agreement allocates income taxes in an amount generally equivalent to the amount which would be expensed by the subsidiary if it filed a separate tax return. Net operating loss benefits are paid to the subsidiary by the Registrant to the extent such losses are utilized in the consolidated tax returns.
Note C - Dividends and Capital Contributions
When the Registrant receives dividends from its subsidiaries, such amounts are recorded as a reduction to the investments in the respective subsidiaries.
For all periods presented, the Registrant made capital contributions to certain subsidiaries primarily to comply with minimum net worth requirements and to fund business combinations. Such amounts have been recorded as an increase in investment in the respective subsidiaries.
Molina Healthcare, Inc. 2021 Form 10-K | 85
CONTROLS AND PROCEDURES
MANAGEMENT’S EVALUATION OF DISCLOSURE CONTROLS AND PROCEDURES
We maintain disclosure controls and procedures, as defined in Rule 13a-15(e) and Rule 15d-15(e) under the Securities Exchange Act of 1934, as amended (the “Exchange Act”), that are designed to provide reasonable assurance that information required to be disclosed by us in reports we file or submit under the Exchange Act is recorded, processed, summarized and reported within the time periods specified in the SEC's rules and forms. Disclosure controls and procedures include, without limitation, controls and procedures designed to provide reasonable assurance that information required to be disclosed by us in reports we file or submit under the Exchange Act is accumulated and communicated to our management, including our principal executive officer and principal financial officer or persons performing similar functions, as appropriate, to allow timely decisions regarding required disclosure. In designing and evaluating the disclosure controls and procedures, management recognizes that any controls and procedures, no matter how well designed and operated, can provide only reasonable assurance of achieving the desired control objectives, and management is required to apply its judgment in evaluating the cost-benefit relationship of any possible controls and procedures.
Under the supervision and with the participation of our management, including our chief executive officer and our chief financial officer, we carried out an evaluation of the effectiveness of our disclosure controls and procedures as of the end of the period covered by this Form 10-K pursuant to Rule 13a-15(b) and Rule 15d-15(b) of the Exchange Act. Based on this evaluation, our chief executive officer and our chief financial officer concluded that our disclosure controls and procedures were effective as of December 31, 2021, at the reasonable assurance level. In addition, management concluded that our consolidated financial statements included in this Annual Report on Form 10-K are fairly stated in all material respects in accordance with U.S. generally accepted accounting principles (“GAAP”) for each of the periods presented herein.
MANAGEMENT’S REPORT ON INTERNAL CONTROL OVER FINANCIAL REPORTING
Management is responsible for establishing and maintaining adequate internal control over financial reporting, as such term is defined in Rule 13a-15(f) under the Exchange Act. Our internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of our assets; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with GAAP, and that our receipts and expenditures are being made only in accordance with authorizations of our management and directors; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of our assets that could have a material effect on our financial statements.
Internal control over financial reporting is designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements prepared for external purposes in accordance with GAAP. Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of the effectiveness of our internal control over financial reporting to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
Management concluded that we maintained effective internal control over financial reporting as of December 31, 2021, based on criteria described in Internal Control-Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission (“COSO”).
Ernst & Young, LLP, the independent registered public accounting firm who audited our Consolidated Financial Statements included in this Form 10-K, has issued a report on our internal control over financial reporting, which is included herein.
Changes in Internal Control over Financial Reporting
There were no changes in our internal control over financial reporting (as defined in Rule 13a-15(f) of the Exchange Act) during the quarter ended December 31, 2021, that has materially affected, or is reasonably likely to materially affect, our internal control over financial reporting.
Molina Healthcare, Inc. 2021 Form 10-K | 86
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Stockholders and the Board of Directors of Molina Healthcare, Inc.
Opinion on Internal Control Over Financial Reporting
We have audited Molina Healthcare, Inc.’s internal control over financial reporting as of December 31, 2021, based on criteria established in Internal Control-Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) (the “COSO criteria”). In our opinion, Molina Healthcare, Inc. (the “Company”) maintained, in all material respects, effective internal control over financial reporting as of December 31, 2021, based on the COSO criteria.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (“PCAOB”), the consolidated balance sheets of the Company as of December 31, 2021 and 2020, the related consolidated statements of income, comprehensive income, stockholders’ equity and cash flows for each of the three years in the period ended December 31, 2021, and the related notes and our report dated February 14, 2022, expressed an unqualified opinion thereon.
Basis for Opinion
The Company’s management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting included in the accompanying Management’s Report on Internal Control Over Financial Reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audit in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects.
Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
Definition and Limitations of Internal Control Over Financial Reporting
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
/s/ Ernst & Young LLP
Los Angeles, California
February 14, 2022
Molina Healthcare, Inc. 2021 Form 10-K | 87
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Stockholders and the Board of Directors of Molina Healthcare, Inc.
Opinion on the Financial Statements
We have audited the accompanying consolidated balance sheets of Molina Healthcare, Inc. (the “Company”) as of December 31, 2021 and 2020, the related consolidated statements of income, comprehensive income, stockholders’ equity and cash flows for each of the three years in the period ended December 31, 2021, and the related notes (collectively referred to as the “consolidated financial statements”). In our opinion, the consolidated financial statements present fairly, in all material respects, the financial position of the Company at December 31, 2021 and 2020, and the results of its operations and its cash flows for each of the three years in the period ended December 31, 2021, in conformity with U.S. generally accepted accounting principles.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (“PCAOB”), the Company’s internal control over financial reporting as of December 31, 2021, based on criteria established in Internal Control-Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework), and our report dated February 14, 2022, expressed an unqualified opinion thereon.
Basis for Opinion
These financial statements are the responsibility of the Company‘s management. Our responsibility is to express an opinion on the Company‘s financial statements based on our audits. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
Critical Audit Matters
The critical audit matters communicated below are matters arising from the current period audit of the financial statements that were communicated or required to be communicated to the audit committee and that: (1) relate to accounts or disclosures that are material to the financial statements and (2) involved our especially challenging, subjective or complex judgments. The communication of critical audit matters does not alter in any way our opinion on the consolidated financial statements, taken as a whole, and we are not, by communicating the critical audit matters below, providing a separate opinion on the critical audit matters or on the accounts or disclosures to which they relate.
| | | | | | | | |
| | Valuation of incurred but not paid fee-for-service claims |
| | |
| Description of the matter | | As of December 31, 2021, the Company’s liability for fee-for-service claims incurred but not paid (“IBNP”), comprised $2,486 million of the $3,363 million of Medical Claims and Benefits Payable. As discussed in Note 10 to the consolidated financial statements, the Company’s IBNP liability is determined using actuarial methods that include a number of factors and assumptions, including completion factors, which seek to measure the cumulative percentage of claims expense that will have been paid for a given month of service as of the reporting date, based on historical payment patterns, and assumed health care cost trend factors, which represent an estimate of claims expense based on recent claims expense levels and healthcare cost levels. There is significant uncertainty inherent in determining management’s best estimate of completion and trend factors, which are used to calculate actuarial estimates of incurred but not paid claims. |
| | |
Molina Healthcare, Inc. 2021 Form 10-K | 88
| | | | | | | | |
| | Auditing management’s best estimate of the IBNP liability was complex and required the involvement of our actuarial specialists due to the highly judgmental nature of completion and trend factor assumptions used in the valuation process. These assumptions have a significant effect on the valuation of the IBNP liability. |
| | |
| How we addressed the matter in our audit | | We obtained an understanding, evaluated the design, and tested the operating effectiveness of the Company’s controls over the process for estimating the IBNP liability. This included testing management review controls over completion and trend factor assumptions, and management’s review and approval of actuarial methods used to calculate IBNP liability, including the data inputs and outputs of those models. |
| | |
| | To test IBNP liability, our audit procedures included, among others, testing the completeness and accuracy of data used in the calculation by testing reconciliations of underlying claims and membership data recorded in source systems to the actuarial reserving calculations, and comparing a sample of claims to source documentation. With the assistance of EY actuarial specialists, we evaluated the Company’s selection and weighting of actuarial methods by comparing the weightings used in the current estimate to those used in prior periods and those used in the industry for the specific types of insurance. To evaluate significant assumptions used by management in the actuarial methods, we compared assumptions to current and historical claims trends, to those used historically and to current industry benchmarks. We also compared management’s recorded IBNP liability to a range of reasonable IBNP estimates calculated independently by our EY actuarial specialists. Additionally, we performed a review of the prior period estimates using subsequent claims development, and we reviewed and evaluated management’s disclosures surrounding fee-for-service claims IBNP. |
/s/ Ernst & Young LLP
We have served as the Company’s auditor since 2000.
Los Angeles, California
February 14, 2022
Molina Healthcare, Inc. 2021 Form 10-K | 89
OTHER INFORMATION
None.
DIRECTORS, EXECUTIVE OFFICERS, AND CORPORATE GOVERNANCE
Information required by Item 10 of Part III will be included in our Proxy Statement relating to our 2022 Annual Meeting of Stockholders (the “2022 Proxy Statement”), and is incorporated herein by reference. This information will be included in the following sections of the 2022 Proxy Statement:
•PROPOSAL 1 - Election of Directors
•Information About Director Nominees
•Information About Directors Continuing in Office
•Additional Information About Directors
•Corporate Governance and Board of Directors Matters
•Information About the Executive Officers of the Company
•Section 16(a) Beneficial Ownership Reporting Compliance
Information relating to our Code of Business Conduct and Ethics and compliance with Section 16(a) of the Exchange Act will be set forth in the 2022 Proxy Statement and is incorporated herein by reference. To the extent permissible under NYSE rules, we intend to disclose amendments to our Code of Business Conduct and Ethics, as well as waivers of the provisions thereof, on our investor relations website under the heading “Investor Information—Corporate Governance” at molinahealthcare.com.
EXECUTIVE COMPENSATION
Information required by Item 11 of Part III will be included in the 2022 Proxy Statement in the section entitled “Executive Compensation,” and is incorporated herein by reference.
SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED SHAREHOLDER MATTERS
Information required by Item 12 of Part III will be included in the 2022 Proxy Statement in the section entitled “Security Ownership of Certain Beneficial Owners and Management,” and is incorporated herein by reference.
CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS, AND DIRECTOR INDEPENDENCE
Information required by Item 13 of Part III will be included in the 2022 Proxy Statement in the sections entitled “Related Party Transactions,” and “Corporate Governance and Board of Directors Matters—Director Independence,” and is incorporated herein by reference.
PRINCIPAL ACCOUNTANT FEES AND SERVICES
Our independent registered public accounting firm is Ernst & Young LLP, Los Angeles, CA, Auditor Firm ID: 42.
Information required by Item 14 of Part III will be included in the 2022 Proxy Statement in the section entitled “Fees Paid to Independent Registered Public Accounting Firm,” and is incorporated herein by reference.
Molina Healthcare, Inc. 2021 Form 10-K | 90
EXHIBITS AND FINANCIAL STATEMENT SCHEDULES
FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA
(1) The consolidated financial statements are included in this report in the section entitled “Financial Statements and Supplementary Data.”
(2) Financial Statement Schedules:
Schedules for which provision is made in the applicable accounting regulations of the SEC are not required under the related instructions, are inapplicable, or the required information is included in the consolidated financial statements, and therefore have been omitted.
EXHIBITS
Reference is made to the accompanying “Index to Exhibits.”
Molina Healthcare, Inc. 2021 Form 10-K | 91
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the undersigned registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized, on the 14th day of February, 2022.
| | | | | | | | | | | |
| MOLINA HEALTHCARE, INC. |
| | | |
| By: | | /s/ Joseph M. Zubretsky |
| | | Joseph M. Zubretsky |
| | | Chief Executive Officer
(Principal Executive Officer) |
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the registrant and in the capacities as indicated, as of February 14, 2022.
| | | | | | | | |
| Signature | | Title |
| | |
| /s/ Joseph M. Zubretsky | | Chief Executive Officer, President and Director |
| Joseph M. Zubretsky | | (Principal Executive Officer) |
| | |
| /s/ Mark L. Keim | | Chief Financial Officer |
| Mark L. Keim | | (Principal Financial Officer) |
| | |
| /s/ Maurice S. Hebert | | Chief Accounting Officer |
| Maurice S. Hebert | | (Principal Accounting Officer) |
| | |
| /s/ Barbara L. Brasier | | Director |
| Barbara L. Brasier | | |
| | |
| /s/ Daniel Cooperman | | Director |
| Daniel Cooperman | | |
| | |
| /s/ Stephen H. Lockhart | | Director |
| Stephen H. Lockhart | | |
| | |
| /s/ Steven J. Orlando | | Director |
| Steven J. Orlando | | |
| | |
| /s/ Ronna E. Romney | | Director |
| Ronna E. Romney | | |
| | |
| /s/ Richard M. Schapiro | | Director |
| Richard M. Schapiro | | |
| | |
| /s/ Dale B. Wolf | | Chairman of the Board |
| Dale B. Wolf | | |
| | |
| /s/ Richard C. Zoretic | | Director |
| Richard C. Zoretic | | |
Molina Healthcare, Inc. 2021 Form 10-K | 92
INDEX TO EXHIBITS
The following exhibits, which are furnished with this Annual Report on Form 10-K (this “Form 10-K”) or incorporated herein by reference, are filed as part of this annual report.
The agreements included or incorporated by reference as exhibits to this Form 10-K may contain representations and warranties by each of the parties to the applicable agreement. These representations and warranties were made solely for the benefit of the other parties to the applicable agreement and (i) were not intended to be treated as categorical statements of fact, but rather as a way of allocating the risk to one of the parties if those statements prove to be inaccurate; (ii) may have been qualified in such agreement by disclosures that were made to the other party in connection with the negotiation of the applicable agreement; (iii) may apply contract standards of “materiality” that are different from “materiality” under the applicable securities laws; and (iv) were made only as of the date of the applicable agreement or such other date or dates as may be specified in the agreement. The Company acknowledges that, notwithstanding the inclusion of the foregoing cautionary statements, it is responsible for considering whether additional specific disclosures of material information regarding material contractual provisions are required to make the statements in this Form 10-K not misleading.
| | | | | | | | | | | | | | |
| Number | | Description | | Method of Filing |
| 2.1 | | | | Filed as Exhibit 2.1 to registrant’s Form 8-K filed May 6, 2020 |
| 2.2 | | | | Filed as Exhibit 2.1 to registrant’s Form 10-Q filed October 29, 2020 |
| 3.1 | | | | Filed as Exhibit 3.2 to registrant’s Registration Statement on Form S-1 filed December 30, 2002 |
| 3.2 | | | | Filed as Appendix A to registrant’s Definitive Proxy Statement on Form DEF 14A filed March 25, 2013 |
| 3.3 | | | | Filed as Appendix A to registrant’s Definitive Proxy Statement on Form DEF 14A filed March 25, 2019 |
| 3.4 | | | | Filed as Exhibit 3.3 to registrant’s Form 10-K filed February 19, 2019 |
| 4.1 | | | | Filed as Exhibit 4.1 to registrant’s Form 8-K filed June 2, 2020 |
| 4.2 | | | | Filed as Exhibit 4.2 to registrant’s Form 8-K filed June 2, 2020 (Included in Exhibit 4.1 to registrant’s Form 8-K filed June 2, 2020) |
| 4.3 | | | | Filed as Exhibit 4.1 to registrant’s Form 8-K filed November 17, 2020 |
| 4.4 | | | | Filed as Exhibit 4.2 to registrant’s Form 8-K filed November 17, 2020 (Included in Exhibit 4.1 to registrant’s Form 8-K filed November 17, 2020) |
| 4.5 | | | | Filed as Exhibit 4.1 to registrant’s Form 8-K filed November 16, 2021 |
| 4.6 | | | | Filed as Exhibit 4.2 to registrant’s Form 8-K filed November 16, 2021 (Included in Exhibit 4.1 to registrant’s Form 8-K filed November 16, 2021) |
| 4.7 | | | | Filed as Exhibit 4.9 to registrant’s Form 10-K filed February 16, 2021 |
| 10.1 | | | | Filed as Exhibit 10.1 to registrant’s Form 8-K filed June 8, 2020 |
| *10.2 | | | | Filed as Appendix C to registrant’s Definitive Proxy Statement on Form DEF 14A filed March 25, 2019 |
Molina Healthcare, Inc. 2021 Form 10-K | 93
| | | | | | | | | | | | | | |
| Number | | Description | | Method of Filing |
| *10.3 | | | | Filed as Appendix B to registrant’s Definitive Proxy Statement on Form DEF 14A filed March 25, 2019 |
| *10.4 | | | | Filed as Exhibit 10.1 to registrant’s Form 10-Q filed July 31, 2019 |
| *10.5 | | | | Filed as Exhibit 10.2 to registrant’s Form 10-Q filed July 31, 2019 |
| *10.6 | | | | Filed as Exhibit 10.3 to registrant’s Form 10-Q filed July 31, 2019 |
| *10.7 | | | | Filed as Exhibit 10.4 to registrant’s Form 10-Q filed July 31, 2019 |
| *10.8 | | | | Filed as Exhibit 10.14 to registrant’s Form 10-K filed February 16, 2021 |
| *10.9 | | | | Filed as Exhibit 10.14 to registrant’s Form 10-K filed March 14, 2007 |
| *10.10 | | | | Filed herewith |
| *10.11 | | | | Filed as Exhibit 10.3 to registrant’s Form 8-K filed June 14, 2013 |
| *10.12 | | | | Filed as Exhibit 10.16 to registrant’s Form 10-K filed February 28, 2013 |
| *10.13 | | | | Filed as Exhibit 10.1 to registrant’s Form 8-K filed September 9, 2021 |
| *10.14 | | | | Filed as Exhibit 10.1 to registrant’s Form 8-K filed November 17, 2020 |
| +10.15 | | | | Filed as Exhibit 10.36 to registrant’s Form 10-K filed February 19, 2019
|
| 10.16 | | | | Filed as Exhibit 10.1 to registrant’s Form 10-Q filed October 30, 2019 |
| 21.1 | | | | Filed herewith |
| 23.1 | | | | Filed herewith |
| 31.1 | | | | Filed herewith |
| 31.2 | | | | Filed herewith |
| 32.1 | | | | Filed herewith |
| 32.2 | | | | Filed herewith |
| 101.INS | | Inline XBRL Taxonomy Instance Document - the instance document does not appear in the Interactive Data File because its XBRL tags are embedded within the inline XBRL document. | | Filed herewith |
| 101.SCH | | Inline XBRL Taxonomy Extension Schema Document | | Filed herewith |
| 101.CAL | | Inline XBRL Taxonomy Extension Calculation Linkbase Document | | Filed herewith |
| 101.DEF | | Inline XBRL Taxonomy Extension Definition Linkbase Document | | Filed herewith |
| 101.LAB | | Inline XBRL Taxonomy Extension Label Linkbase Document | | Filed herewith |
| 101.PRE | | Inline XBRL Taxonomy Extension Presentation Linkbase Document | | Filed herewith |
| 104 | | Cover Page Interactive Data file (formatted as Inline XBRL and embedded within Exhibit 101) | | Filed herewith |
Molina Healthcare, Inc. 2021 Form 10-K | 94
| | | | | |
| * | Management contract or compensatory plan or arrangement required to be filed (and/or incorporated by reference) as an exhibit to this Annual Report on Form 10-K pursuant to Item 15(b) of Form 10-K. |
| ** | Certain portions of this agreement have been omitted in accordance with Item 601(b)(10) of Regulation S-K. A copy of any omitted portion will be furnished to the Securities and Exchange Commission upon request. |
| + | Portions of this exhibit have been omitted pursuant to a request for confidential treatment filed with the Securities and Exchange Commission under Rule 24b-2. The omitted confidential material has been filed separately. The location of the redacted confidential information is indicated in the exhibit as “[redacted]”. |
Molina Healthcare, Inc. 2021 Form 10-K | 95