UNITED STATES SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
Form
(Mark One)
ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
|
|
|
|
For the fiscal year ended |
|
Or |
TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
|
|
|
|
For the transition period from to |
Commission file number
(Exact name of registrant as specified in its charter)
(State or other jurisdiction of incorporation or organization) |
(IRS Employer Identification No.) |
|
|
(Address of principal executive offices) |
(Zip Code) |
Registrant’s telephone number, including area code:
(
Securities registered pursuant to Section 12(b) of the Act:
|
|
|
Title of Each Class |
Trading Symbol(s) |
Name of Each Exchange on Which Registered |
Securities registered pursuant to Section 12(g) of the Act: None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ☐
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or 15(d) of the Act. Yes ☐
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days.
Indicate by check mark whether the registrant has submitted electronically every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S-T (§ 232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit such files).
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer,” “smaller reporting company” and “emerging growth company” in Rule 12b-2 of the Exchange Act:
|
|
|
|
|
Large accelerated filer ☐ |
Smaller reporting company |
|
|
Non-accelerated filer ☐ |
Emerging growth company |
|
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ☐
Indicate by check mark whether the registrant has filed a report on and attestation to its management’s assessment of the effectiveness of its internal control over financial reporting under Section 404(b) of the Sarbanes-Oxley Act (15 U.S.C. 7262(b)) by the registered public accounting firm that prepared or issued its audit report.
If securities are registered pursuant to Section 12(b) of the Act, indicate by check mark whether the financial statements of the registrant included in the filing reflect the correction of an error to previously issued financial statements.
Indicate by check mark whether any of those error corrections are restatements that required a recovery analysis of incentive-based compensation received by any of the registrant’s executive officers during the relevant recovery period pursuant to §240.10D-1(b). ☐
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act). Yes
The aggregate market value of the voting stock held by non-affiliates of the Registrant was $
DOCUMENTS INCORPORATED BY REFERENCE
Certain information required for Part III of this annual report is incorporated by reference to portions of the Registrant’s definitive proxy statement for its 2024 annual meeting of stockholders to be filed with the Securities and Exchange Commission within 120 days after the end of the Registrant’s fiscal year ended December 31, 2023.
TABLE OF CONTENTS
COMMUNITY HEALTH SYSTEMS, INC.
Year ended December 31, 2023
|
|
|
Page |
|
PART I |
|
|
|
|
|
|
Item 1. |
|
1 |
|
Item 1A. |
|
24 |
|
Item 1B. |
|
44 |
|
Item 1C. |
|
44 |
|
Item 2. |
|
45 |
|
Item 3. |
|
48 |
|
Item 4. |
|
50 |
|
|
|
|
|
|
PART II |
|
|
|
|
|
|
Item 5. |
|
51 |
|
Item 6. |
|
52 |
|
Item 7. |
Management’s Discussion and Analysis of Financial Condition and Results of Operations |
|
53 |
Item 7A. |
|
72 |
|
Item 8. |
|
73 |
|
Item 9. |
Changes in and Disagreements with Accountants on Accounting and Financial Disclosure |
|
118 |
Item 9A. |
|
118 |
|
Item 9B. |
|
118 |
|
Item 9C. |
Disclosure Regarding Foreign Jurisdictions that Prevent Inspections |
|
118 |
|
|
|
|
|
PART III |
|
|
|
|
|
|
Item 10. |
|
121 |
|
Item 11. |
|
122 |
|
Item 12. |
Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters |
|
122 |
Item 13. |
Certain Relationships and Related Transactions, and Director Independence |
|
122 |
Item 14. |
|
122 |
|
|
|
|
|
|
PART IV |
|
|
|
|
|
|
Item 15. |
|
123 |
|
Item 16. |
|
130 |
Item 1. Business of Community Health Systems, Inc.
Overview of Our Company
We are one of the nation’s largest healthcare companies. Our affiliates are leading providers of healthcare services, developing and operating healthcare delivery systems in 40 distinct markets across 15 states. As of December 31, 2023, our subsidiaries own or lease 71 affiliated hospitals, with approximately 12,000 beds, and operate more than 1,000 sites of care, including physician practices, urgent care centers, freestanding emergency departments, occupational medicine clinics, imaging centers, cancer centers and ambulatory surgery centers. We generate revenues by providing a broad range of general and specialized hospital healthcare services and outpatient services to patients in the communities in which we are located. For the hospitals that we own and operate, we are paid for our services by governmental agencies, private insurers and directly by the patients we serve. Services provided through our hospitals and outpatient facilities include general acute care, emergency room, general and specialty surgery, critical care, internal medicine, obstetrics, diagnostic, psychiatric and rehabilitation services. An integral part of providing these services is our network of affiliated physicians at our hospitals and affiliated businesses. As of December 31, 2023, we employed approximately 1,500 physicians and an additional 1,100 licensed healthcare practitioners. Through our management and operation of these businesses, we provide standardization and centralization of operations across key business areas; strategic assistance to expand and improve services and facilities; implementation of patient safety and quality of care improvement programs and assistance in the recruitment of additional physicians and licensed healthcare practitioners to the markets in which our hospitals are located. In a number of our markets, we have partnered with local physicians, for-profit entities and/or not-for-profit providers in the ownership of our facilities.
Throughout this Form 10-K, we refer to Community Health Systems, Inc., or the Parent Company, and its consolidated subsidiaries in a simplified manner and on a collective basis, using words like “we,” “our,” “us” and the “Company.” This drafting style is suggested by the Securities and Exchange Commission, or SEC, and is not meant to indicate that the publicly-traded Parent Company or any particular subsidiary of the Parent Company owns or operates any asset, business or property. The hospitals, operations and businesses described in this filing are owned and operated, and management services provided, by distinct and indirect subsidiaries of Community Health Systems, Inc.
Available Information
Our website address is www.chs.net and the investor relations section of our website is located at www.chs.net/investor-relations. Notwithstanding the foregoing, the information contained on our website as noted above or elsewhere in this Form 10-K is not incorporated by reference into this Form 10-K. We make available free of charge, through the investor relations section of our website, annual reports on Form 10-K, quarterly reports on Form 10-Q and current reports on Form 8-K as well as amendments to those reports, as soon as reasonably practical after they are filed with, or furnished to, the SEC. The SEC maintains a website that contains our reports, proxy and information statements, and other information that we file electronically with the SEC at www.sec.gov.
We also make available free of charge, through the investor relations section of our website, our By-laws, our Governance Guidelines, our Code of Conduct and the charters of our Audit and Compliance Committee, Compensation Committee and Governance and Nominating Committee.
We have included the Chief Executive Officer and the Chief Financial Officer certifications regarding the public disclosure required by Sections 302 and 906 of the Sarbanes-Oxley Act of 2002 as Exhibits 31.1, 31.2, 32.1 and 32.2 to this Form 10-K.
Our Business Strategy
The key elements of our business strategy are to:
Become a market leader and increase market share in the communities we serve
We operate across diverse markets that range from sole community providers to large regional networks. We are able to leverage our significant scale and standardized systems to provide cost-effective services and best practices for our affiliate operations. Each of our markets develops and executes a strategic plan with short- and long-term goals, based on their unique opportunities and the needs of their respective communities. In addition, as an organization, we have implemented a number of strategic initiatives designed to improve market position, expand services to our patients, and capture a greater share of healthcare spending in our markets. These include:
1
Strengthening Regional Networks and Local Market Operations. We believe opportunities exist in select markets to create healthcare networks consisting of multiple hospitals and corresponding outpatient services.
Regional networks are able to expand the breadth of services provided for our patients, centralize key services, deliver care in an organized and efficient way across the network, improve alignment with physicians and other providers, and make services more attractive to managed care and other payors. Currently, 43 of our hospitals operate in 12 unique regional networks.
We also operate healthcare systems that are built around a single acute-care hospital. In these markets, we are focused on supporting the hospital with physician practices, outpatient services, clinical collaborations and partnerships that offer our patients health services across the continuum of care. These hospitals and their related outpatient services may operate in competitive markets or as sole community providers.
Expanding Patient Access Points, Health Services and Infrastructure. When expanding services—in both the acute and non-acute care settings—our approach is data-driven and strategic to ensure our investments are responsive to community and patient needs and produce sound financial results. While we continue to provide health services across a broad spectrum, we have focused our attention and resources on service lines we believe have the greatest potential for growth, including primary care, emergency medicine, orthopedics, neuroscience, cardiovascular care, surgical services and behavioral health. Significant investments have been made in existing markets to expand the scale of inpatient offerings, including through increasing bed capacity and constructing new surgical and procedural suites. As the shift to delivering health services in outpatient settings accelerates, we continue to expand our care offerings beyond hospital walls to include more outpatient access through primary care practices, urgent care centers, free-standing emergency departments, ambulatory surgery centers, imaging and diagnostic centers and direct-to-consumer virtual health visits. We endeavor to advance the scale and breadth of inpatient and outpatient capabilities through both direct investments and strategic partnerships.
We believe expanding our patient access footprint can attract new patients and increase patient retention, as well as our ability to connect patients from one episode of care to the next appropriate care setting. We also believe our investments will enhance our long-term growth and generate increased revenue, earnings, and operating margins by providing a solid return on investment.
Recruiting and/or Employing Additional Primary Care Physicians and Specialists. The physician-patient relationship is the foundation on which healthcare services are built. Understanding this, we continuously assess our communities to identify service gaps and practice opportunities in order to recruit an optimal mix of primary care physicians and specialists. We analyze demographic data and referral trends and employ recruiters at the corporate level to support local hospital administrators in their physician recruitment efforts. In some markets, we employ physicians through recruitment or acquisition of their existing practices. However, most physicians in our communities and on our medical staffs remain in private practice and are not our employees.
We work hard to develop positive, collaborative relationships with physicians. We currently participate in 11 Medicare Shared Savings Program Accountable Care Organizations, which include approximately 3,500 employed and independent physicians in our communities. We look forward to continuing to realize the benefits of these organizations, including opportunities to strengthen quality, deepen clinical collaboration and demonstrate performance under a reimbursement system moving toward more value-based incentives and payments.
Developing a More Consumer-Centric Experience and Facilitating Connections between Episodes of Care. Consumers continue to take a more active role in healthcare decision-making, especially as they assume increasing responsibility for the cost of their healthcare. The rise in consumerism is highlighting customer expectations that have not always been prioritized in the healthcare setting. We are working on ways to create more enduring relationships with our patients by providing services that help people navigate their healthcare journeys and enable more seamless connections across episodes of care in our healthcare systems, hospitals, and physician practices. Some of these initiatives include:
2
Increase productivity and operating efficiencies to enhance profitability
Our hospital management teams are supported by experienced corporate leaders who have significant industry knowledge and a proven track record of success. Local hospitals benefit from centralized clinical, operational, financial and regulatory expertise that encompasses nearly every aspect of our business. Additionally, we are able to leverage deep and meaningful data sources to facilitate informed decision-making and drive operational improvements across the enterprise in areas such as drug and supply procurement, workforce optimization and staffing and emergency department and operating room performance.
Standard policies and procedures in areas ranging from physician practice management to patient accounting to construction and facilities management help to facilitate best practices, reduce variation and improve operating results. The following areas highlight some of our standardized and centralized platforms.
Billing and Collections. We have adopted standard policies and procedures with respect to billing and collections. We have automated various components of the collection cycle, including statements and collection letters, to help facilitate timely and accurate progression of our accounts through the collection cycle. We have consolidated local hospital billing and collection functions into three centralized business offices and have completed the transition of our hospital billing departments to this new infrastructure. These efforts have resulted in lower patient claim denials, higher underpayment recoveries and reduced operating costs.
Physician Support. We support newly recruited physicians to facilitate a smooth and effective transition into our communities. We have implemented programs to improve physician workflow, reduce physician turnover, optimize staffing at physician clinics and standardize onboarding processes.
Human Resources. We have created a centralized nurse recruitment program to support our hospitals in their efforts to recruit the nurses needed for the delivery of high quality care, which are a priority due to workforce shortages across the healthcare industry. We also operate nursing school programs on some of our hospital campuses and partner with nursing schools in many of our communities. In addition, we have expanded programs aimed at employee retention and satisfaction, including an expanded employee benefits program with higher levels of tuition reimbursement and student loan support. We also operate leadership development programs and have established rewards and recognition initiatives.
Procurement and Materials Management. We have standardized and centralized supply chain operations to improve procurement of the medical supplies, equipment and pharmaceuticals used in our hospitals. We have a noncontrolling ownership interest in and participation agreement with HealthTrust Purchasing Group, L.P., or HealthTrust, a group purchasing organization, or GPO, which benefits members through scaled pricing. HealthTrust contracts with certain vendors who supply a substantial portion of our medical supplies, equipment and pharmaceuticals.
Case and Resource Management. The primary goal of our case management program is to deliver safe, high-quality care in an efficient and cost effective manner. The program focuses on:
Our case management program integrates the functions of utilization review, discharge planning, assessment of medical necessity and resource management. Patients are assessed upon presentation to the hospital and throughout their course of care with ongoing reviews. Industry-standard criteria are utilized in patient assessments and discharge plans are adjusted according to patient needs. Cases are monitored to prevent delays in service or unnecessary utilization of resources. When a patient is ready for discharge, a case manager works with the patient’s attending physician to evaluate and coordinate the patient’s needs for continued care in the post-acute setting.
Continuously improve patient safety and quality of care
We maintain quality assurance programs to monitor, support and advance quality of care standards and to meet Medicare and Medicaid accreditation and regulatory requirements. We maintain an emphasis on patient safety and clinical outcomes and we are continuously focused on ways to improve patient, physician and employee satisfaction. We believe that a focus on continuous improvement yields the best results for patients, reduces risk and liability, and creates value for the people and communities we serve.
3
We have developed and implemented programs to support and monitor patient safety and quality of care that include:
We have also expanded our network of outpatient services to create greater access and more convenience for our patients, including through significant expansion of our ability to provide remote patient care.
We have operated a Patient Safety Organization, or PSO, since 2012. Our PSO is listed by the U.S. Department of Health and Human Services, or HHS, Agency for Healthcare Research and Quality. We believe our PSO has assisted, and will continue to assist us, in improving patient safety at our hospitals. The PSO has been recertified by the Agency for Healthcare Research and Quality through 2026.
Over the past decade, we have instituted numerous programs to improve safety in our hospitals and other patient care environments. We are also deploying innovative programs to deliver better outcomes including, for example, remote monitoring for patients with certain chronic conditions, maternal/fetal monitoring using machine learning and artificial intelligence, as well as tele-sitting technology.
Industry Overview
According to the Centers for Medicare & Medicaid Services, or CMS, national healthcare expenditures grew 4.1% in 2022 to over $4.4 trillion, an increase from the growth of 3.2% experienced in 2021. The increase in 2022 reflected strong growth in Medicaid and private health insurance spending that was partially offset by continued declines in federal spending associated with developments regarding the COVID-19 pandemic. National healthcare expenditures accounted for approximately 17.3% of total U.S. gross domestic product in 2022. CMS projections indicate that total U.S. healthcare spending is expected to grow at an average annual rate of 5.5% for 2024 through 2031. CMS anticipates that total U.S. healthcare annual expenditures will exceed $7.1 trillion by 2031, accounting for approximately 19.6% of the total U.S. gross domestic product. The CMS projections of healthcare spending are constructed using a current-law framework. The most recent historical data was published in December 2023, and the most recent projections for future years were published in June 2023, and do not take into account the actual expenditures in 2023. Since the health sector has been significantly affected by the COVID-19 pandemic since 2020, CMS expects that the unwinding of various measures related to the COVID-19 public health emergency will affect projected trends. CMS expects the expiration of pandemic-related provisions, coupled with recent legislation, to impact health insurance enrollment trends. Going forward, CMS expects changes in spending growth to be influenced more by health-specific factors, such as medical-specific price inflation, the use and intensity of medical care, and demographic impacts associated with the continuing enrollment of the baby-boom generation in Medicare, and less by federal supplemental payments to providers and federal public health spending.
Hospital services, the market within the healthcare industry in which we primarily operate, is the largest single category of healthcare expenditures. Hospital care expenditures totaled nearly $1.4 trillion in 2022, an increase of 2.2% over 2021, slowing in comparison to the growth rate of 4.5% in 2021. The slower growth rate in 2022 was driven by slower growth in spending for hospital care by private health insurance, Medicare and Medicaid, and by a decline in other private revenues. Trends in hospital prices and use of services also contributed to the lower growth in 2022. CMS projects that the hospital services category will grow at an average of 6.1% annually from 2024 through 2031, reaching over $2.3 trillion by 2031.
U.S. Hospital Industry. The U.S. hospital industry is broadly defined to include acute care, rehabilitation and psychiatric facilities that are either public (government owned and operated), not-for-profit private (religious or secular), or for-profit institutions (investor owned). According to the American Hospital Association, there are approximately 5,000 community hospitals in the U.S., which are not-for-profit owned, investor owned, or state or local government owned. Of these hospitals, approximately 35% are located in communities not located within a metropolitan area designated by the U.S. Office of Management and Budget and the Census Bureau. We believe that a majority of these hospitals are owned by not-for-profit or governmental entities. These facilities offer a broad range of healthcare services, including internal medicine, general surgery, cardiology, oncology, orthopedics, OB/GYN and emergency services. In addition, hospitals offer other ancillary services, including psychiatric, diagnostic, rehabilitation, home care and outpatient surgery services.
4
Factors Affecting Performance. Among the many factors that can influence a hospital’s financial and operating performance are:
Patients needing the most complex care are more often served by the larger and/or more specialized urban hospitals. We believe opportunities exist in selected urban markets to create networks between urban hospitals and non-urban hospitals in order to expand the breadth of services offered in the non-urban hospitals while improving physician alignment in those markets and making them more attractive to managed care organizations.
Hospital Industry Trends
Demographic Trends. According to the U.S. Census Bureau, in 2023, there were nearly 58 million Americans aged 65 or older in the U.S., comprising approximately 17.3% of the total U.S. population. By the year 2030, the number of Americans aged 65 or older is expected to climb to 71 million, or 20.6% of the total population. The number of people aged 85 and older is also expected to increase from 6 million in 2022 to 9 million by the year 2030. These anticipated increases will increase demand for healthcare services and, as importantly, the demand for innovative, more sophisticated means of delivering those services. Hospitals, as the largest category of care in the healthcare market, will be among those impacted most directly by this increase in demand. Based on data compiled for us, the populations of the service areas where our hospitals are located grew 6.7% from 2018 to 2023 and are expected to grow by 2.6% from 2023 to 2028. The number of people aged 65 or older in these service areas grew by 16.4% from 2018 to 2023 and is expected to grow by 13.5% from 2023 to 2028. People aged 65 or older comprised 18.6% of the total population in our service areas in 2023, and they may comprise an estimated 20.6% of the total population in our service areas by 2028.
Consolidation. In addition to our own acquisitions and dispositions in recent years, consolidation activity in the hospital industry, primarily through mergers and acquisitions involving both for-profit and not-for-profit hospital systems, is continuing. Reasons for this activity include:
The payor industry is also consolidating and acquiring health services providers in an effort to offer more expansive, competitive programs.
Trends in Payment for Healthcare Services. As discussed in more detail in the Government Regulation section of this Form 10-K, growing financial and economic pressures on the healthcare industry have resulted in a shift away from traditional reimbursement models. Government and private third-party payors are increasingly adopting and exploring value-based purchasing initiatives, which typically emphasize the cost-effective delivery of care and quality of outcomes. In addition, health insurance coverage models have evolved, with increased enrollment in Medicare Managed Care and Medicaid managed care programs and in high-deductible health plans. We may face greater risk of write-offs of uncollectible amounts from patients enrolled in high-deductible health plans.
5
Shift to Outpatient Services. Because of the growing availability of stand-alone outpatient healthcare facilities, the increase in the services that can be provided at these locations, and payor policies requiring or promoting treatment in outpatient settings, many individuals are seeking a broader range of services at outpatient facilities. This trend has contributed to an increase in outpatient services while inhibiting the growth of inpatient admissions. Changes to Medicare policy affecting the reimbursement methodology for certain items and services provided by off-campus provider-based hospital departments have generally resulted in reduced payment rates for these hospital outpatient settings. In addition, CMS makes annual updates to the Inpatient Only List, which is a list of procedures eligible to be reimbursed by Medicare only if performed in an inpatient setting. To the extent procedures become eligible to be reimbursed by Medicare if performed in outpatient settings, demand for outpatient services may increase in comparison to demand for inpatient services.
Selected Operating Data
The following table sets forth operating statistics for each of the years presented for our hospitals. Statistics for 2023 include a full year of operations for 71 hospitals and partial periods for eight hospitals that were divested, and one hospital in which we sold a majority ownership during the year, reflecting the operations of these hospitals prior to divestiture. Statistics for 2022 include a full year of operations for 79 hospitals and partial periods for one hospital that was divested, one hospital that opened and three hospitals that were closed during the year, reflecting the operations of these hospitals prior to divestiture, opening, or closure as applicable. Statistics for 2021 include a full year of operations for 83 hospitals, and partial periods for five hospitals that were divested reflecting the operations of these hospitals prior to divestiture and one hospital that ceased to operate as a stand-alone hospital and began operating as a campus of another hospital offering only emergency room and outpatient services (statistics for 2021 reflect the operations of that hospital prior to being consolidated into another hospital).
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
|
|
(Dollars in millions) |
|
|||||||||
Consolidated Data |
|
|
|
|
|
|
|
|
|
|||
Number of hospitals (at end of period) |
|
|
71 |
|
|
|
80 |
|
|
|
83 |
|
Licensed beds (at end of period)(1) |
|
|
11,902 |
|
|
|
12,832 |
|
|
|
13,289 |
|
Beds in service (at end of period)(2) |
|
|
10,234 |
|
|
|
10,936 |
|
|
|
11,629 |
|
Admissions(3) |
|
|
435,913 |
|
|
|
434,765 |
|
|
|
442,445 |
|
Adjusted admissions(4) |
|
|
992,552 |
|
|
|
975,737 |
|
|
|
950,717 |
|
Patient days(5) |
|
|
1,957,536 |
|
|
|
2,052,864 |
|
|
|
2,190,405 |
|
Average length of stay (days)(6) |
|
|
4.5 |
|
|
|
4.7 |
|
|
|
5.0 |
|
Occupancy rate (beds in service)(7) |
|
|
52.4 |
% |
|
|
49.2 |
% |
|
|
51.1 |
% |
Net operating revenues |
|
$ |
12,490 |
|
|
$ |
12,211 |
|
|
$ |
12,368 |
|
Net inpatient revenues as a % of net operating revenues |
|
|
46.6 |
% |
|
|
46.8 |
% |
|
|
48.3 |
% |
Net outpatient revenues as a % of net operating revenues |
|
|
53.4 |
% |
|
|
53.2 |
% |
|
|
51.7 |
% |
Net (loss) income attributable to Community Health Systems, Inc. |
|
$ |
(133 |
) |
|
$ |
46 |
|
|
$ |
230 |
|
Net (loss) income attributable to Community Health Systems, Inc. |
|
|
(1.1 |
)% |
|
|
0.4 |
% |
|
|
1.9 |
% |
Adjusted EBITDA(8) |
|
$ |
1,453 |
|
|
$ |
1,466 |
|
|
$ |
1,969 |
|
Adjusted EBITDA as a % of net operating revenues(8) |
|
|
11.6 |
% |
|
|
12.0 |
% |
|
|
15.9 |
% |
|
|
|
|
|
|
|
|
|
|
|||
Liquidity Data |
|
|
|
|
|
|
|
|
|
|||
Net cash flows provided by (used in) operating activities |
|
$ |
210 |
|
|
$ |
300 |
|
|
$ |
(131 |
) |
Net cash flows provided by (used in) operating activities as a % of net |
|
|
1.7 |
% |
|
|
2.5 |
% |
|
|
(1.1 |
)% |
Net cash flows used in investing activities |
|
$ |
(26 |
) |
|
$ |
(259 |
) |
|
$ |
(524 |
) |
Net cash flows used in financing activities |
|
$ |
(264 |
) |
|
$ |
(430 |
) |
|
$ |
(514 |
) |
6
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
Increase (Decrease) |
|
|||
|
|
(Dollars in millions) |
|
|||||||||
Same-Store Data(9) |
|
|
|
|
|
|
|
|
|
|||
Admissions(3) |
|
|
413,529 |
|
|
|
399,355 |
|
|
|
3.5 |
% |
Adjusted admissions(4) |
|
|
942,074 |
|
|
|
894,388 |
|
|
|
5.3 |
% |
Patient days(5) |
|
|
1,864,128 |
|
|
|
1,895,988 |
|
|
|
|
|
Average length of stay (days)(6) |
|
|
4.5 |
|
|
|
4.7 |
|
|
|
|
|
Occupancy rate (beds in service)(7) |
|
|
49.9 |
% |
|
|
51.5 |
% |
|
|
|
|
Net operating revenues |
|
$ |
12,009 |
|
|
$ |
11,457 |
|
|
|
4.8 |
% |
Income from operations |
|
$ |
942 |
|
|
$ |
973 |
|
|
|
(3.2 |
)% |
Income from operations as a % of net operating revenues |
|
|
7.8 |
% |
|
|
8.5 |
% |
|
|
|
|
Depreciation and amortization |
|
$ |
485 |
|
|
$ |
491 |
|
|
|
|
|
Equity in earnings of unconsolidated affiliates |
|
$ |
(8 |
) |
|
$ |
(14 |
) |
|
|
|
|
7
Adjusted EBITDA is not a measurement of financial performance under U.S. GAAP. It should not be considered in isolation or as a substitute for net income, operating income, or any other performance measure calculated in accordance with U.S. GAAP. The items excluded from Adjusted EBITDA are significant components in understanding and evaluating financial performance. The Company believes such adjustments are appropriate as the magnitude and frequency of such items can vary significantly and are not related to the assessment of normal operating performance. Additionally, this calculation of Adjusted EBITDA may not be comparable to similarly titled measures disclosed by other companies.
The following table reflects the reconciliation of Adjusted EBITDA, as defined, to net (loss) income attributable to Community Health Systems, Inc. stockholders as derived directly from our Consolidated Financial Statements for the years ended December 31, 2023, 2022 and 2021 (in millions):
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Net (loss) income attributable to Community Health Systems, Inc. |
|
$ |
(133 |
) |
|
$ |
46 |
|
|
$ |
230 |
|
Adjustments: |
|
|
|
|
|
|
|
|
|
|||
Provision for income taxes |
|
|
191 |
|
|
|
170 |
|
|
|
131 |
|
Depreciation and amortization |
|
|
505 |
|
|
|
534 |
|
|
|
540 |
|
Net income attributable to noncontrolling interests |
|
|
149 |
|
|
|
133 |
|
|
|
138 |
|
Interest expense, net |
|
|
830 |
|
|
|
858 |
|
|
|
885 |
|
(Gain) loss from early extinguishment of debt |
|
|
(72 |
) |
|
|
(253 |
) |
|
|
79 |
|
Gain from CoreTrust Transaction |
|
|
— |
|
|
|
(119 |
) |
|
|
— |
|
Gain on sale of equity interests in Macon Healthcare, LLC |
|
|
— |
|
|
|
— |
|
|
|
(39 |
) |
Impairment and (gain) loss on sale of businesses, net |
|
|
(87 |
) |
|
|
71 |
|
|
|
24 |
|
Expense from government and other legal matters and |
|
|
36 |
|
|
|
5 |
|
|
|
— |
|
(Income) expense from the settlement of professional liability claims |
|
|
— |
|
|
|
— |
|
|
|
(19 |
) |
Expense related to employee termination benefits and other |
|
|
12 |
|
|
|
6 |
|
|
|
— |
|
Change in estimate for professional claims liability |
|
|
— |
|
|
|
15 |
|
|
|
— |
|
Expense from business transformation costs |
|
|
22 |
|
|
|
— |
|
|
|
— |
|
Adjusted EBITDA |
|
$ |
1,453 |
|
|
$ |
1,466 |
|
|
$ |
1,969 |
|
Sources of Revenue
The following table presents the approximate percentages of net operating revenues by payor source for the periods indicated. The data for the periods presented are not strictly comparable due to the effect that businesses acquired, sold, closed or opened during each of the respective periods, as applicable, have had on these statistics.
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Medicare |
|
|
19.9 |
% |
|
|
20.9 |
% |
|
|
21.4 |
% |
Medicare Managed Care |
|
|
16.8 |
|
|
|
16.1 |
|
|
|
15.1 |
|
Medicaid |
|
|
14.3 |
|
|
|
14.8 |
|
|
|
13.5 |
|
Managed Care and other third-party payors |
|
|
47.9 |
|
|
|
47.5 |
|
|
|
49.1 |
|
Self-pay |
|
|
1.1 |
|
|
|
0.7 |
|
|
|
0.9 |
|
Total |
|
|
100.0 |
% |
|
|
100.0 |
% |
|
|
100.0 |
% |
As shown above, we receive a substantial portion of our revenues from the Medicare, Medicare Managed Care and Medicaid programs. Included in Managed Care and other third-party payors is net operating revenues from insurance companies with which we
8
have insurance provider contracts, insurance companies for which we do not have insurance provider contracts, workers’ compensation carriers and non-patient service revenue, such as gain (loss) on investments, rental income and cafeteria sales. We generally expect the portion of revenues received from the Medicare, Medicare Managed Care and Medicaid programs to increase over the long-term due to the general aging of the population and other factors, including health reform initiatives. There has been a trend toward increased enrollment in Medicare Managed Care and Medicaid managed care programs, which may adversely affect our net operating revenues. We may also be impacted by regulatory requirements imposed on insurers, such as minimum medical-loss ratios and specific benefit requirements. Furthermore, in the normal course of business, managed care programs, insurance companies and employers actively negotiate the amounts paid to hospitals. Our relationships with payors may be impacted by price transparency initiatives and out-of-network billing restrictions, including those in the No Surprises Act. There can be no assurance that we will retain our existing reimbursement arrangements or that third-party payors will not attempt to further reduce the rates they pay for our services.
Net operating revenues include amounts estimated by management to be reimbursable by Medicare and Medicaid under prospective payment systems and provisions of cost-based reimbursement and other payment methods. In addition, we are reimbursed by non-governmental payors using a variety of payment methodologies. Amounts we receive for the treatment of patients covered by Medicare, Medicaid and non-governmental payors are generally less than our standard billing rates. We account for the differences between the estimated program reimbursement rates and our standard billing rates as contractual allowance adjustments, which we deduct from gross revenues to arrive at net operating revenues. Final settlements under some of these programs are subject to adjustment based on administrative review and audit by third parties. We account for adjustments to previous program reimbursement estimates as contractual allowance adjustments and report them in the periods that such adjustments become known. Contractual allowance adjustments related to final settlements and previous program reimbursement estimates impacted net operating revenues by an insignificant amount in each of the years ended December 31, 2023, 2022 and 2021.
The payment rates under the Medicare program for hospital inpatient and outpatient acute care services are based on prospective payment systems, which depend upon a patient’s diagnosis or the clinical complexity of services provided to a patient, among other factors. These rates are indexed for inflation annually, although increases have historically been less than actual inflation.
Payment rates under the Medicaid program vary by state. In addition to the base payment rates for specific claims for services rendered to Medicaid enrollees, several states utilize supplemental reimbursement programs to make separate payments that are not specifically tied to an individual’s care, some of which offset a portion of the cost of providing care to Medicaid and indigent patients. These programs are funded with a combination of state and federal resources, including, in certain instances, fees or taxes levied on the providers. The programs are generally authorized by CMS for a specified period of time and require CMS’s approval to be extended. We are unable to predict whether or on what terms CMS will extend the supplemental programs in the states in which we operate. Under these supplemental programs, we recognize revenue and related expenses in the period in which amounts are estimable and payment is reasonably assured. Reimbursement under these programs is reflected in net operating revenues and included as Medicaid revenue in the table above, and fees, taxes or other program related costs are reflected in other operating expenses.
As of December 31, 2023, Indiana, Alabama, Texas and Florida represented our only areas of significant geographic concentration. Net operating revenues generated by our hospitals in Indiana, as a percentage of consolidated net operating revenues, were 17.1% in 2023, 17.3% in 2022 and 16.4% in 2021. Net operating revenues generated by our hospitals in Alabama, as a percentage of consolidated net operating revenues, were 14.4% in 2023, 13.3% in 2022 and 13.0% in 2021. Net operating revenues generated by our hospitals in Texas, as a percentage of consolidated net operating revenues, were 11.7% in 2023, 11.7% in 2022 and 11.0% in 2021. Net operating revenues generated by our hospitals in Florida, as a percentage of consolidated net operating revenues, were 11.1% in 2023, 11.6% in 2022 and 12.2% in 2021.
Hospital revenues depend upon inpatient occupancy levels, the volume of outpatient procedures and the payment rates for hospital services provided, which are a function of amounts charged, rates negotiated with third-party payors and rates determined by government payors. Charges and payment rates for routine inpatient services vary significantly depending on the type of service performed and the geographic location of the hospital. In recent years, we have experienced a significant increase in revenue received from outpatient services. We attribute this increase to:
Healthcare facility operations are also subject to certain seasonal fluctuations, including decreases in patient utilization during holiday periods and increases in colder weather months. Variations in the prevalence and severity of outbreaks of illnesses, such as COVID-19, have also resulted in, and may continue to result in, similar fluctuations of our business.
9
Government Regulation
Overview. Participants in the healthcare industry are required to comply with extensive government regulation at the federal, state and local levels. If we fail to comply with applicable laws and regulations, we may be subject to criminal penalties and civil sanctions, our hospitals could lose their licenses and we could lose our ability to participate in Medicare, Medicaid and other government programs. These legal and regulatory standards address, among other issues, licensure, certification, and enrollment with government programs; the necessity and adequacy of medical care; quality of medical equipment and services; qualifications of medical and support personnel; operating policies and procedures; screening, stabilization and transfer of individuals who have emergency medical conditions; billing and coding for services; handling overpayments; classifications of levels of care provided; preparing and filing cost reports; relationships with referral sources and referral recipients; maintenance of adequate records; hospital use; rate-setting; building codes; environmental protection; privacy and security; interoperability and refraining from information blocking; debt collection; balance billing and billing for out-of-network services; and communications with patients and consumers.
Hospitals are subject to periodic inspection by federal, state and local authorities to determine their compliance with applicable regulations and requirements necessary for licensing and certification. All of our hospitals are licensed under appropriate state laws and are qualified to participate in Medicare and Medicaid programs. In addition, most of our hospitals are accredited by The Joint Commission. This accreditation indicates that a hospital satisfies the applicable health and administrative standards to participate in Medicare and Medicaid programs.
Government regulations are subject to change. If applicable laws and regulations change, we may have to make changes to our facilities, equipment, personnel and services so that our hospitals remain certified as hospitals and qualified to participate in these programs. We believe that our hospitals are in substantial compliance with current federal, state and local regulations and standards. We cannot be certain that governmental officials responsible for enforcing these laws or whistleblowers will not assert that we are in violation of them or that such statutes or regulations will be interpreted by the courts in a manner consistent with our interpretation.
Healthcare Reform, including Price Transparency. The healthcare industry is subject to changing political, regulatory, and economic influences that may affect our business. In recent years, the U.S. Congress and certain state legislatures have introduced and passed a large number of proposals and legislation affecting the healthcare system, including laws intended to impact access to health insurance and reduce healthcare costs and government spending. The most prominent of these efforts, the Affordable Care Act, affects how healthcare services are covered, delivered and reimbursed, and expanded health insurance coverage through a combination of public program expansion and private sector health insurance reforms. The Affordable Care Act has been, and continues to be, subject to legislative and regulatory changes and court challenges.
To increase access to health insurance during the COVID-19 pandemic, the American Rescue Plan Act of 2021, or the ARPA, enhanced subsidies for individuals eligible to purchase coverage through Affordable Care Act marketplaces. Subsequent legislation extended these enhanced subsidies through 2025. In addition, Medicaid enrollment increased as a result of COVID-19 relief legislation that authorized a temporary increase in federal funds for certain Medicaid expenditures in states that maintained continuous Medicaid enrollment, among other requirements. However, this “continuous coverage” requirement expired on April 1, 2023, which has led to Medicaid coverage disruptions and dis-enrollments of Medicaid enrollees. These and other changes and initiatives may impact the number of individuals that elect to obtain public or private health insurance or the scope of such coverage, if purchased.
Of critical importance to us is the potential impact of any changes specific to the Medicaid program, including the funding and expansion provisions of the Affordable Care Act and subsequent legislation or agency initiatives. Historically, the states with the greatest reductions in the number of uninsured adult residents have expanded Medicaid under the Affordable Care Act. A number of states have opted out of the Medicaid coverage expansion provisions, but could ultimately decide to expand their programs at a later date. Of the 15 states in which we operated hospitals as of December 31, 2023, nine states have expanded their Medicaid programs. At this time, the other six states have not, including Florida, Alabama, Tennessee, Mississippi and Texas, where we operated a significant number of hospitals as of December 31, 2023. Some states use, or have applied to use, waivers granted by CMS to implement expansion, impose different eligibility or enrollment conditions, or otherwise implement programs that vary from federal standards.
Other recent reform initiatives and proposals at the federal and state levels include those focused on price transparency and limiting out-of-network charges, which may impact prices, our competitive position and the relationships between hospitals, insurers, patients, and ancillary providers (such as anesthesiologists, radiologists, and pathologists). For example, the No Surprises Act imposes requirements on providers and health plans intended to prevent “surprise” medical bills. Among other restrictions and requirements, the law prohibits providers from charging patients an amount beyond the in-network cost sharing amount for services rendered by out-of-network providers, subject to limited exceptions. For services for which balance billing is prohibited (even when no balance billing occurs), the No Surprises Act may limit the amounts received by out-of-network providers from health plans and establishes an independent dispute resolution process for providers and payors to handle payment disputes that cannot be resolved through direct negotiations. The No Surprises Act also requires that providers provide a good faith estimate of expected charges to uninsured or self-pay patients for scheduled items and services, in advance of the date of the scheduled item or service or upon request. Based on these
10
estimates, such patients may invoke a patient-provider dispute resolution process to challenge charges in certain circumstances. The regulations and related guidance implementing the No Surprises Act, including those establishing the provider-payer dispute resolution process, have been and continue to be subject to legal challenges.
Other trends toward transparency and value-based purchasing may impact the competitive position and patient volumes of providers. For example, the CMS Care Compare website makes available to the public certain data that hospitals submit in connection with Medicare reimbursement claims, including hospital performance data on quality measures and patient satisfaction. In addition, Medicare reimbursement for hospitals is adjusted based on quality and efficiency measures, and CMS currently administers various accountable care organizations and bundled payment demonstration projects. The CMS Innovation Center has highlighted the need to accelerate the movement to value-based care and drive broader system transformation.
Fraud and Abuse Laws. Participation in the Medicare and Medicaid programs is heavily regulated by federal statute and regulation. If a hospital fails to comply substantially with the requirements for participating in the programs, the hospital’s participation may be terminated and/or civil or criminal penalties may be imposed. For example, a hospital may lose its ability to participate in the Medicare program if it engages in any of the following acts:
Any person or entity that knowingly and willfully defrauds or attempts to defraud a healthcare benefit program, including private healthcare plans, may be subject to fines, imprisonment or both. Additionally, any person or entity that knowingly and willfully falsifies or conceals a material fact or makes any material false or fraudulent statements in connection with the delivery or payment of healthcare services by a healthcare benefit plan is subject to a fine, imprisonment or both.
A section of the Social Security Act known as the “Anti-Kickback Statute” prohibits some business practices and relationships under Medicare, Medicaid and other federal healthcare programs. These practices include the payment, receipt, offer, or solicitation of remuneration of any kind in exchange for items or services that are reimbursed under a federal healthcare program. Courts have interpreted this statute broadly and have held that there is a violation of the Anti-Kickback Statute if just one purpose of the remuneration is to generate referrals.
The Office of Inspector General of the Department of Health and Human Services, or OIG, is responsible for identifying and investigating fraud and abuse activities in federal healthcare programs. As authorized by Congress, the OIG publishes regulations outlining activities and business relationships that would be deemed not to violate the Anti-Kickback Statute. These regulations are known as “safe harbor” regulations. The failure of a particular activity to comply with the safe harbor regulations does not necessarily mean that the activity violates the Anti-Kickback Statute; however, such failure may lead to increased scrutiny by government enforcement authorities.
The OIG also provides guidance to healthcare providers by identifying types of activities that could violate the Anti-Kickback Statute. The OIG has identified the following incentive arrangements as potential violations of the Anti-Kickback Statute:
11
We have a variety of financial relationships with physicians who refer patients to our hospitals. Physicians own interests in a number of our facilities. Physicians may also own our stock. We also have contracts with physicians providing for a variety of financial arrangements, including employment contracts, leases, management agreements and professional service agreements. We provide financial incentives to recruit physicians to relocate to communities served by our hospitals. These incentives include relocation, reimbursement for certain direct expenses, income guarantees and, in some cases, loans. Although we strive to comply with the Anti-Kickback Statute, taking into account available guidance including the “safe harbor” regulations, we cannot assure you that regulatory authorities will not determine otherwise. If that happens, we could be subject to criminal and civil penalties and/or exclusion from participating in Medicare, Medicaid or other government healthcare programs. Civil monetary penalties increase annually based on updates to the consumer price index.
The Social Security Act also includes a provision commonly known as the “Stark Law.” This law prohibits physicians from referring Medicare and Medicaid patients to healthcare entities in which they or any of their immediate family members have ownership interests or other financial arrangements. These types of referrals are commonly known as “self-referrals.” Sanctions for violating the Stark Law include denial of payment, civil monetary penalties that are increased annually based on updates to the consumer price index and exclusion from federal healthcare programs.
There are ownership and compensation arrangement exceptions to the self-referral prohibition. CMS has issued regulations that interpret these exceptions and other provisions of the Stark Law. One exception allows a physician to refer patients to a healthcare entity in which the physician has an ownership interest if the entity is located in a rural area, as defined in the statute. There are also exceptions for many of the customary financial arrangements between physicians and providers, including employment contracts, leases and recruitment agreements.
Another exception to the Stark Law, known as the “whole hospital” exception, allows a physician to make a referral to a hospital if the physician owns an interest in the entire hospital, as opposed to an ownership interest in a department of the hospital, and the hospital meets certain “grandfathering” requirements imposed by the Affordable Care Act. These requirements prohibit physicians from increasing the aggregate percentage of their ownership in the hospital and restrict the ability of physician-owned hospitals from expanding the capacity of their aggregate licensed beds, operating rooms and procedure rooms, beyond the ownership percentage and capacities in place in 2010. The whole hospital exception also contains additional public disclosure requirements. A hospital is considered to be physician-owned if any physician, or an immediate family member of a physician, holds debt, stock or other types of investment in the hospital or in any owner of the hospital, excluding physician ownership through publicly-traded securities that meet certain conditions.
In addition to the restrictions and disclosure requirements applicable to physician-owned hospitals under the Stark Law, CMS regulations require physician-owned hospitals and their physician owners to disclose certain ownership information to patients. Physician-owned hospitals must disclose their physician ownership in writing to patients and must make a list of their physician owners available upon request. Additionally, each physician owner who is a member of a physician-owned hospital’s medical staff must agree, as a condition of continued medical staff membership or admitting privileges, to disclose in writing to all patients whom they refer to the hospital their (or an immediate family member’s) ownership interest in the hospital. If a hospital fails to comply with these regulations, the hospital could lose its Medicare provider agreement and be unable to participate in Medicare.
Law enforcement authorities, including the OIG, the courts and Congress have in recent years increased scrutiny of arrangements between healthcare providers and potential referral sources to ensure that the arrangements are not designed as a mechanism to improperly pay for patient referrals and/or other business. Investigators have demonstrated a willingness to look behind the formalities of a business transaction to determine the underlying purpose of payments between healthcare providers and potential referral sources.
Many states in which we operate have also adopted laws that prohibit payments to physicians in exchange for referrals, similar to the federal Anti-Kickback Statute, or that otherwise prohibit fraud and abuse activities. Many states have also passed self-referral legislation similar to the Stark Law, prohibiting the referral of patients to entities with which the physician has a financial relationship. Often these state laws are broad in scope and may apply regardless of the source of payment for care. These statutes typically provide for criminal and civil penalties, as well as loss of licensure. Little precedent exists for the interpretation or enforcement of these state laws.
Our operations could be adversely affected by the failure of our arrangements to comply with the Anti-Kickback Statute, the Stark Law, billing laws and regulations, state fraud and abuse laws, evolving interpretations of current requirements or the adoption of new, federal or state laws or regulations. We are unable to predict whether other legislation or regulations at the federal or state level in any of these areas will be adopted, what form such legislation or regulations may take or how they may affect our operations. We are
12
continuing to enter into new financial arrangements with physicians and other providers in a manner structured to comply in all material respects with these laws. We strive to comply with applicable fraud and abuse laws. We cannot assure you, however, that governmental officials responsible for enforcing these laws or whistleblowers will not assert that we are in violation of them or that such statutes or regulations ultimately will be interpreted by the courts in a manner consistent with our interpretation.
Federal False Claims Act and Similar State Laws. Another significant enforcement mechanism used within the healthcare industry is the federal False Claims Act, or FCA, which can be used to prosecute Medicare and other government program fraud involving issues such as coding errors, billing for service not provided and submitting false cost reports. The FCA covers payments involving federal funds in connection with the health insurance exchanges created under the Affordable Care Act, if those payments involve any federal funds. Liability under the FCA often arises when an entity knowingly submits a false claim for reimbursement to the federal government. The FCA broadly defines the term “knowingly.” Although simple negligence will not give rise to liability under the FCA, submitting a claim with reckless disregard to its truth or falsity may constitute “knowingly” submitting a false claim and result in liability. Among the many other potential bases for liability under the FCA is the knowing and improper failure to report and refund amounts owed to the government within 60 days of identifying an overpayment. An overpayment is deemed to be identified when a person has, or should have through reasonable diligence, determined that an overpayment was received and quantified the overpayment. Submission of a claim for an item or service generated in violation of the Anti-Kickback Statute constitutes a false or fraudulent claim under the FCA. In some cases, whistleblowers, the federal government and courts have taken the position that providers who allegedly have violated other statutes, such as the Stark Law, have thereby submitted false claims under the FCA.
When a defendant is determined by a court of law to be liable under the FCA, the defendant must pay three times the actual damages sustained by the government, plus substantial civil penalties for each separate false claim. These civil monetary penalties are adjusted annually based on updates to the consumer price index. Settlements entered into prior to litigation usually involve a less severe calculation of damages. The FCA also contains “qui tam,” or whistleblower provisions, which allow private individuals to bring actions on behalf of the government alleging that the defendant has defrauded the federal government. If the government intervenes in the action and prevails, the party filing the initial complaint may share in any settlement or judgment. If the government does not intervene in the action, the whistleblower plaintiff may pursue the action independently and may receive a larger share of any settlement or judgment. When a private party brings a qui tam action under the FCA, the defendant generally will not be made aware of the lawsuit until the government commences its own investigation or determines whether it will intervene. Every entity that receives at least $5 million annually in Medicaid payments must have written policies for all employees, contractors and agents providing detailed information about false claims, false statements and whistleblower protections under certain federal laws, including the FCA, and similar state laws.
A number of states, including states in which we operate, have adopted their own false claims provisions as well as their own whistleblower provisions whereby a private party may file a civil lawsuit in state court. Federal law provides an incentive to states to enact false claims laws that are comparable to the FCA. From time to time, companies in the healthcare industry, including ours, may be subject to actions under the FCA or similar state laws.
Corporate Practice of Medicine; Fee-Splitting. Some states prohibit unlicensed persons or business entities, including corporations, from employing physicians or certain other health professionals. Some states also prohibit direct or indirect payments to, or entering into fee-splitting arrangements with, healthcare providers and unlicensed persons or business entities. Possible sanctions for violations of these restrictions include loss of a healthcare provider’s license, civil and criminal penalties and rescission of business arrangements. These laws vary from state to state, are often vague and have seldom been interpreted by the courts or regulatory agencies. We structure our arrangements with healthcare providers to comply with the relevant state law. However, we cannot provide assurance that governmental officials responsible for enforcing these laws will not assert that we, or transactions in which we are involved, are in violation of these laws. These laws may also be interpreted by the courts in a manner inconsistent with our interpretations.
Emergency Medical Treatment and Active Labor Act. The Emergency Medical Treatment and Active Labor Act, or EMTALA, imposes federal requirements as to the care that must be provided to anyone who comes to facilities providing emergency medical services seeking care before they may be transferred to another facility or otherwise denied care. Under this law, healthcare facilities are required to screen patients for emergency medical conditions and stabilize them where such conditions exist, regardless of an individual’s ability to pay for treatment. Sanctions for failing to fulfill these requirements include exclusion from participation in Medicare and Medicaid programs and civil money penalties, which are increased annually based on updates to the consumer price index. In addition, the law creates private civil remedies that enable an individual who suffers personal harm as a direct result of a violation of the law to sue the offending hospital for damages and equitable relief. A medical facility that suffers a financial loss as a direct result of another participating hospital’s violation of the law also has a similar right. Although we believe that our practices comply with the law, we can give no assurance that governmental officials responsible for enforcing the law will not assert we are in violation of this law or that interpretations of the law will not change. In particular, hospitals may face conflicting interpretations as to the requirements imposed by EMTALA as interpreted by HHS in relation to state laws that limit access to abortion or other reproductive health services. For example, CMS has provided guidance regarding EMTALA obligations specific to patients who are
13
pregnant or are experiencing pregnancy loss and the preemption of state law. This guidance is the subject of legal challenges, including pending cases in Texas and Ohio that have allowed state restrictions to remain in effect or stayed or have limited application of the guidance as the cases continue.
Conversion Legislation. Many states, including some where we have hospitals and others where we may in the future acquire hospitals, have adopted legislation regarding the sale or other disposition of hospitals operated by not-for-profit entities. In other states that do not have specific legislation, the attorneys general have demonstrated an interest in these transactions under their general obligations to protect charitable assets from waste. These legislative and administrative efforts primarily focus on the appropriate valuation of the assets divested and the use of the proceeds of the sale by the not-for-profit seller. While these reviews and, in some instances, approval processes can add additional time to the closing of a hospital acquisition, we have not had any significant difficulties or delays in completing the acquisition process. There can be no assurance, however, that future actions on the state level will not seriously delay or even prevent our ability to acquire hospitals. If these activities are widespread, they could limit our ability to acquire hospitals.
Antitrust Laws. The federal government and most states have enacted antitrust laws that prohibit certain types of conduct deemed to be anti-competitive. These laws prohibit price fixing, market allocation, bid-rigging, concerted refusal to deal, market monopolization, price discrimination, tying arrangements, acquisitions of competitors and other practices that have, or may have, an adverse effect on competition. Recently, some states have also passed legislation requiring for-profit healthcare entities, including hospitals, to notify the state attorneys general or other designated entities in advance of sales or other transactions. Violations of federal or state antitrust laws can result in various sanctions, including criminal and civil penalties. Antitrust enforcement in the healthcare industry is currently a priority of the Federal Trade Commission, or FTC, and the U.S. Department of Justice. We believe we are in compliance with such federal and state laws, but courts or regulatory authorities may reach a determination in the future that could adversely affect our operations.
Certificates of Need. The construction of new facilities, the acquisition of existing facilities, significant capital expenditures and the addition of new services at our facilities may be subject to state laws that require prior approval by state regulatory agencies. These certificate of need, or CON, laws generally require that a state agency determine the public need and give approval prior to the construction or acquisition of facilities, significant capital expenditure or the addition of new services. As of December 31, 2023, we operated 53 hospitals in 11 states that have adopted CON laws. If we fail to obtain necessary state approval, we will not be able to expand our facilities, complete acquisitions or significant capital expenditures or add new services in these states. Violation of these state laws may result in the imposition of civil sanctions or the revocation of a provider’s licenses.
HIPAA Administrative Simplification and Privacy, Security and Interoperability Requirements. The Health Insurance Portability and Accountability Act of 1996, or HIPAA, requires the use of uniform transaction standards for healthcare claims and payment transactions submitted or received electronically. These provisions are intended to encourage electronic commerce in the healthcare industry. HHS has established transaction standards and code sets that all healthcare providers must use when submitting or receiving certain healthcare transactions electronically and has issued operating rules to promote uniformity in the implementation of each standardized electronic transaction. HIPAA also requires that each provider use a National Provider Identifier.
As required by HIPAA, HHS has issued privacy and security regulations that extensively regulate the use and disclosure of protected health information, and require covered entities, including health plans and most healthcare providers, to implement administrative, physical and technical safeguards to protect the security of individually identifiable health information that is electronically maintained or transmitted. Business associates (entities that handle protected health information on behalf of covered entities) are subject to direct liability for violation of applicable provisions of the regulations. In addition, a covered entity may be subject to penalties as a result of a business associate violating HIPAA, if the business associate is found to be an agent of the covered entity.
Covered entities must report breaches of unsecured protected health information to affected individuals without unreasonable delay, but not to exceed 60 days of discovery of the breach by the covered entity or its agents. Notification must also be made to HHS and, in certain situations involving large breaches, to the media. HHS is required to publish on its website a list of all covered entities that report a breach involving more than 500 individuals. All non-permitted uses or disclosures of unsecured protected health information are presumed to be breaches unless the covered entity or business associate establishes that there is a low probability the information has been compromised. Various state laws and regulations may also require us to notify affected individuals in the event of a data breach involving individually identifiable information.
Violations of the HIPAA privacy and security regulations may result in criminal penalties and in substantial civil penalties per violation. The civil penalties are adjusted annually based on updates to the consumer price index. HHS is required to perform compliance audits. In addition to enforcement by HHS, state attorneys general are authorized to bring civil actions seeking either injunction or damages in response to violations of HIPAA privacy and security regulations that threaten the privacy of state residents. HHS may resolve HIPAA violations through informal means, such as allowing a covered entity to implement a corrective action plan,
14
but HHS has the discretion to move directly to impose monetary penalties and is required to impose penalties for violations resulting from willful neglect. We are also subject to any federal or state privacy-related laws that are more restrictive than the privacy regulations issued under HIPAA or that apply to other types of information. These laws vary and could impose additional penalties and subject us to additional privacy and security restrictions. For example, the FTC uses its consumer protection authority to initiate enforcement actions in response to data breaches. In addition, various states have enacted, and other states are considering, laws and regulations concerning the privacy and security of consumer and other personal information. To the extent we are subject to such requirements, these laws and regulations often have far-reaching effects, are subject to amendments and changing requirements and updates to regulators’ enforcement priorities, may require us to modify our data processing practices and policies, and may subject our business to a risk of increased potential liability. These laws and regulations often provide for civil penalties for violations, as well as a private right of action for data breaches, which may increase the likelihood or impact of data breach litigation. We have developed and utilize an information privacy and security compliance plan as part of our effort to comply with HIPAA and other federal and state privacy and security requirements. The privacy regulations and security laws and regulations have imposed, and will continue to impose, significant costs on us in order to comply with these standards.
Healthcare providers and industry participants are also subject to an increasing number of requirements intended to promote the interoperability and exchange of patient health information. For example, healthcare providers and certain other entities are subject to information blocking restrictions pursuant to the 21st Century Cures Act that prohibit practices that are likely to interfere with the access, exchange or use of electronic health information, except as required by law or specified by HHS as a reasonable and necessary activity. Violations may result in penalties or other significant disincentives. In November 2023, HHS issued a proposed rule to establish disincentives for certain types of providers. If finalized, hospitals found to have committed information blocking would not qualify as “meaningful electronic health record users” under the Medicare Promoting Interoperability Program and as a result would lose 75% of the annual market basket increase they would otherwise receive.
Payment
Medicare. Medicare is a federal health insurance program that provides certain hospital and medical insurance benefits to persons age 65 and over, some disabled persons, persons with end-stage renal disease and persons with amyotrophic lateral sclerosis, also known as ALS or Lou Gehrig’s Disease.
Payments for inpatient acute hospital services are generally made pursuant to a prospective payment system, or PPS. Under the inpatient PPS, our hospitals are paid a predetermined amount for each hospital discharge based on the patient’s diagnosis. Specifically, each discharge is assigned to a Medicare severity diagnosis-related group, commonly known as an “MS-DRG,” based upon the patient’s condition and treatment during the relevant inpatient stay. The MS-DRGs are severity-adjusted to account for the severity of each patient’s condition and expected resource consumption. Each MS-DRG has a payment weight assigned to it that is based on the average resources used to treat Medicare patients in that MS-DRG. MS-DRG payments are based on national averages and not on charges or costs specific to a hospital. Medicare sets discharge base rates (standardization payment amounts), which are adjusted according to the MS-DRG relative weights and geographic factors. In addition, hospitals may qualify for an “outlier” payment when a patient’s treatment costs are extraordinarily high and exceed a specified regulatory threshold.
The MS-DRG payment rates for inpatient acute services are adjusted by an update factor on October 1 of each year, the beginning of the federal fiscal year. The index used to adjust the MS-DRG payment rates, known as the “market basket index,” gives consideration to the inflation experienced by hospitals in purchasing goods and services. MS-DRG payment rates were increased by the “market basket index” update of 4.1% and 3.3% for each of federal fiscal years 2023 and 2024, respectively, subject to certain adjustments. For federal fiscal year 2023, the market basket update was adjusted by the following percentage points: a positive 0.5 percentage point adjustment in accordance with the Medicare Access and CHIP Reauthorization Act of 2015, or MACRA, and a 0.3 percentage point reduction for the productivity adjustment. For federal fiscal year 2024, the market basket update was reduced by 0.2 percentage points for the productivity adjustment. A reduction of 25% of the market basket update occurs if patient quality data is not submitted, and a reduction of 75% of the market basket update occurs for hospitals that fail to demonstrate meaningful use of certified electronic health records, or EHR, technology without receiving a hardship exception. Additional adjustments may apply, depending on patient-specific or hospital-specific factors.
The MS-DRG payment rates are also adjusted to promote value-based purchasing, linking payments to quality and efficiency. First, hospitals that meet or exceed certain quality performance standards receive greater reimbursement under CMS’s Hospital Value-Based Purchasing Program, while hospitals that do not satisfy certain quality performance standards receive reduced Medicare inpatient hospital payments. CMS withholds 2% of participating hospitals’ Medicare payments and uses the total amount collected to fund payments that reward hospitals based on a set of quality and resource use measures. CMS scores each hospital on its achievement relative to other hospitals and improvement relative to that hospital’s own past performance. Second, hospitals experiencing “excess readmissions” within 30 days from the patient’s date of discharge following treatment for designated conditions or procedures during a prior performance review period receive reduced payments for all inpatient discharges in the fiscal year, not just discharges relating to the conditions or procedures subject to the readmission standard. The payment reduction, which can be up to 3% of a hospital’s
15
base payments, is determined by assessing that hospital’s readmissions relative to hospitals with similar proportions of dual-eligible patients. Third, the bottom quartile of hospitals based on the national risk-adjusted hospital acquired condition, or HAC, rates in the previous year have their total inpatient operating Medicare payments reduced by 1%. Moreover, Medicare does not reimburse for care related to certain HACs. For cases in which a designated HAC was not present on admission, CMS does not allow the discharge to be assigned to a higher-paying MS-DRG based on the HAC, and the case is paid as though the secondary diagnosis (HAC) was not present.
In addition, hospitals may qualify for Medicare disproportionate share hospital, or DSH, payment adjustments when their percentage of low-income patients exceeds specified regulatory thresholds. A majority of our hospitals qualify to receive these adjustments. The methodology for calculating DSH payment adjustments is affected by shifts in CMS payment policy. For example, in August 2023, CMS changed the DSH formula by altering how days of care provided to patients who are eligible for benefits from Section 1115 Demonstrations are included in the Medicaid fraction and by excluding from the Medicaid fraction days of care of patients for which hospitals are paid from demonstration-authorized uncompensated or undercompensated care pools. This change will effectively decrease DSH payments for many hospitals. CMS also distributes an additional payment to each DSH hospital for its proportion of uncompensated care costs relative to the uncompensated care amount of other DSH hospitals. The uncompensated care amount is hospital-specific and generally includes charity care and non-Medicare and non-reimbursable Medicare bad debt. The Medicare DSH adjustments and uncompensated care payments as a percentage of net operating revenues were 0.75% and 0.88% for the years ended December 31, 2023 and 2022, respectively.
We also receive Medicare reimbursement for hospital outpatient services through a PPS. Services paid under the hospital outpatient PPS are grouped into ambulatory payment classifications, or APCs. Services for each APC are similar clinically and in terms of the resources they require. APC payment rates are generally determined by applying a conversion factor, which CMS updates annually using a market basket. For calendar year 2023, CMS estimated an increase in hospital outpatient PPS payments of 3.8%. This reflected a market basket increase of 4.1%, with a negative 0.3 percentage point productivity adjustment. For calendar year 2024, CMS estimated an increase in hospital outpatient PPS payments of 3.1%, reflecting a market basket increase of 3.3%, with a negative 0.2 percentage point productivity adjustment. A 2.0 percentage point reduction to the market basket update applies to hospitals that do not submit required patient quality data.
The Medicare reimbursement for outpatient services may also be affected by broad shifts in payment policy. For example, recent changes related to the 340B Drug Pricing Program have implications for all hospitals reimbursed under the outpatient PPS, including those, like ours, that do not participate in the program. The 340B program allows non-profit healthcare organizations to purchase certain outpatient drugs from pharmaceutical manufacturers at discounted rates. In 2018, CMS implemented a payment policy that reduced Medicare payments for 340B hospitals for most drugs obtained at 340B-discounted rates and that resulted in increased payments for non-340B hospitals. In June 2022, the U.S. Supreme Court invalidated past payment cuts for hospitals participating in the 340B Drug Pricing Program. In light of the U.S. Supreme Court decision and to achieve budget neutrality, CMS implemented a reduction of approximately 3.1% to payment rates for non-drug services under the outpatient PPS for calendar year 2023. HHS directed that $9 billion be paid to affected 340B providers in one-time lump sum payments as the remedy for calendar years 2018 through 2022. In order to comply with budget neutrality requirements, HHS finalized a corresponding offset in future non-drug item and service payments for all outpatient PPS providers (except new providers) that will reduce the outpatient PPS conversion factor by 0.5% annually. This adjustment will start in calendar year 2026 and continue for approximately 16 years.
CMS has implemented an expanded site-neutral payment policy for off-campus provider-based departments paid under the outpatient PPS. Under the policy, all off-campus provider-based departments are paid the Medicare Physician Fee Schedule, or MPFS, -equivalent rate for clinic visits, which is generally substantially lower than the outpatient PPS rate. The MPFS-equivalent rate for calendar year 2024 is approximately 40% of the outpatient PPS rate.
CMS uses fee schedules to pay for physician services, physical, occupational and speech therapies, durable medical equipment, clinical diagnostic laboratory services, freestanding surgery center services, and certain other items and services. Under the MPFS, CMS has assigned a national relative value unit, or RVU, to most medical procedures and services that reflects the resources required to provide the services relative to all other services. Each RVU is calculated based on a combination of the time and intensity of work required, overhead expense attributable to the service, and professional liability insurance expense. These elements are each modified by a geographic adjustment factor to account for local practice costs and are then aggregated. To determine the payment rate for a particular service, the sum of the geographically adjusted RVUs is multiplied by a conversion factor. For calendar year 2024, CMS decreased the conversion factor by approximately 3.4%.
CMS requires physicians and certain other healthcare clinicians to participate in one of two tracks under the Quality Payment Program, or QPP, which is a payment methodology intended to reward high-quality patient care. Under both tracks, performance data collected each performance year affects Medicare payments two years later. CMS expects to transition increasing financial risk to providers as QPP evolves. The Advanced Alternative Payment Model, or Advanced APM, encourages participation in specific innovative payment models approved by CMS through financial incentives. For performance year 2023 and years prior, providers
16
were able to earn Medicare incentive payments. Beginning in the 2024 performance year, qualifying providers will instead receive positive adjustments to their MPFS payment rates (performance year 2024 determines adjustments in payment year 2026). In addition, providers are exempt from the reporting requirements and payment adjustments imposed under the Merit-Based Incentive Payment System, or MIPS, if the provider has sufficient participation in an Advanced APM. Alternatively, providers may participate in the MIPS track, under which physicians receive performance-based payment incentives or payment reductions based on their performance with respect to clinical quality, resource use, clinical improvement activities, and meeting Promoting Interoperability standards related to the meaningful use of EHRs.
In addition to the Medicare reimbursement reductions and adjustment discussed above, the Budget Control Act of 2011, or BCA, requires automatic spending reductions to reduce the federal deficit, resulting in a uniform percentage reduction across all Medicare programs of 2% per fiscal year that extends through the first seven months of 2032. These reductions apply to certain other federally funded healthcare programs, including TRICARE. As a result of the ARPA, an additional Medicare payment reduction of up to 4% was required to take effect in January 2022, although Congress has delayed implementation of this reduction until 2025. We anticipate that the federal deficit will continue to place pressure on government healthcare programs, and it is possible that future deficit reduction legislation will impose additional spending reductions.
Medicaid. Medicaid is a program funded jointly by state and federal governments, and administered by the states, that provides hospital and medical benefits to qualifying low-income individuals. Medicaid enrollment increased as a result of COVID-19 relief legislation that authorized a temporary increase in federal funds for certain Medicaid expenditures in states that maintained continuous Medicaid enrollment, among other requirements. The end of the continuous enrollment condition in 2023, including the resumption of redeterminations for Medicaid enrollees, has resulted in significant coverage disruptions and dis-enrollments of enrollees, and Medicaid enrollment is generally expected to decline through fiscal year 2024 (which ends June 30, 2024, in most states).
Most state Medicaid payments are made under a PPS or under programs that negotiate payment levels with individual hospitals. In addition to the base payment rates for specific claims for services rendered to Medicaid enrollees, states utilize supplemental reimbursement programs to make separate payments that are not specifically tied to an individual’s care. Supplemental payments may be in the form of Medicaid DSH payments, which are intended to offset hospitals’ uncompensated care costs. Medicaid DSH payments as a percentage of our net operating revenues were 0.21% and 0.39% for the years ended December 31, 2023 and 2022, respectively. The Affordable Care Act and subsequent legislation provide for reductions to the Medicaid DSH program, but Congress has delayed the implementation of these reductions. Under current law, Medicaid DSH payments will be reduced by $8.0 billion for the period from March 9, 2024 through September 30, 2024 and per year in each of federal fiscal years 2025 through 2027. Supplemental payments may also be in the form of non-DSH payments, such as upper payment limit payments, which are intended to address the difference between Medicaid fee-for-service payments and Medicare reimbursement rates, and payments under other programs that vary by state under Section 1115 waivers. These supplemental reimbursement programs are generally authorized by CMS for a specified period of time and require CMS’s approval to be extended. CMS is considering changes to both types of programs, and we are unable to predict whether or on what terms CMS will extend the supplemental programs in the states in which we operate.
The federal government and many states are using or considering various strategies to reduce Medicaid expenditures, outside of the pandemic response. In response to budgetary pressures, certain states in which we operate have adopted broad taxes on healthcare providers to fund the non-federal share of Medicaid programs. In addition, many states currently operate, or have applied to CMS to operate, Medicaid programs under waivers to standard Medicaid program requirements.
In recent years, aspects of existing or proposed Medicaid waiver programs have been subject to legal challenge, resulting in uncertainty. The prior presidential administration increased state flexibility in the administration of Medicaid programs, including by allowing states to condition enrollment on work or other community engagement or to use a block grant funding structure. However, the current presidential administration has implemented policies intended to strengthen Medicaid programs. For example, it has rescinded approvals of waivers for work and community engagement requirements, which have also been rejected by several courts, and is reexamining block grant funding structures. However, a federal court permitted Georgia to impose work and community engagement requirements under a Medicaid demonstration program that launched in mid-2023.
TRICARE. TRICARE is the Department of Defense’s healthcare program for active duty service members of the armed forces and others, including certain family members, retirees, and survivors. For inpatient services, TRICARE generally reimburses hospitals based on a DRG system modeled on the Medicare inpatient PPS. For outpatient services, TRICARE reimburses hospitals based on a PPS that is similar to that utilized for services furnished to Medicare beneficiaries.
Annual Cost Reports. Hospitals participating in the Medicare and some Medicaid programs, whether paid on a reasonable cost basis or under a PPS, are required to meet specified financial reporting requirements. Federal and, where applicable, state regulations require submission of annual cost reports identifying medical costs and expenses associated with the services provided by each hospital to Medicare beneficiaries and Medicaid recipients.
17
Annual cost reports required under the Medicare and some Medicaid programs are subject to routine governmental audits. These audits may result in adjustments to the amounts ultimately determined to be due to us under these reimbursement programs. Finalization of these audits often takes several years. Providers can appeal any final determination made in connection with an audit.
Medicare and Medicaid Managed Care. Under the Managed Medicare program, also known as Medicare Part C, or Medicare Advantage, the federal government contracts with private health plans to provide members with Medicare benefits. The plans may choose to offer supplemental benefits and impose higher premiums and cost-sharing obligations. Similarly, managed Medicaid programs enable states to contract with private entities to handle program responsibilities like care management and claims adjudication. Enrollment in Managed Medicare and managed Medicaid programs has increased in recent years as the federal and state governments seek to control healthcare costs.
Medicare Administrative Contractors. CMS competitively bids the Medicare fiscal intermediary and Medicare carrier functions to Medicare Administrative Contractors, or MACs, in 12 jurisdictions. Each MAC is geographically assigned and serves both Part A and Part B providers within a given jurisdiction. Chain providers had the option of having all hospitals use one home office MAC, and we chose to do so. CMS periodically re-solicits bids, and the MAC servicing a geographic area can change as a result of the bid competition. MAC transition periods can impact claims processing functions and the resulting cash flow.
Medicare and Medicaid Integrity. CMS contracts with third parties to promote the integrity of the Medicare program through review of quality concerns and detection of improper payments. Quality Improvement Organizations, or QIOs, for example, are groups of physicians and other healthcare quality experts that work on behalf of CMS to ensure that Medicare pays only for goods and services that are reasonable and necessary and that are provided in the most appropriate setting. Under the Recovery Audit Contractor, or RAC, program, CMS contracts with RACs nationwide to conduct post-payment reviews to detect and correct improper payments in the Medicare program, as required by statute. RACs review claims submitted to Medicare for billing compliance, including correct coding and medical necessity. Compensation for RACs is on a contingency basis and based upon the amount of overpayments and underpayments identified, if any. CMS limits the number of claims that RACs may audit by limiting the number of records that RACs may request from hospitals based on each provider’s claim denial rate for the previous year.
The RAC program’s scope also includes Medicaid claims. States may coordinate with Medicaid RACs regarding recoupment of overpayments and refer suspected fraud and abuse to appropriate law enforcement agencies. Medicaid RAC programs vary by state in design and operation. Under the Medicaid Integrity Program, CMS contracts with Unified Program Integrity Contractors, or UPICs, to perform audits, investigations and other integrity activities. Working across five geographic jurisdictions, UPICs collaborate with states and coordinate provider investigations across the Medicare and Medicaid programs.
We maintain policies and procedures to respond to the RAC requests and payment denials. Payment recoveries resulting from RAC reviews and denials are appealable, and we pursue reversal of adverse determinations at appropriate appeal levels. In recent years, there have been significant delays in the Medicare appeals process. However, HHS has taken steps to streamline the appeals process and, as of March 2023, it had nearly eliminated the backlog. Nevertheless, we may experience significant delays in appealing any RAC payment denials. Depending upon the growth of RAC programs and our success in appealing claims in future periods, our cash flows and results of operations could be negatively impacted.
Accountable Care Organizations. Accountable Care Organizations, or ACOs, have gained traction in both the public and private sectors. An ACO is a network of providers and suppliers (including hospitals, physicians and other designated professionals) that work together to invest in infrastructure and redesign delivery processes to achieve high quality and efficient delivery of services. ACOs are intended to produce savings as a result of improved quality and operational efficiency. For example, the Medicare Shared Savings Program seeks to promote accountability and coordination of care for Medicare fee-for-service beneficiaries through the creation of ACOs. Medicare-approved ACOs that achieve quality performance standards established by HHS are eligible to share in a portion of the amounts saved by the Medicare program. HHS has significant discretion to determine key elements of Medicare ACO programs. Certain waivers and exceptions are available from fraud and abuse laws for ACOs.
The Center for Medicare and Medicaid Innovation, or CMS Innovation Center, is responsible for establishing demonstration projects and other initiatives in order to identify, develop, test and encourage the adoption of new methods of delivering and paying for healthcare that create savings under the Medicare and Medicaid programs, while maintaining or improving quality of care. In a strategic report issued in 2021 and updated in 2022, the CMS Innovation Center highlighted the need to accelerate the movement to value-based care and drive broader system transformation. By 2030, the CMS Innovation Center aims to have all fee-for-service Medicare beneficiaries and most Medicaid beneficiaries in a care relationship with accountability for quality and total cost of care. CMS also indicated it will streamline its payment model portfolio and consider how to ensure broad provider participation.
18
Bundled Payment Initiatives. Providers participating in bundled payment initiatives accept accountability for costs and quality of care by agreeing to receive one payment for services provided to Medicare patients for certain medical conditions or episodes of care. By rewarding providers for increasing quality and reducing costs and penalizing providers if costs exceed a certain amount, bundled payment models are intended to lead to higher quality, more coordinated care at a lower cost to the Medicare program. The CMS Innovation Center has implemented bundled payment models, including the Bundled Payment for Care Improvement Advanced, or BPCI Advanced, initiative, which is expected to run through December 2025. Generally, participation in bundled payment programs is voluntary, but CMS currently requires hospitals in selected markets to participate in bundled payment initiatives for specific orthopedic procedures and end-stage renal disease treatment. A mandatory radiation oncology bundled payment model was expected to begin January 1, 2023, but CMS has delayed its implementation until a future date to be determined by the agency. CMS has indicated that it will provide six months’ notice before starting the model. In its 2021 strategy refresh, the CMS Innovation Center signaled its intent to increase provider participation through implementation of more mandatory models. We expect value-based purchasing programs, including models that condition reimbursement on patient outcome measures, to become more common with both governmental and non-governmental payors.
Commercial Insurance and Managed Care Companies. Our hospitals provide services to individuals covered by private healthcare insurance or by health plans administered by managed care companies. These payors pay our hospitals or in some cases reimburse their policyholders based upon the hospital’s established charges and the coverage provided in the insurance policy. Payors try to limit their costs by negotiating with hospitals and other healthcare providers for discounts to established charges. Commercial insurers and managed care companies also seek to reduce payments to hospitals by establishing payment rules that in effect re-characterize the services ordered by physicians. For example, some payors vigorously review each patient’s length of stay in the hospital and re-characterize as outpatient all inpatient stays of less than a particular duration (e.g., 24 hours). Similarly, some payors have prior authorization requirements designed to shift certain procedures to outpatient settings, where payment rates are typically lower. Reductions in payments for services provided by our hospitals to individuals covered by these payors could adversely affect us.
Supply Contracts
We purchase items, primarily medical supplies, medical equipment and pharmaceuticals, under an agreement with HealthTrust, a GPO in which we are a noncontrolling partner. The current term of this agreement expires in December 2024, with automatic renewal terms of one year unless either party terminates by giving notice of non-renewal. As of December 31, 2023, we had a 12.6% ownership interest in HealthTrust. By participating in this organization, we are able to procure items at competitively priced rates for our hospitals. There can be no assurance that our arrangement with HealthTrust will continue to provide the discounts that we have historically received.
Competition
The hospital industry is highly competitive. The competition among hospitals and other healthcare providers, including urgent care centers and other outpatient providers, for patients has intensified with the implementation of price transparency initiatives and as patients have become more conscious of rising costs and quality of care in their healthcare decision-making process. The majority of our hospitals are located in generally larger non-urban service areas in which we believe we are the primary, if not the sole, provider of general acute care health services. Those hospitals in non-urban service areas may face limited or no direct competition because there are no other hospitals in their primary service areas. However, these hospitals face competition from hospitals outside of their primary service area, including hospitals in urban areas that provide more complex services. Patients in those service areas may travel to these other hospitals for a variety of reasons, including the need for services we do not offer, payor networks that exclude our providers or physician referrals. Patients who are required to seek services from these other hospitals may subsequently shift their preferences to those hospitals for services we do provide. Our other hospitals, in selected urban service areas, may face competition from hospitals that are more established than our hospitals. Some of our competitors offer services, including extensive medical research and medical education programs, that are not offered by our facilities. In addition, in certain markets where we operate, large teaching hospitals provide highly specialized facilities, equipment and services that may not be available at our hospitals. We also face competition from other specialized care providers, including outpatient surgery, orthopedic, oncology and diagnostic centers. Some competitors are implementing physician alignment strategies, such as employing physicians, acquiring physician practice groups, and participating in ACOs or other clinical integration models. Cost-reduction strategies by large employer groups and their affiliates may increase this competition. We believe that we will continue to face increased competition in outpatient service models that become more integrated through acquisitions or partnerships between physicians, specialized care providers, and managed care payors.
In most markets in which we are not the sole provider of general acute care health services, our primary competitor is a municipal or not-for-profit hospital. These hospitals are owned by tax-supported governmental agencies or not-for-profit entities supported by endowments and charitable contributions. These hospitals are exempt from sales, property and income taxes. Such exemptions and support are not available to our hospitals and may provide the tax-supported or not-for-profit entities an advantage in funding general and capital expenditures and offering services more specialized than those available at our hospitals.
19
The number and quality of the physicians on a hospital’s staff is an important factor in a hospital’s competitive position. Physicians decide whether a patient is admitted to the hospital and the procedures to be performed. Admitting physicians may be on the medical staffs of other hospitals in addition to those of our hospitals. We attempt to attract our physicians’ patients to our hospitals by offering quality services and facilities, convenient locations and state-of-the-art equipment.
Trends towards transparency and value-based purchasing may impact our competitive position, ability to obtain or maintain favorable contract terms and patient volumes. CMS publicizes on its Care Compare website data that hospitals submit in connection with Medicare reimbursement claims, including performance data related to quality measures and patient satisfaction surveys. The quality measures that must be reported by providers, some of which impact reimbursement under value-based purchasing initiatives, continue to evolve. In addition, hospitals are required to publish online a list of their standard charges for all items and services, including gross charges, discounted cash prices and payor-specific and de-identified negotiated charges, in a machine-readable, publicly accessible online file. Hospitals are also required to publish a consumer-friendly list of standard charges for certain “shoppable” services (i.e., services that can be scheduled by a patient in advance) and any associated ancillary services or, alternatively, maintain an online price estimator tool. Further, CMS requires most health insurers to publish online charges negotiated with providers for healthcare services. Starting January 1, 2024, most health insurers must also provide online price comparison tools to help individuals get personalized cost estimates for all covered items and services. In addition, the No Surprises Act requires providers to send to an insured patient’s health plan a good faith estimate of the expected charges for scheduled items or services, including billing and diagnostic codes, prior to the scheduled date of the items or services. The estimate must cover any item or service that is reasonably expected to be provided together with the primary items or services, including those that may be provided by other providers. For uninsured or self-pay patients, providers must provide a good faith estimate of expected charges for scheduled items or services, in advance of the date of the scheduled item or service or upon request of the individual. If the actual charges to an uninsured or self-pay patient exceed the estimate by an amount determined by regulation to be substantial (currently $400), the patient may invoke a patient-provider dispute resolution process established by regulation to challenge the higher amount. HHS is deferring enforcement of portions of the good faith estimate requirements until it issues additional regulations.
Compliance Program
We take an operations team approach to compliance and utilize corporate experts for program design efforts and facility leaders for employee-level implementation. We believe compliance is another area that demonstrates our utilization of standardization and centralization techniques and initiatives, which yield efficiencies and consistency throughout our facilities. We recognize that our compliance with applicable laws and regulations depends on individual employee actions as well as company operations. Our approach focuses on integrating compliance responsibilities with operational functions. This approach is intended to reinforce our company-wide commitment to operate strictly in accordance with the laws and regulations that govern our business.
Our company-wide compliance program has been in place since 1997. Currently, the program’s elements include leadership, management and oversight at the highest levels, a Code of Conduct, risk area specific policies and procedures, employee education and training, an internal system for reporting concerns, auditing and monitoring programs and a means for enforcing the program’s policies.
The compliance program continues to be expanded and developed to meet the industry’s expectations and our needs. Specific written policies, procedures, training and educational materials and programs, as well as auditing and monitoring activities, have been prepared and implemented to address the functional and operational aspects of our business. Included within these functional areas are materials and activities for business sub-units, including laboratory, radiology, pharmacy, emergency, surgery, observation, home care, skilled nursing and clinics. Specific areas identified through regulatory interpretation and enforcement activities have also been addressed in our program. Claims preparation and submission, including coding, billing and cost reports, comprise the bulk of these areas. Financial arrangements with physicians and other referral sources, including compliance with the federal Anti-Kickback Statute and the Stark Law, emergency department treatment and transfer requirements and other patient disposition issues, are also the focus of policy and training, standardized documentation requirements and review and audit. Another focus of the program is the interpretation and implementation of the HIPAA standards for privacy and security.
We have a Code of Conduct, which applies to all directors, officers, employees and consultants, and a confidential disclosure program to enhance the statement of ethical responsibility expected of our employees and business associates who work in the accounting, financial reporting and asset management areas of our Company. Our Code of Conduct is posted on our website at www.chs.net/company-overview/code-of-conduct.
20
Human Capital
Overview
At December 31, 2023, we had approximately 61,000 employees, including approximately 13,000 part-time employees. References herein to “employees” refer to employees of our affiliates. We are subject to various state and federal laws that regulate wages, hours, benefits and other terms and conditions relating to employment. At December 31, 2023, certain employees at three of our hospitals are represented by various labor unions. It is possible that union organizing efforts will take place at additional hospitals in the future. We consider our employee relations to be good and have not experienced work stoppages that have materially, adversely affected our business or results of operations.
Our industry has been facing unprecedented workforce challenges, which have given rise to significant operating issues for healthcare providers. To address this challenge, we have implemented several initiatives to improve retention, recruiting, compensation programs and productivity. An area that has been particularly challenging for providers is registered nurse, or RN, recruitment and retention. We had a centralized clinical recruiting function in place for a limited number of our markets beginning in 2018 which has now been expanded to cover all of our health systems. Our team of recruiters and sourcers began focusing primarily on bedside nursing roles, but they also recruit for licensed practical nurse, case management, and director level positions. Given the success we have had with recruitment of these roles, we have expanded the function to also cover difficult-to-fill allied health positions. Since we have implemented our centralized recruiting function, we have seen an increase in clinical position hires and a decreased time-to-fill for these key patient care roles, which has decreased our level of reliance on higher cost contract labor. In addition to these efforts, we have been working to bring international RNs through the visa process to our hospitals. We have significantly expanded this effort by working with various outside firms specializing in international recruitment, and we are also offering a direct-to-hire model. We believe that these efforts will aid in our ability to take patient transfer requests, shorten emergency department wait times and lessen dependency on high cost contract labor. Finally, we have expanded our hospital-based nursing programs through our partnership with Jersey College and have eight campuses open in six states. Partnerships with other local nursing programs have also been strengthened across the enterprise to expand clinical faculty and increase enrollment.
Due to the challenges noted above and other factors, our hospitals and other healthcare facilities, like many other healthcare providers, have experienced increased labor costs. We may be required to continue to enhance wages and benefits to recruit and retain nurses and other medical support personnel or to hire more expensive temporary or contract personnel. We also depend on the available labor pool of semi-skilled and unskilled employees in each of the markets in which we operate. In some of our markets, employers across various industries have increased their wages for these roles, which has created more competition for this sector of employees. As a result of these and other factors, our labor costs could continue to increase. Moreover, potential changes to federal labor laws and regulations, including those supported by the current presidential administration, could increase the likelihood of employee unionization activity and the ability of employees to unionize. The extent of unionization may affect labor costs in the future. In addition, the states in which we operate could adopt mandatory nurse-staffing ratios or could revise mandatory nurse-staffing ratios already in place. State-mandated nurse-staffing ratios or other measures to regulate staffing could significantly affect labor costs and have an adverse impact on revenues if we are required to limit patient admissions in order to comply with such requirements.
Our hospitals are staffed by licensed physicians, including both employed physicians and physicians who are not employees of our hospitals. Some physicians provide services in our hospitals under contracts, which generally describe a term of service, provide and establish the duties and obligations of such physicians, require the maintenance of certain performance criteria and fix compensation for such services. Any licensed physician may apply to be accepted to the medical staff of any of our hospitals, but the hospital’s medical staff and the appropriate governing board of the hospital, in accordance with established credentialing criteria, must approve acceptance to the staff. Members of the medical staffs of our hospitals often also serve on the medical staffs of other hospitals and may terminate their affiliation with one of our hospitals at any time.
We believe that our employees are vital contributors to our success, and we devote significant resources to recruit, retain and develop our workforce. Certain areas of focus in this regard are summarized below.
Diversity, Equity and Inclusion
We believe that a diverse workforce is a catalyst for positive and consistent patient outcomes and high quality care. With inclusion as our strategy, diversity and equity are the outcomes we expect. Our objective is to recruit and retain a diverse population of employees with respect to their experiences, education, socioeconomic status, race, color, ethnicity, religion, national origin, disability, culture, sexual orientation and gender identity or expression that are reflective of the communities we serve. As of December 31, 2023, approximately 80% of our employees were women and approximately 29% were people of color.
21
As we strive to deepen our culture of inclusion, our goal is to strengthen our individual and collective cultural competence through both formal training and development programs and by informally sharing lived experiences and relating to one another. We are committed to building a diverse talent pipeline through a variety of venues and programs such as internships, residencies, mentorship programs and by partnering with diverse professional organizations. We formed the Diversity Leadership Committee in 2021, which has undertaken various actions with respect to diversity, equity and inclusion objectives such as retaining and developing high potential employees, improving patient experience and outcomes and increasing supplier diversity. We intend to leverage data to inform and measure the effectiveness of our diversity, equity and inclusion efforts over time.
Training and Talent Development
The delivery of high quality patient care is predicated on proper education and continued training. We provide a wide range of development programs and resources to support our employees, including temporary and contract personnel. In this regard, our talent development strategy is facilitated through our Advanced Learning Center platform, or ALC, a web-based portal, which provides employees and contractors access to computer based training courses as well as instructor-led classes. Our ALC provides training in many areas, including clinical, compliance, information technology, employee development, health information management, human resources, workplace safety and security, as well as hands-on resuscitation skills training. We offer continuing education credits for many of these disciplines. We are committed to continue to offer a quality library of training courses, which, at present, consists of approximately 9,300 courses published companywide, with a significant number of additional courses published at local facility levels.
The quality of our training is assured through a robust annual course review process. Each course is reviewed by the author or subject matter expert for current accuracy of content, relevancy and utilization. Updates are made based on current standards as well as feedback from individuals who complete the courses. Under the direction of our senior leadership, some courses are assigned to learners based on their role in our organization. The vast majority of the library is available for self-enrollment by our employees at no additional cost to the learner.
We also provide a wide range of other development programs and resources as part of our Pathways benefit offering. Pathways includes an expanded tuition reimbursement program for all staff looking to further their education in any discipline offered by our health systems, a new student loan repayment program for numerous key clinical roles and reimbursement for licenses and certifications that are required for each individual role. We operate nursing school programs on some of our hospital campuses and partner with nursing schools in many of our communities, as a way to provide educational pathways to those desiring to become professional nurses; an executive development program, which identifies and develops qualified personnel for leadership-level positions at our healthcare facilities; our Community Leadership Excellence and Development Series, or LEADS, which is a proprietary training program for directors, managers and supervisors at our hospitals and corporate offices; and residency training programs.
Employee Safety
The safety of our employees is of the utmost importance and is key to the continuous delivery of high quality patient care. We strive to protect our employees through continued communication, data analysis, equipment evaluation and education. Leadership methods, which employ a “safety-first” mindset, are practiced in our hospitals, including in safety huddles performed regularly by personnel at our hospitals. Each huddle consists of a three-part agenda: (1) a look back at any significant safety or quality issues in the past 24 hours, (2) a look ahead to any anticipated safety or quality issues in the next 24 hours, and (3) a follow-up on safety critical issues requiring a rapid response.
Environmental Matters
We are subject to a number of federal, state and local environmental laws, rules and regulations that govern, among other things, our disposal of medical waste, as well as our use, storage, transportation and disposal of hazardous and toxic materials. In addition, we could be affected by climate change to the extent that climate change results in severe weather conditions or other disruptions impacting the communities in which our facilities are located or adversely impacts general economic conditions, including in communities in which our facilities are located. Moreover, legal requirements regulating greenhouse gas emissions and energy inputs or otherwise associated with the transition to a lower carbon economy may increase in the future, which could increase our costs associated with compliance and otherwise disrupt and adversely affect our operations.
22
At the current time, our compliance with environmental legal requirements, including legal requirements relating to climate change, does not have a material effect on our capital expenditures, financial results or operations. However, it is possible that future environmental-related developments may impact us, including as a result of climate change and/or new legal requirements associated with the transition to a lower carbon economy, in a manner that we are currently unable to predict.
We recognize the environment is an exhaustible resource and the importance of using the environment and its resources responsibly. We have taken actions with respect to various sustainability matters with a focus on the reduction of our carbon footprint, water and energy usage and material waste. For additional information about our ongoing environmental sustainability actions and practices, refer to our most recent Environmental Sustainability Report, which is available in the Company Overview-Sustainability section of our website. Notwithstanding the foregoing, the information on our website, including our most recent Environmental Sustainability Report, is not incorporated by reference into this Form 10-K.
Professional Liability Claims
As part of our business of owning and operating hospitals, we are subject to legal actions alleging liability on our part. To cover claims arising out of the operations of hospitals, we maintain professional liability insurance and general liability insurance on a claims-made basis in excess of those amounts for which we are self-insured, in amounts we believe to be sufficient for our operations. We also maintain umbrella liability coverage for claims, which, due to their nature or amount, are not covered by our other insurance policies. However, our insurance coverage does not cover all claims against us or may not continue to be available at a reasonable cost for us to maintain adequate levels of insurance. For a further discussion of our insurance coverage, see our discussion of professional liability claims in “Management’s Discussion and Analysis of Financial Condition and Results of Operations” in Part II, Item 7 of this Form 10-K.
23
Item 1A. Risk Factors
Our business faces a variety of risks. If any of the events or circumstances described in any of the following risk factors occurs, our business, results of operations or financial condition could be materially and adversely affected, and our actual results may differ materially from those predicted in any forward-looking statements we make in any public disclosures. The considerations and risks that follow are organized within relevant headings but may be relevant to other headings as well. Additional factors that could affect our business, results of operations and financial condition are discussed elsewhere in this Report (including in “Management’s Discussion and Analysis of Financial Condition and Results of Operations” in Part II, Item 7 of this Form 10-K). Moreover, risks or uncertainties not presently known to us, or that we currently deem immaterial, also may adversely affect our business, results of operations and financial condition.
Summary of Risk Factors
The following is a summary of the risk factors set forth below.
Risks Related to Our Indebtedness
Risks Related to Economic Conditions
Risks Related to Our Business
Risks Related to Human Capital
24
Risks Related to Legal Proceedings
Risks Related to Government Regulation
Risks Related to Impairment
Risks Related to Cybersecurity and Technology
For a more complete discussion of these risk factors, see below.
Risks Related to Our Indebtedness
Our level of indebtedness could adversely affect our ability to refinance existing indebtedness or raise additional capital to fund our operations, limit our ability to react to changes in the economy or our industry and prevent us from meeting our obligations under the agreements related to our indebtedness.
We have a significant amount of indebtedness, which is more fully described in the Liquidity and Capital Resources section of “Management’s Discussion and Analysis of Financial Condition and Results of Operations” in Part II, Item 7 of this Form 10-K and Note 6 of the Notes to Consolidated Financial Statements included under Part II, Item 8 of this Form 10-K. The maximum aggregate principal amount under the ABL Facility is $1.0 billion, subject to borrowing base capacity. At December 31, 2023, we had outstanding borrowings of $247 million and approximately $637 million of additional borrowing capacity (after taking into consideration $81 million of outstanding letters of credit) under the ABL Facility.
25
Our substantial leverage could have important consequences, including the following:
Despite current indebtedness levels, we may still be able to incur substantially more debt. This could further exacerbate the risks described in this section.
We and our subsidiaries have the ability to incur substantial additional indebtedness in the future, subject to restrictions contained in the ABL Facility and the indentures governing our outstanding notes. The maximum aggregate principal amount under the ABL Facility is $1.0 billion, subject to borrowing base capacity. At December 31, 2023, we had outstanding borrowings of $247 million and approximately $637 million of additional borrowing capacity (after taking into consideration $81 million of outstanding letters of credit) under the ABL Facility. The aggregate amount we may draw under the ABL Facility may not exceed the “borrowing base” (as calculated thereunder) less outstanding letters of credit thereunder, which fluctuates from time to time. Aside from the ABL Facility, our ability to incur other additional secured debt (other than secured debt used to refinance existing secured debt) is highly limited by certain of the indentures governing our outstanding notes. If additional indebtedness is added to our current debt levels, the related risks that we currently face related to indebtedness as noted in this section could increase.
We may not be able to generate sufficient cash to service all of our indebtedness, and we may be forced to take other actions to satisfy our obligations under our indebtedness, which may not be successful.
Our ability to make scheduled payments on or to refinance our indebtedness depends on our financial and operating performance, which is subject to prevailing economic and competitive conditions and to financial, business, regulatory and other factors beyond our control. We cannot assure you that we will maintain a level of cash flows from operating activities sufficient to permit us to pay the principal, premium, if any, and interest on our indebtedness.
In addition, the borrower under the ABL Facility and issuer of our outstanding notes is a holding company with no direct operations. Its principal assets are the equity interests we hold in our operating subsidiaries. As a result, we are dependent upon dividends and other payments from our subsidiaries to generate the funds necessary to meet our outstanding debt service and other obligations. Our subsidiaries may not generate sufficient cash from operations to enable us to make principal and interest payments on our indebtedness. In addition, any payments of dividends, distributions, loans or advances to us by our subsidiaries could be subject to legal and contractual restrictions.
Our subsidiaries are permitted under the terms of our indebtedness to incur additional indebtedness that may restrict payments from those subsidiaries to us. The agreements governing the current and future indebtedness of our subsidiaries may not permit those subsidiaries to provide us with sufficient cash to fund payments on our indebtedness when due. Our non-guarantor subsidiaries are separate and distinct legal entities, and they have no obligation, contingent or otherwise, to pay amounts due under the terms of our indebtedness or to make any funds available to pay those amounts, whether by dividend, distribution, loan or other payment. If our cash flows and capital resources are insufficient to fund our debt service obligations, we could face substantial liquidity problems and may be forced to reduce or delay capital expenditures, sell assets or operations, seek additional capital or restructure or refinance our indebtedness. Our ability to refinance our indebtedness on favorable terms, or at all, is directly affected by the then current macroeconomic conditions, financial and capital market conditions as well as the then current interest rate environment. In addition, our ability to incur additional secured indebtedness (which would generally enable us to achieve better pricing than the incurrence of unsecured indebtedness) depends in part on the value of our assets, which depends, in turn, on the strength of our cash flows and results of operations, and on economic and market conditions and other factors. We may find it necessary or prudent to refinance certain of our outstanding indebtedness, the terms of which may not be favorable to us.
26
We cannot assure you that we would be able to take any of these actions, that these actions would be successful and permit us to meet our scheduled debt service obligations or that these actions would be permitted under the terms of our existing or future debt agreements, including the ABL Facility and the indentures governing our outstanding notes. For example, the ABL Facility and the indentures governing our outstanding notes restrict our ability to dispose of certain assets and use the proceeds from any dispositions. We may not be able to consummate those dispositions and any proceeds we receive may not be adequate to meet any debt service obligations then due.
We have a substantial amount of indebtedness under certain series of our outstanding notes and other debt scheduled to mature in close proximity to each other.
As further described in the Liquidity and Capital Resources section of “Management’s Discussion and Analysis of Financial Condition and Results of Operations” in Part II, Item 7 of this Form 10-K and Note 6 of the Notes to Consolidated Financial Statements included under Part II, Item 8 of this Form 10-K, we have a substantial amount of indebtedness under certain series of our outstanding notes and other debt scheduled to mature in close proximity to each other. As a result, we may not have sufficient cash to repay all amounts owing under such indebtedness and there can be no assurance that we will have the ability to borrow or otherwise raise the amounts necessary to repay all such amounts, and the prior maturity of such other substantial indebtedness may make it difficult to refinance the notes or repay them at maturity. Our ability to refinance our indebtedness on favorable terms, or at all, is dependent on (among other things) conditions in the credit and capital markets, which are beyond our control.
Restrictive covenants in the agreements governing our indebtedness may adversely affect us.
The ABL Facility and the indentures governing our outstanding notes contain various covenants that limit our ability to take certain actions, including our ability to:
In addition, the ABL Facility contains restrictive covenants and may, in certain circumstances, require us to maintain a specified financial ratio and satisfy other financial condition tests. Our ability to meet these restrictive covenants and financial ratio and tests (if applicable) may be affected by events beyond our control, and we cannot assure you that we will meet those tests.
In addition, our ability to incur additional secured debt (other than (i) secured debt to refinance existing secured debt and (ii) indebtedness incurred under our ABL Facility) is highly limited.
A breach of any of these covenants could result in a default under the ABL Facility and the indentures governing our outstanding notes. Upon the occurrence of an event of default under the ABL Facility or any of the indentures governing our outstanding notes, all amounts outstanding under the applicable indebtedness may become immediately due and payable and all commitments under the ABL Facility to extend further credit may be terminated. If we were unable to repay those amounts, the holders of such indebtedness could, subject to applicable intercreditor agreements, proceed against the collateral granted to them to secure that indebtedness. If holders of any of our indebtedness accelerate the maturity date of any of our indebtedness, we cannot assure you that we will have sufficient assets to repay the indebtedness that has been accelerated (and all other indebtedness that is also accelerated by virtue of applicable cross-acceleration provisions in the agreements governing our indebtedness).
27
Higher interest rates could increase the cost of refinancing our indebtedness and could cause our debt service obligations to increase significantly.
The current high interest rate environment could adversely impact us. If interest rates remain at their current elevated levels or continue to increase, this could adversely impact our ability to refinance existing indebtedness or obtain additional debt financing on acceptable terms or at all, and otherwise could increase our debt service obligations in connection with future debt refinancings. In addition, any borrowings under the ABL Facility are at variable rates of interest and expose us to interest rate risk. If interest rates increase, our debt service obligations on such variable rate indebtedness would increase even though the amount borrowed remained the same, and our net income would decrease. As of December 31, 2023, we had outstanding borrowings of $247 million under the ABL Facility.
If we default on our obligations to pay our indebtedness, or if we otherwise fail to comply with the various covenants in the instruments governing our indebtedness, we could be in default under the terms of the agreements governing our indebtedness.
If we are unable to generate sufficient cash flow and are otherwise unable to obtain funds necessary to meet required payments of principal, premium, if any, and interest on our indebtedness, or if we otherwise fail to comply with the various covenants, including financial and operating covenants, in the instruments governing our indebtedness, including covenants in the ABL Facility and the indentures governing our outstanding notes, we could be in default under the terms of the agreements governing such indebtedness. In the event of any default, the holders of such indebtedness could elect to declare all the funds borrowed to be immediately due and payable, together with accrued and unpaid interest; the lenders under the ABL Facility could elect to terminate their commitments thereunder, cease making further loans and direct the applicable collateral agents to institute foreclosure proceedings against our assets; and we could be forced into bankruptcy or liquidation. If our operating performance declines, we may in the future need to obtain waivers from the required lenders under the ABL Facility to avoid being in default. If we breach our covenants under the ABL Facility and seek a waiver, we may not be able to obtain a waiver from the required lenders. If this occurs, we would be in default under the ABL Facility, the lenders could exercise their rights, as described above, and we could be forced into bankruptcy or liquidation.
Risks Related to Economic Conditions
Our financial results have been, and may continue to be, adversely impacted by negative macroeconomic conditions.
Economic conditions in the United States continue to be challenging in various respects, and the United States economy continues to experience significant inflationary pressures, elevated interest rates, challenging labor market conditions, and possible adverse effects associated with current geopolitical instability. Taking into account these factors, we have incurred in certain recent periods, and may continue to incur, increased expenses arising from factors such as wage inflation for permanent employees, increased rates for and utilization of temporary contract labor (including contract nursing personnel), and increased rates for outsourced medical specialists. Moreover, if economic conditions in the United States significantly deteriorate, any such developments could materially and adversely affect our results of operations, financial position, and/or our cash flows.
Other risks we face during periods of economic weakness include potential declines in the population covered under commercial insurance agreements, increased patient decisions to postpone or cancel elective and non-emergency healthcare procedures (including delaying surgical procedures), which may lead to poorer health and higher acuity interventions, potential increases in the uninsured and underinsured populations, increased adoption of health plan structures that shift financial responsibility to patients, and increased difficulties in collecting patient receivables for copayment and deductible receivables. In addition, negative macroeconomic conditions in the United States have resulted in, and may continue to result in, increased budget deficits at federal, state and local governmental levels, which may continue to negatively impact spending for health and human services programs, including Medicare, Medicaid and similar programs, which represent significant third-party payor sources for our healthcare facilities. Moreover, it is difficult to predict whether, when, or what additional deficit reduction initiatives may be proposed by Congress, but future legislation may include additional Medicare spending reductions, which may adversely affect our business and financial results due to our reliance on Medicare payments. Further, there is ongoing uncertainty regarding the federal budget and federal spending levels, including the possible impacts of a failure to increase the “debt ceiling.” Any U.S. government default on its debt could have broad macroeconomic effects. In addition, negative macroeconomic conditions in the United States (including elevated interest rates) have had, and may continue to have, an adverse impact on capital market conditions, which could limit our ability to refinance existing indebtedness or obtain additional debt or equity financing on acceptable terms or at all.
28
Risks Related to Our Business
If we are unable to complete divestitures as we may deem advisable, our results of operations and financial condition could be adversely affected.
We have divested certain of our hospitals and non-hospital businesses in recent years, and may give consideration to divesting certain additional hospitals and non-hospital businesses. For a description of recent divestitures, see “Acquisition, Divestiture and Closure Activity” under Part II, Item 7 of this Form 10-K. Generally, these hospitals and non-hospital businesses are not in one of our strategically beneficial service areas, are less complementary to our business strategy and/or have lower operating margins. In addition, we continue to receive interest from potential acquirers for certain of our hospitals and non-hospital businesses. As such, we may sell additional hospitals and/or non-hospital businesses if we consider any such disposition to be in our best interests. However, there is no assurance that potential divestitures will be completed or, if they are completed, the aggregate amount of proceeds we will receive, that potential divestitures will be completed within our targeted timeframe, or that potential divestitures will be completed on terms favorable to us. Moreover, the current negative macroeconomic environment may make it more difficult for us to complete divestitures on acceptable terms, or at all. Additionally, the results of operations for these hospitals and non-hospital businesses that we may divest and the potential gains or losses on the sales of those businesses may adversely affect our results of operations. We may also incur asset impairment charges related to potential or completed divestitures that reduce our profitability. In addition, after entering into a definitive agreement, we may be subject to the satisfaction of pre-closing conditions as well as necessary regulatory and governmental notices and approvals, which, if not satisfied or obtained, may prevent us from completing the sale. Divestitures may also involve continued financial exposure related to the divested business, such as through indemnities or retained obligations, that present risk to us.
Any future divestiture activities may present financial, managerial, and operational risks. Those risks include diversion of management attention from improving existing operations; additional restructuring charges and the related impact from separating personnel, renegotiating contracts, and restructuring financial and other systems; adverse effects on existing business relationships with patients and third-party payors; and the potential that the collectability of any patient accounts receivable retained from any divested hospital may be adversely impacted. Any of these factors could adversely affect our financial condition and results of operations.
The impact of past acquisitions, as well as potential future acquisitions, could have a negative effect on our operations.
Our business strategy has historically included growth by acquisitions, and we may complete additional acquisitions in the future. However, not-for-profit hospital systems and other for-profit hospital companies generally attempt to acquire the same type of hospitals as we may desire to acquire. Some of the competitors for our acquisitions have greater financial resources than we have. Furthermore, some hospitals are sold through an auction process, which may result in higher purchase prices than we believe are reasonable. Therefore, we may not be able to acquire additional hospitals on terms favorable to us.
In addition, many of the hospitals we have previously acquired have had lower operating margins than we do and operating losses incurred prior to the time we acquired them. Hospitals or other businesses acquired in the future may have similar financial performance issues. In the past, we have experienced delays in improving the operating margins or effectively integrating the operations of certain acquired hospitals and other businesses. In the future, if we are unable to improve the operating margins of acquired hospitals or other businesses, operate them profitably, or effectively integrate their operations, our results of operations and business may be adversely affected.
Moreover, hospitals or other businesses that we have acquired, or in the future could acquire, may have unknown or contingent liabilities, including liabilities associated with ongoing legal proceedings or for failure to comply with healthcare laws and regulations. Although we generally seek indemnification from sellers covering these matters, we may nevertheless have material liabilities for past activities of acquired hospitals.
If we are unable to effectively compete, patients could use other hospitals and healthcare providers, and our business may be adversely impacted.
The healthcare industry is highly competitive among hospitals and other healthcare providers, such as urgent care centers and other outpatient providers and other industry participants, for patients, affiliations with physicians and acquisitions. Changes in licensure or other regulations, recognition of new provider types or payment models, and industry consolidation could negatively impact our competitive position. For example, in states with certificate of need or similar prior approval requirements, removal of these requirements could remove barriers to entry and increase competition in our service areas. Our hospitals, our competitors, and other healthcare industry participants are increasingly implementing physician alignment strategies, such as acquiring physician practice groups, employing physicians and participating in ACOs or other clinical integration models. Increasing consolidation within the
29
payor industry, vertical integration efforts involving payors and healthcare providers, and cost-reduction strategies by payors, large employer groups and their affiliates may impact our ability to contract with payors on favorable terms, participate in favorable payment tiers or provider networks, and otherwise affect our competitive position. Legislative and regulatory initiatives, such as changes in Texas law that eliminated restrictions on tiered networks and steering patients to particular providers, may accelerate or otherwise impact these trends.
The majority of our hospitals are located in generally larger non-urban service areas in which we believe we are the primary, if not the sole, provider of general acute care health services. As a result, the most significant competition for providers of general acute care services are hospitals outside of our primary service areas, typically hospitals in larger urban areas that provide more complex services. Patients in our primary service areas may travel to other hospitals because of physician referrals, payor networks that exclude our providers or the need for services we do not offer, among other reasons. Patients who receive services from these other hospitals may subsequently shift their preferences to those hospitals for the services we provide.
Our other hospitals, in selected urban service areas, may face competition from hospitals that are more established than our hospitals. Some of our competitors offer services, including extensive medical research and medical education programs, that are not offered by our facilities. In addition, in certain markets where we operate, there are large teaching hospitals that provide highly specialized facilities, equipment and services that may not be available at our hospitals. We also face competition from other specialized care providers, including outpatient surgery, orthopedic, oncology and diagnostic centers.
At December 31, 2023, 43 of our hospitals competed with one or more non-affiliated hospitals in their respective primary service areas. In most markets in which we are not the sole provider of general acute care health services, our primary competitor is a municipal or not-for-profit hospital. These hospitals are owned by tax-supported governmental agencies or not-for-profit entities supported by endowments and charitable contributions. These hospitals are exempt from sales, property and income taxes. Such exemptions and support are not available to our hospitals and may provide the tax-supported or not-for-profit entities an advantage in funding general and capital expenditures and offering services more specialized than those available at our hospitals. If our competitors are better able to attract patients with these offerings, we may experience an overall decline in patient volume.
Trends toward transparency and value-based purchasing may have an impact on our competitive position, ability to obtain and maintain favorable contract terms, and patient volumes in ways that are difficult to predict. The CMS Care Compare website makes available to the public certain data that hospitals submit in connection with Medicare reimbursement claims, including performance data related to quality measures and patient satisfaction surveys. Further, every hospital must establish and update annually a public, online listing of the hospital’s standard charges for all items and services, including discounted cash prices and payor-specific charges, and must also publish a consumer-friendly list of standard charges for certain “shoppable” services or, alternatively, maintain an online price estimator tool for the shoppable services. HHS also requires health insurers to publish online charges negotiated with providers for healthcare services, and health insurers must provide online price comparison tools to help individuals get personalized cost estimates for all covered items and services. If any of our hospitals achieve poor results (or results that are lower than our competitors) on the quality measures or on patient satisfaction surveys, or if our standard charges are higher than our competitors, we may attract fewer patients.
The No Surprises Act creates additional price transparency requirements that may impact our competitive position, including requiring providers to send uninsured or self-pay patients and health plans of insured patients a good faith estimate of the expected charges and diagnostic codes prior to the scheduled date of the service or item or upon request. Until HHS issues additional regulations, HHS is deferring enforcement of portions of the good faith estimate requirements. It is unclear how price transparency requirements and similar initiatives will affect consumer behavior, our relationships with payors, or our ability to set and negotiate prices.
We expect these competitive trends to continue. If we are unable to compete effectively with other hospitals and other healthcare providers, patients may seek healthcare services at providers other than our hospitals and affiliated businesses.
We may be adversely affected by consolidation among health insurers and other industry participants.
In recent years, a number of health insurers have merged or increased efforts to consolidate with other non-governmental payors. Insurers are also increasingly pursuing alignment initiatives with healthcare providers. Consolidation within the health insurance industry may result in insurers having increased negotiating leverage and competitive advantages, such as greater access to performance and pricing data. Our ability to negotiate prices and favorable terms with health insurers in certain markets could be affected negatively as a result of this consolidation. Also, the shift toward value-based payment models could be accelerated if larger insurers, including those engaging in consolidation activities, find these models to be financially beneficial. We cannot predict whether we will be able to negotiate favorable terms with payors and otherwise respond effectively to the impact of increased consolidation in the payor industry or vertical integration efforts.
30
The failure to obtain our medical supplies at favorable prices could cause our operating results to decline.
We have a participation agreement with HealthTrust, a GPO. The current term of this agreement extends through the end of December 2024, with automatic renewal terms of one year, unless either party terminates by giving notice of non-renewal. GPOs attempt to obtain favorable pricing on medical supplies with manufacturers and vendors, sometimes by negotiating exclusive supply arrangements in exchange for discounts. To the extent these exclusive supply arrangements are challenged or deemed unenforceable, we could incur higher costs for our medical supplies obtained through HealthTrust. Further, costs of supplies and drugs may continue to increase due to market pressure from pharmaceutical companies and new product releases, among other factors. Also, there can be no assurance that our arrangement with HealthTrust will provide the discounts we expect to achieve.
If reimbursement rates paid by federal or state healthcare programs or commercial payors are reduced, if we are unable to maintain favorable contract terms with payors or comply with our payor contract obligations, if insured individuals move to insurance plans with greater coverage exclusions or narrower networks, or if insurance coverage is otherwise restricted or reduced, our net operating revenues may decline.
During the year ended December 31, 2023, 34.2% of our net operating revenues came from the Medicare and Medicaid programs. However, as federal healthcare expenditures continue to increase and state governments continue to face budgetary shortfalls, federal and state governments have made, and continue to make, significant changes in the Medicare and Medicaid programs, including reductions in reimbursement levels. For example, as a result of sequestration measures that extend through April 2032, Medicare payments are automatically reduced by 2%. In addition, as a result of the ARPA, an additional Medicare payment reduction of up to 4% was required to take effect in January 2022; however, Congress has delayed implementation of this reduction until 2025. In addition, CMS may implement changes through new or modified demonstration projects authorized pursuant to Medicaid waivers. Some of these changes have decreased, or could decrease, the amount of money we receive for our services relating to these programs.
In addition, government and commercial payors as well as other third parties from whom we receive payment for our services attempt to control healthcare costs by, for example, requiring hospitals to discount payments for their services in exchange for exclusive or preferred participation in their benefit plans, restricting coverage through utilization review, reducing coverage of inpatient and emergency room services and shifting care to outpatient settings, requiring prior authorizations, and implementing alternative payment models. The ability of commercial payors to control healthcare costs using these measures may be enhanced by the increasing consolidation of insurance and managed care companies, vertical integration of health insurers with healthcare providers and regulatory changes.
Limitations on balance billing may also reduce the amount that hospitals and other providers are able to collect for out-of-network services. For example, the No Surprises Act prohibits providers from charging patients an amount beyond the in-network cost sharing amount for services rendered by out-of-network providers, subject to limited exceptions. For services for which balance billing is prohibited (even when no balance billing occurs), the No Surprises Act includes provisions that may limit the amounts received by out-of-network providers by health plans, and also establishes an independent dispute resolution process for providers and payors to handle payment disputes that cannot be resolved through direct negotiation. The regulations and related guidance implementing the No Surprises Act, including those establishing the dispute resolution process, are the subject of legal challenges and, potentially, regulatory changes.
In addition, price transparency initiatives may impact our ability to obtain or maintain favorable contract terms. For example, the No Surprises Act requires providers to send health plans of insured patients a good faith estimate of the expected charges and diagnostic codes prior to the scheduled date of the service or item. HHS is deferring enforcement of certain requirements related to good faith estimates until the agency issues additional regulations. Further, hospitals are required to publish online payor-specific negotiated charges and de-identified minimum and maximum charges. In addition, health insurers must provide online price comparison tools to help individuals get personalized cost estimates for covered items and services.
During the year ended December 31, 2023, 64.7% of our net operating revenues came from commercial payors. Our contracts with payors require us to comply with a number of terms related to the provision of services and billing for services. If we are unable to negotiate increased reimbursement rates, maintain existing rates or other favorable contract terms, effectively respond to payor cost controls and reimbursement policies or comply with the terms of our payor contracts, the payments we receive for our services may be reduced. Also, we are increasingly involved in disputes with payors and experience payment denials, both prospectively and retroactively. In addition, enrollment of individuals in high-deductible health plans, sometimes referred to as consumer-directed plans, has increased over the last decade. In comparison to traditional health plans, these plans tend to have lower reimbursement rates for providers along with higher co-pays and deductibles due from the patient, which subjects us to increased collection cost and risk. Further, high-deductible health plans may exclude our hospitals and employed physicians from coverage.
31
If we experience continued growth in self-pay volume and revenues or if we experience deterioration in the collectability of patient responsibility accounts, our financial condition or results of operations could be adversely affected.
Our primary collection risks relate to uninsured patients and outstanding patient balances for which the primary insurance payor has paid some but not all of the outstanding balance, with the remaining outstanding balance (generally deductibles and co-payments) owed by the patient. Collections are impacted by the economic ability of patients to pay and the effectiveness of our collection efforts. Significant changes in payor mix, business office operations, economic conditions or trends in federal and state governmental healthcare coverage may affect our collection of accounts receivable and are considered in our estimates of accounts receivable collectability.
In recent years, federal and state legislatures have considered or passed various proposals impacting or potentially impacting the size of the uninsured population. The number and identity of states that choose to expand or otherwise modify Medicaid programs and the terms of expansion and other program modifications continue to evolve. Further, early COVID-related legislation authorized a temporary increase in federal funds for state Medicaid expenditures in states that maintained continuous Medicaid enrollment, among other requirements. The resumption of Medicaid eligibility redeterminations following the expiration of this continuous coverage requirement in April 2023 has resulted in significant Medicaid coverage disruptions and dis-enrollments. Medicaid enrollment is generally expected to decline through fiscal year 2024 (which ends June 30, 2024, in most states). CMS has required certain states to pause disenrollments due to noncompliant renewal systems. The ARPA temporarily increased the value of premium tax credit subsidies for subsidy-eligible individuals purchasing health insurance coverage through the federal and state-run marketplaces and expanded eligibility for the tax credit subsidies to more individuals. Subsequent legislation extended the enhanced subsidies through 2025. In addition, although the federal financial penalty associated with the Affordable Care Act’s mandate that individuals enroll in an insurance plan has been effectively eliminated, some states have imposed individual health insurance mandates with financial penalties for noncompliance. Other states have explored or offer public health insurance options. These variables, among others, make it difficult to predict the number of uninsured individuals and what percentage of our total revenue will be comprised of self-pay revenues.
We may be adversely affected by the growth in patient responsibility accounts as a result of the adoption of plan structures, including health savings accounts, narrow networks and tiered networks, that shift greater responsibility for care to individuals through greater exclusions and copayment and deductible amounts. Further, our ability to collect patient responsibility accounts may be limited by statutory, regulatory and investigatory initiatives, including private lawsuits directed at hospital charges and collection practices for uninsured and underinsured patients and regulatory restrictions on charges for out-of-network services. For example, the No Surprises Act requires providers to send uninsured and self-pay patients a good faith estimate of expected charges for items and services. The estimate must be provided in advance of the scheduled date for the item or service or upon request and cover items and services that are reasonably expected to be provided together with the primary item or services, including those that may be provided by other providers. If the uninsured or self-pay patient receives a bill that is substantially greater than the expected charges in the good faith estimate or the provider furnishes an item or service that was not included in the good faith estimate, they may initiate a patient-provider dispute resolution process established by regulation. In addition, a deterioration of economic conditions in the United States could potentially lead to higher levels of uninsured patients, result in higher levels of patients covered by lower paying government programs, result in fiscal uncertainties for both government payors and private insurers and/or limit the economic ability of patients to make payments for which they are responsible. If we experience continued growth in self-pay volume or deterioration in collectability of patient responsibility accounts, our financial condition or results of operations could be adversely affected.
Some of the non-urban communities in which we operate face challenging economic conditions, and the failure of certain employers, or the closure of certain manufacturing and other facilities in our markets, could have a disproportionate impact on our hospitals.
Some of the non-urban communities in which we operate have been facing particularly challenging economic conditions, which in certain instances predate, and/or are broader than or disproportionately exacerbated by, the current negative macroeconomic conditions impacting the United States economy. In addition, the economies in the non-urban communities in which our hospitals primarily operate are often dependent on a small number of large employers, especially manufacturing or similar facilities. These employers often provide income and health insurance for a disproportionately large number of community residents who may depend on our hospitals for care. The failure of one or more large employers, or the closure or substantial reduction in the number of individuals employed at manufacturing or other facilities located in or near many of the non-urban communities in which our hospitals primarily operate, could cause affected employees to move elsewhere for employment or lose insurance coverage that was otherwise available to them. When patients are experiencing personal financial difficulties or have concerns about general economic conditions, they may delay or forgo elective procedures, choose to seek care in emergency rooms and purchase high-deductible insurance plans or no insurance at all, which increases a hospital’s dependence on self-pay revenue and may adversely affect our results of operations.
32
The demand for services provided by our hospitals and affiliated providers can be impacted by factors beyond our control.
Our admissions and adjusted admissions as well as acuity trends may be impacted by factors beyond our control. For example, seasonal fluctuations in the severity of influenza and other critical illnesses, such as COVID-19, unplanned shutdowns or unavailability of our facilities due to weather or other unforeseen events, decreases in trends in high acuity service offerings, changes in competition from other service providers, turnover in physicians affiliated with our hospitals, or changes in medical technology can have an impact on the demand for services at our hospitals and affiliated providers.
In addition, certain of our facilities are located in hurricane-prone coastal regions in Florida and other states, and our operations may be adversely impacted by hurricanes, tornadoes, winter storms, and other severe weather conditions, which adverse weather conditions may be more frequent and/or severe as the result of climate change. Moreover, we could be affected by climate change and other environmental issues to the extent such issues adversely affect the general economy or specific markets, adversely impact our supply chain or increase the costs of supplies needed for our operations, or otherwise result in disruptions impacting the communities in which our facilities are located. In addition, legal requirements regulating greenhouse gas emissions and energy inputs or otherwise associated with the transition to a lower carbon economy may increase in the future, which could increase our costs associated with compliance and otherwise disrupt and adversely affect our operations. The impact of these or other factors beyond our control could have an adverse effect on our business, financial position and results of operations.
A deterioration of public health conditions associated with COVID-19, or a future pandemic, epidemic or outbreak of an infectious disease in the markets in which we operate or that otherwise impacts our facilities could adversely impact our business.
As a provider of healthcare services, we were significantly impacted by the public health and economic effects of the COVID-19 pandemic. If public health conditions related to COVID-19 significantly worsen, our business and financial results could be adversely impacted. Moreover, conditions related to COVID-19 continue to evolve, and we may not be able to predict or effectively respond to future developments.
In response to the COVID-19 pandemic, the federal government authorized financial relief for eligible healthcare providers through the Public Health and Social Services Emergency Fund, or PHSSEF. Although recipients are not required to repay funding received, provided they attest to and comply with certain terms and conditions, changes to interpretations of guidance on the underlying terms and conditions may result in the derecognition of amounts previously realized. To the extent that any unrecognized PHSSEF payments that have been received by us do not qualify for reimbursement, we may be required to return such payments. Further, we may be subject to or incur costs from related government actions including payment recoupment, audits and inquiries by governmental authorities, and criminal, civil or administrative penalties.
In addition, if a future pandemic, epidemic, or outbreak of an infectious disease or other public health crisis were to affect our markets, our business could be adversely affected. Any such crisis could diminish the public trust in healthcare facilities, especially hospitals that fail to accurately or timely diagnose, or that are treating (or have treated) patients affected by, contagious diseases. If any of our facilities are involved, or perceived as being involved, in treating patients for such a contagious disease, other patients might cancel elective procedures or fail to seek needed care at our facilities. Patient volumes may decline or volumes of uninsured and underinsured patients may increase, depending on the economic circumstances surrounding the pandemic, epidemic, or outbreak. Further, a pandemic, epidemic, or outbreak might adversely impact our business by causing a temporary shutdown or diversion of patients, by causing disruption or delays in supply chains for materials and products or by causing staffing shortages in our facilities. Although we have contingency plans in place, including infection control and disaster plans, the potential impact of, as well as the public’s and government’s response to, any such future pandemic, epidemic or outbreak of an infectious disease with respect to our markets or our facilities is difficult to predict and could adversely impact our business.
The industry trend towards value-based purchasing may negatively impact our business.
There is a trend toward value-based purchasing of healthcare services across the healthcare industry among both government and commercial payors. Generally, value-based purchasing initiatives tie payment to the quality and efficiency of care. For example, hospital payments may be negatively impacted by the occurrence of HACs. Medicare does not reimburse for care related to HACs, by disallowing the hospital to be assigned a higher paying MS-DRG if certain HACs were not present on admission and the identified HAC is the only condition resulting in the assignment of the higher paying MS-DRG. Hospitals in the bottom quartile of HAC rates receive a 1% reduction in their total Medicare payments the following year. In addition, federal funds may not be used under the Medicaid program to reimburse providers for services provided to treat HACs. Hospitals that experience excess readmissions for designated conditions receive reduced payments for all inpatient discharges in the fiscal year. HHS also reduces Medicare inpatient hospital payments for all discharges by a required percentage and pools the amount collected from these reductions to fund payments to reward hospitals that meet or exceed certain quality performance standards. Further, Medicare and Medicaid require hospitals to report certain quality data to receive full reimbursement updates.
33
HHS continues to focus on tying Medicare payments to quality or value through alternative payment models, which generally aim to make providers attentive to the quality and cost of care they deliver to patients. Examples of alternative payment models include ACOs and bundled payment arrangements. An ACO is a care coordination model intended to produce savings as a result of improved quality and operational efficiency. By 2030, the CMS Innovation Center aims to have all fee-for-service Medicare beneficiaries and the vast majority of Medicaid beneficiaries in an accountable care relationship with providers who are responsible for quality and total medical costs. In bundled payment models, providers receive one payment for services provided to patients for certain medical conditions or episodes of care, accepting accountability for costs and quality of care. Providers may receive supplemental Medicare payments or owe repayments to CMS depending on whether spending exceeds or falls below a specified spending target and whether certain quality standards are met. Generally, participation in Medicare bundled payment programs is voluntary, but CMS currently requires hospitals in selected markets to participate in bundled payment initiatives for specific orthopedic procedures and end-stage renal disease treatment. A mandatory radiation oncology bundled payment model was expected to begin January 1, 2023, but CMS has indefinitely delayed its implementation. CMS has signaled its intent to streamline its payment models and to increase provider participation through implementation of more mandatory models.
There are also several state-driven value-based care initiatives. For example, some states have aligned quality metrics across payors through legislation or regulation. Commercial payors are transitioning toward value-based reimbursement arrangements as well. Further, many commercial payors require hospitals to report quality data and restrict reimbursement for certain preventable adverse events.
We expect value-based purchasing programs, including programs that condition reimbursement on patient outcome measures, to become more common and to involve a higher percentage of reimbursement amounts. It is unclear whether these and other alternative payment models will successfully coordinate care and reduce costs or whether they will decrease aggregate reimbursement. While we believe we are adapting our business strategies to compete in a value-based reimbursement environment, we are unable at this time to predict how this trend will affect our results of operations. If we perform at a level below the outcomes demonstrated by our competitors, are unable to meet or exceed the quality performance standards under any applicable value-based purchasing program, or otherwise fail to effectively provide or coordinate the efficient delivery of quality healthcare services, our reputation in the industry may be negatively impacted, we may receive reduced reimbursement amounts and we may owe repayments to payors, causing our revenues to decline.
Our revenues are somewhat concentrated in a relatively small number of states, which makes us particularly sensitive to regulatory and economic changes in those states.
Our revenues are particularly sensitive to regulatory and economic changes in states in which we generate a significant portion of our revenues, including Indiana, Alabama, Texas and Florida. Accordingly, any change in the current demographic, economic, competitive, or regulatory conditions in these states could have an adverse effect on our business, financial condition, or results of operations. Changes to the Medicaid programs in these states could also have an adverse effect on our business, financial condition, results of operations, or cash flows. For example, the Texas Healthcare Transformation and Quality Improvement Program, or the Texas Waiver Program, which enables the expansion of Medicaid managed care programs in the state, provides funding for uncompensated care and includes several directed payment programs, is operated under a waiver granted pursuant to Section 1115 of the Social Security Act. The Texas waiver continues through 2030, but directed payment programs have more limited approval periods, such as the Comprehensive Hospital Increase Reimbursement Program, or CHIRP, which is currently set to expire on August 31, 2024. If Texas is unable to obtain future extensions or other approvals of the directed payment program or similar programs, our revenues could be negatively impacted. It is difficult to predict whether and how Medicaid programs, including their waiver programs, might be modified, extended or eliminated, any of which could negatively impact our revenues.
Risks Related to Human Capital
Our performance depends on our ability to recruit and retain quality physicians.
The success of our healthcare facilities depends in part on the number and quality of the physicians on the medical staffs of our healthcare facilities, our ability to employ quality physicians, the admitting and utilization practices of employed and independent physicians, maintaining good relations with those physicians and controlling costs related to the employment of physicians. Although we employ some physicians, physicians are often not employees at our healthcare facilities at which they practice. In many of the markets we serve, many physicians have admitting privileges at other healthcare facilities in addition to our healthcare facilities. Such physicians may terminate their affiliation with or employment by our healthcare facilities at any time. Moreover, we are facing increased competition from health insurers and private equity-backed companies seeking to acquire or affiliate with physicians or physician practices.
34
We may face increased challenges recruiting and retaining quality physicians as the physician population reaches retirement age, especially if there is a shortage of physicians willing and able to provide comparable services. In some markets, physician recruitment and retention may be affected by a shortage of physicians in certain specialties or the difficulties physicians may experience in obtaining professional liability insurance. The types, amount and duration of compensation and assistance we can provide when recruiting physicians are limited by the federal Physician Self-Referral Law (commonly known as the Stark Law), the federal Anti-Kickback Statute, similar state laws and implementing regulations. If we are unable to provide adequate support personnel or technologically advanced equipment and facilities that meet the needs of those physicians and their patients, our ability to recruit and retain quality physicians may be negatively impacted.
Our performance and labor costs have been, and may continue to be, adversely affected by challenging labor market conditions and the shortage of qualified nurses and other healthcare personnel.
The operations of our healthcare facilities are dependent on the efforts, abilities and experience of our facility management, healthcare professionals, such as nurses, pharmacists, lab technicians, and medical support personnel. We compete with other healthcare providers in recruiting and retaining qualified facility management and personnel responsible for the daily operations of our healthcare facilities, including nurses, other non-physician healthcare professionals and medical support personnel.
The healthcare industry has been experiencing a challenging labor market arising out of current macroeconomic conditions, and our hospitals and other healthcare facilities, like many other healthcare providers, have experienced increased labor costs. In some markets in which we operate, a shortage of available nurses, other healthcare professionals and medical support personnel has been a significant operating issue for healthcare providers, which has been exacerbated by current labor market conditions as noted above. Due to such challenges and other factors, our hospitals and other healthcare facilities, like other healthcare providers, have experienced increased labor costs. We may be required to continue to enhance wages and benefits to recruit and retain nurses, other healthcare professionals and medical support personnel, and/or to hire more expensive temporary or contract personnel. In addition, to the extent we are unable to maintain sufficient staffing levels at our hospitals, we may be required to limit the acute healthcare services provided at certain of our hospitals, which would have a corresponding adverse effect on our net revenues. We also depend on the available labor pool of semi-skilled and unskilled employees in each of the markets in which we operate. In some of our markets, employers across various industries have increased their wages for these roles, which has created more competition for this sector of employees. The impact of labor shortages across the healthcare industry may result in other healthcare facilities, such as nursing homes, limiting admissions, which may constrain our ability to discharge patients to such facilities and further exacerbate the demand on our resources.
In addition, the states in which we operate could adopt mandatory nurse-staffing ratios, could revise mandatory nurse-staffing ratios already in place or adopt other measures aimed at regulating staffing. State-mandated nurse-staffing ratios and similar measures could significantly affect labor costs and have an adverse impact on revenues if we are required to limit admissions or incur other costs in order to comply with such requirements.
We may be unable to attract, hire, and retain a highly qualified and diverse workforce, including key management.
At December 31, 2023, certain employees at three of our hospitals were represented by various labor unions. While we have not experienced work stoppages to date that have material and adversely affected our business or results of operations, increased or ongoing labor union activity could adversely affect our labor costs or otherwise adversely impact us. In addition, when negotiating collective bargaining agreements with unions, whether such agreements are renewals or first contracts, there is the possibility that strikes could occur during the negotiation process, and our continued operation during any strikes could increase our labor costs and otherwise adversely impact us. Finally, potential changes to federal labor laws and regulations, including those supported by the current presidential administration, could increase the likelihood of employee unionization activity and the ability of employees to unionize, which could adversely impact our operations and financial results.
If our labor costs continue to increase, we may not be able to raise rates to offset these increased costs. Because a significant percentage of our revenues consists of fixed, prospective payments, our ability to pass along increased labor costs is constrained. In the event we are not entirely effective at recruiting and retaining qualified facility management, nurses and other medical support personnel, or in controlling labor costs, this could continue to have an adverse effect on our results of operations.
35
We may be adversely impacted by the inability of third parties with whom we contract to provide hospital-based physicians as the result of industry-wide disruptions in the market for outsourced medical specialists.
We contract with various third parties who provide hospital-based physicians, including emergency, anesthesiology, hospitalist/inpatient care, radiology, tele-radiology and surgery. Third-party providers of hospital-based physicians, including those with whom we contract, have experienced significant disruption in the form of regulatory changes, including those stemming from enactment of the No Surprises Act, challenging labor market conditions resulting from a shortage of physicians and inflationary wage-related pressures, as well as increased competition through consolidation of physician groups. In some instances, providers of outsourced medical specialists have become insolvent and unable to fulfill their contracts with us for providing hospital-based physicians. The success of our hospitals depends in part on the adequacy of staffing, including through contracts with third parties. If we are unable to adequately contract with providers, or the providers with whom we contract become unable to fulfill their contracts, our admissions may decrease, and our operating performance, capacity and growth prospects may be adversely affected. Further, our efforts to mitigate the potential impact to our business from third-party providers who are unable to fulfill their contracts to provide hospital-based physicians, including through acquisitions of outsourced medical specialist businesses, employment of physicians and re-negotiation or assumption of existing contracts, may be unsuccessful. These developments with respect to providers of outsourced medical specialists, and our inability to effectively respond to and mitigate the potential impact of such developments, may disrupt our ability to provide healthcare services, which may adversely impact our business and financial results.
Risks Related to Legal Proceedings
We are the subject of various legal, regulatory and governmental proceedings that, if resolved unfavorably, could have an adverse effect on us, and we may be subject to other loss contingencies, both known and unknown.
We are a party to various legal, regulatory and governmental proceedings and other related matters. Those proceedings include, among other things, government investigations. In addition, we are and may become subject to other loss contingencies, both known and unknown, which may relate to past, present and future facts, events, circumstances and occurrences. Should an unfavorable outcome occur in connection with our current or potential future legal, regulatory or governmental proceedings or other loss contingencies, or if we become subject to any such loss contingencies in the future, there could be an adverse impact on our financial position, results of operations and liquidity.
In particular, government investigations, as well as qui tam lawsuits, may lead to significant fines, penalties, damages payments or other sanctions, including exclusion from government healthcare programs. Settlements of lawsuits involving Medicare and Medicaid issues routinely require both monetary payments and corporate integrity agreements, each of which could have an adverse effect on our business, financial condition, results of operations and/or cash flows.
We could be subject to substantial uninsured liabilities or increased insurance costs as a result of significant legal actions.
Physicians, hospitals and other healthcare providers have become subject to an increasing number of legal actions alleging professional liability, product liability, or related legal theories. Even in states that have imposed caps on damages, litigants are seeking recoveries under new theories of liability that might not be subject to the caps on damages. Many of these actions involve large claims and significant defense costs. To protect us from the cost of these claims, we maintain claims-made professional liability insurance and general liability insurance coverage in excess of those amounts for which we are self-insured. This insurance coverage is in amounts that we believe to be sufficient for our operations; however, our insurance coverage may not continue to be available at a reasonable cost for us to maintain adequate levels of insurance. Additionally, our insurance coverage does not cover all claims against us, such as fines, penalties, or other damage and legal expense payments resulting from qui tam lawsuits. We cannot predict the outcome of current or future legal actions against us or the effect that judgments or settlements in such matters may have on us or on our insurance costs. Additionally, all professional and general liability insurance we purchase is subject to policy limitations. If the aggregate limit of any of our professional and general liability policies is exhausted, in whole or in part, it could deplete or reduce the limits available to pay any other material claims applicable to that policy period. Furthermore, one or more of our insurance carriers could become insolvent and unable to fulfill its or their obligations to defend, pay or reimburse us when those obligations become due. In that case, or if payments of claims exceed our estimates or are not covered by our insurance, it could have an adverse effect on our business, financial condition or results of operations.
36
Risks Related to Government Regulation
Our business may be adversely impacted by health reform initiatives.
In recent years, the healthcare industry has undergone significant changes, many of which have been aimed at reducing costs and government spending. The U.S. Congress and certain state legislatures have introduced, considered or passed a large number of proposals and legislation affecting the healthcare system, including laws intended to impact access to health insurance.
The Affordable Care Act is the most prominent of these legislative reform efforts. The law affects how healthcare services are covered, delivered, and reimbursed, and expanded health insurance coverage through a combination of public program expansion and private sector health insurance reforms. In addition, some states have imposed individual health insurance mandates, and other states have explored or offer public health insurance options. To increase access to health insurance during the COVID-19 pandemic, the ARPA enhanced subsidies for individuals eligible to purchase coverage through Affordable Care Act marketplaces. Subsequent legislation extended these enhanced subsidies through 2025. These changes and initiatives may impact the number of individuals that elect to obtain public or private health insurance or the scope of such coverage, if purchased.
The Affordable Care Act has been, and continues to be, subject to legislative and regulatory changes and court challenges. There is uncertainty regarding whether, when, and how the Affordable Care Act will be further changed, whether the Affordable Care Act will be repealed or replaced, and how the Affordable Care Act will be interpreted and implemented. Changes to the interpretation or implementation of the Affordable Care Act could eliminate or alter provisions beneficial to us while leaving in place provisions reducing our reimbursement, or otherwise have an adverse effect on our business.
Other recent reform initiatives and proposals at the federal and state levels include those focused on price transparency and out-of-network charges, which may impact prices, our competitive position, patient volumes and the relationships between hospitals, patients, payors, and ancillary providers (such as anesthesiologists, radiologists, and pathologists). For example, among other consumer protections, the No Surprises Act imposes various requirements on providers and health plans intended to prevent “surprise” medical bills. The CMS Care Compare website makes publicly available certain data on hospital performance on quality measures and patient satisfaction. Further, Medicare reimbursement for hospitals is adjusted based on quality and efficiency measures.
There is also uncertainty regarding whether, when, and what other health reform measures will be adopted through governmental avenues and/or the private sector, the timing and implementation of any such efforts, and the impact of those efforts on providers as well as other healthcare industry participants. For example, some members of Congress have proposed measures that would expand government-funded coverage. CMS administrators may make changes to Medicaid payment models and grant states various flexibilities in the administration of state Medicaid programs, including changes encouraging the adoption of value-based care models. Some of these changes may result in coverage reductions or decreased enrollment. Reductions in the number of insured individuals or the scope of insurance coverage may have an adverse effect on our business. Other industry participants, such as private payors and large employer groups and their affiliates, may also introduce financial or delivery system reforms. It is difficult to predict the nature and/or success of current and future health reform initiatives, any of which may have an adverse impact on our business.
If we fail to comply with extensive laws and government regulations, including fraud and abuse laws, we could suffer penalties or be required to make significant changes to our operations.
The healthcare industry is governed by extensive and complex laws and regulations at the federal, state and local government levels. These laws and regulations include requirements related to, among other issues, licensure, certification, and enrollment with government programs; the necessity and adequacy of medical care; quality of medical equipment and services; qualifications of medical and support personnel; operating policies and procedures; screening, stabilization and transfer of individuals who have emergency medical conditions; restrictions on the provision of medical care, including with respect to reproductive care; distribution, maintenance and dispensing of pharmaceuticals and controlled substances; billing and coding for services; proper handling of overpayments; classification of levels of care provided; preparing and filing cost reports; relationships with referral sources and referral recipients; maintenance of adequate records; hospital use; rate-setting; building codes; environmental protection; privacy and security; interoperability and refraining from information blocking; development and use of artificial intelligence and other predictive algorithms; debt collection; limits or prohibitions on balance billing and billing for out-of-network services; and communications with patients and consumers. Examples of these laws include, but are not limited to, HIPAA, the Stark Law, the federal Anti-Kickback Statute, the federal False Claims Act, the EMTALA and similar state laws.
37
There are heightened coordinated civil and criminal enforcement efforts by both federal and state government agencies relating to the healthcare industry, including the hospital segment. Enforcement actions have focused on financial arrangements between hospitals and physicians, billing for services without adequately documenting medical necessity and billing for services outside the coverage guidelines for such services. Specific to our hospitals, we have received inquiries and subpoenas from various governmental agencies regarding these and other matters, and we are also subject to various claims and lawsuits relating to such matters. For a further discussion of these matters, see “Legal Proceedings” in Part I, Item 3 of this Form 10-K.
If we fail to comply with applicable laws and regulations, which are subject to change, we could be subject to liabilities, including civil penalties, money damages, the loss of our licenses to operate one or more facilities, exclusion of one or more facilities from participation in the Medicare, Medicaid and other federal and state healthcare programs, civil lawsuits and criminal penalties. The costs of compliance with, and the other burdens imposed by, these and other laws or regulatory actions may increase our operational costs, result in interruptions or delays in the availability of systems and/or result in a patient volume decline. We may also face audits or investigations by government agencies relating to our compliance with these regulations. An adverse outcome under any such investigation or audit could result in liability, result in adverse publicity, and adversely affect our business. In the future, evolving interpretations or enforcement of applicable laws or regulations could subject our current practices to allegations of impropriety or illegality or could require us to make changes in our facilities or operations. In addition, other legislation or regulations may be adopted that could adversely affect our business.
Actual or perceived failures to comply with legal requirements regarding the privacy and security of health information or other regulated, sensitive or confidential information, or legal requirements regarding data privacy or data protection, could adversely affect our business, results of operations and financial condition.
The data protection landscape is rapidly evolving, and we are subject to numerous state and federal laws, requirements and regulations governing the collection, use, storage, processing, disclosure, retention, privacy and security of health-related and other regulated, sensitive or confidential information, and may become subject to additional legal requirements of this nature in the future. For example, the Health Insurance Portability and Accountability Act of 1996, the Health Information Technology for Economic and Clinical Health Act of 2009, each as amended, and the privacy and security regulations that implement these laws (collectively, “HIPAA”), establish national privacy and security standards for the protection of protected health information, or PHI, by health plans, healthcare clearinghouses and certain healthcare providers, referred to as covered entities, and the business associates with whom such covered entities contract for services. HIPAA requires covered entities like us to develop and maintain policies and procedures with respect to the privacy and security of PHI and to adopt administrative, physical and technical safeguards to protect such information. HIPAA also regulates permissible uses and disclosures of PHI; for example, HHS issued guidance indicating certain data collected on websites and mobile applications offered by HIPAA-regulated entities may be PHI and warning against the use of third-party tracking technologies such as pixels and cookies on such sites. Covered entities must notify affected individuals without unreasonable delay of breaches of unsecured PHI, the HHS Office for Civil Rights, or OCR, which enforces HIPAA, and, in the case of larger breaches, the media. Failure to comply with the HIPAA privacy and security standards can result in civil monetary penalties, resolution agreements, monitoring agreements, and, in certain circumstances, criminal penalties including fines and/or imprisonment. A covered entity may be subject to penalties as a result of a business associate violating HIPAA. In addition, state attorneys general may enforce the HIPAA privacy and security regulations in response to violations that threaten the privacy of state residents. Although HIPAA does not create a private right of action allowing individuals to sue in civil court for violations, the laws and regulations have been used as the basis for duty of care in state civil suits such as those for negligence or recklessness in the misuse or breach of PHI.
There are numerous other laws and legislative and regulatory initiatives at the federal and state levels governing the confidentiality, privacy, availability, integrity and security of PHI and other types of personal information. Certain state laws may be more stringent, broader in scope or offer greater individual rights with respect to PHI than HIPAA, state laws may differ from each other, and the interplay of federal and state laws may be subject to varying interpretations by courts and government agencies, all of which may complicate compliance efforts. Where state laws are more protective than HIPAA or apply more broadly, we have to comply with their stricter provisions. Not only do some of these state laws impose fines and other penalties upon violators, but some may afford private rights of action to individuals who believe their personal information has been misused. We may not remain in compliance with diverse privacy and security requirements in all of the jurisdictions in which we do business, particularly to the extent they are inconsistent, rapidly changing and/or ambiguous and uncertain as to their applicability to our business practices.
To the extent we use, may use or permit the data we create, receive, maintain, and transmit to be used by any artificial intelligence, or AI, or machine learning, or ML, platforms, we may be subject to additional risks under health privacy and other laws and regulations. The regulatory framework for AI/ML, particularly in patient care (e.g., through the use of clinical decision support tools), is evolving and remains uncertain. For example, in December 2023, HHS finalized transparency requirements for AI and other predictive algorithms used in certified health information technology, such as decision support interventions. New laws, regulations, and policies may be adopted, including as a result of a recent executive order on AI, and existing laws and regulations may be interpreted in new ways that would affect our operations and the ways in which we may use AI technology. If we are unable to use
38
AI/ML as the result of such laws and regulations, regulators restrict our ability to use AI/ML for certain purposes or our confidential information becomes part of a dataset that is accessible by other third-party AI/ML applications and uses, it could make our business less efficient, result in competitive disadvantages, increase our operating costs, hinder our ability to provide services, and subject us to potential liabilities. Further, the cost to comply with such laws and regulations could be significant and could adversely affect our business, financial condition and results of operations. Any failure or perceived failure by us to comply with AI laws and regulations could result in proceedings, investigations or actions against us by individuals, consumer rights groups, government agencies or others. We could incur significant costs in investigating and defending such claims and, if found liable, pay significant damages or fines or be required to make changes to our technology and business. Further, to the extent that we rely on or use the output of AI/ML, any inaccuracies, biases or errors could hinder our ability to provide services and otherwise have adverse impacts on us, our business, our results of operations or financial condition. Further, any such proceedings and any subsequent adverse outcomes may subject us to significant negative publicity. While the full impact of regulatory and legal risks associated with AI/ML is unknown, if any of these events were to occur, our business, results of operations and financial condition could be materially adversely affected.
In addition, we are subject to consumer protection laws and regulations in connection with our business activities. For example, the FTC uses its consumer protection authority to initiate enforcement actions in response to data breaches. Failing to take appropriate steps to keep consumers’ personal information secure may violate the Federal Trade Commission Act, or the FTCA. For information that is not subject to HIPAA and deemed to be “personal health records,” the FTC may also impose penalties for violations of the Health Breach Notification Rule, or HBNR, to the extent we are considered a “personal health record-related entity” or “third party service provider.” The FTC has recently taken several enforcement actions under HBNR and indicated that the FTC will continue to protect consumer privacy through greater use of the agency’s enforcement authorities. As a result, we expect scrutiny by federal and state regulators and others of our collection, use and disclosure of health information. Additionally, federal and state consumer protection laws are increasingly being applied by FTC and states’ attorneys general to regulate the collection, use, storage, and disclosure of personal or personally identifiable information, through websites or otherwise, and to regulate the presentation of website content. Our marketing and patient engagement activities are subject to communications laws such as the Telephone Consumer Protection Act, or the TCPA, and the Controlling the Assault of Non-Solicited Pornography and Marketing Act, or CAN-SPAM. Determination by a court or regulatory agency that our calling, texting or email practices violate the TCPA or CAN-SPAM could subject us to civil penalties and could require us to change some portions of our business. Even an unsuccessful challenge by patients or regulatory authorities of our activities could result in adverse publicity and could require a costly response from and defense by us.
Other federal and state laws that restrict the use and protect the privacy and security of personally identifiable information may not be preempted by HIPAA, may apply to new categories of health information, such as “consumer health data”, and may be subject to varying interpretations by the courts and government agencies. These varying interpretations can create complex compliance issues for us and our partners and potentially expose us to additional expense, adverse publicity, and liability, any of which could adversely affect our business.
Although we strive to comply with applicable laws and regulations, the requirements related to the collection, use, storage, processing, disclosure, retention, privacy and security of health and other regulated, sensitive or confidential information are evolving rapidly and may be interpreted or applied in an inconsistent manner across jurisdictions. The cost of compliance with these laws and regulations is high and is likely to increase in the future. Any failure or perceived failure by us to comply with applicable data privacy and security laws or regulations, our internal policies and procedures or our contracts governing our processing of health and other regulated, sensitive or confidential information, or to otherwise adequately address privacy and security concerns, could result in negative publicity, government investigations and enforcement actions, claims by third parties and damage to our reputation, any of which could have a material adverse effect on our business, operations, or financial results.
Healthcare technology initiatives, particularly those related to sharing patient data and interoperability, may adversely affect our business and results of operations.
Under the Health Information Technology for Economic and Clinical Health Act, or HITECH, and other laws, eligible hospitals that fail to demonstrate meaningful use of certified EHR technology and have not applied and qualified for a hardship exception are subject to reduced reimbursement from Medicare. Eligible healthcare professionals are also subject to positive or negative payment adjustments based, in part, on their use of EHR technology. Thus, if our hospitals and employed professionals are unable to properly adopt, maintain, and utilize certified EHR systems, we could be subject to penalties and lawsuits that may have an adverse effect on our consolidated financial position and consolidated results of operations.
39
As EHR technologies have become widespread, the federal government’s focus has shifted to increasing patient access to healthcare data and promoting interoperability. The 21st Century Cures Act and implementing regulations prohibit information blocking by healthcare providers and certain other entities. Information blocking is defined as engaging in activities that are likely to interfere with the access, exchange or use of electronic health information, subject to limited exceptions. Current and future initiatives related to healthcare technology (including AI/ML), data sharing, and interoperability may require changes to our operations, impose new and complex obligations on us, affect our relationships with providers, vendors, healthcare information exchanges and other third parties and require investments in infrastructure. We may be subject to significant penalties or other disincentives or experience reputational damage for failure to comply with applicable laws and regulations. It is difficult to predict how these initiatives will affect our relationships with providers and vendors, participation in healthcare information exchanges or networks, the exchange of patient data and patient engagement.
State efforts to regulate the construction, acquisition or expansion of healthcare facilities could limit our ability to build or acquire additional healthcare facilities, renovate our facilities or expand the breadth of services we offer.
Some states in which we operate require a CON or other prior approval for the construction or acquisition of healthcare facilities, capital expenditures exceeding a prescribed amount, changes in bed capacity or services and some other matters. In evaluating a proposal, these states consider the need for additional or expanded healthcare facilities or services. If we are not able to obtain required CONs or other prior approvals, we will not be able to acquire, operate, replace or expand our facilities or expand the breadth of services we offer. Furthermore, if a CON or other prior approval upon which we relied to invest in construction of a replacement or expanded facility were to be lost through an appeal process or revoked, we may not be able to recover the value of our investment.
Many states have adopted legislation regarding the sale or other disposition of hospitals operated by municipal or not-for-profit entities. In some states that do not have specific legislation, the attorneys general have demonstrated an interest in these transactions under their general obligation to protect the use of charitable assets. These legislative and administrative efforts focus primarily on the appropriate valuation of the assets divested and the use of the proceeds of the sale by the non-profit seller. In addition, some states require for-profit entities, including hospitals, to notify state attorneys general or other designated entities in advance of sales or other transactions. While these notice requirements, reviews and, in some instances, approval processes can add additional time to the closing of a hospital acquisition, we have not yet had any significant difficulties or delays in completing acquisitions. However, if we encounter delays when we seek to acquire hospitals or a state prohibits a transaction, these restrictions could have a negative impact on our business and growth plans.
We may incur additional tax liabilities.
We are subject to tax in the United States as well as those states in which we do business. Changes in tax laws, including increased rates, or interpretations of tax laws by taxing authorities or other standard setting bodies, could increase our tax obligations and materially and adversely impact our results of operations.
Risks Related to Impairment
If the fair value of our reporting unit declines, a material non-cash charge to earnings from impairment of our goodwill could result.
On an ongoing basis, under U.S. GAAP, we evaluate, based on the fair value of our reporting unit, whether the carrying value of our goodwill is impaired when events or changes in circumstances indicate that such carrying value may not be recoverable. Goodwill is evaluated for impairment annually and when an event occurs or circumstances change that, more likely than not, reduce the fair value of the reporting unit below its carrying value.
In assessing the fair value of this reporting unit, we consider, among other things, the most recent price of our common stock and fair value of our long-term debt, our recent financial results, estimates of future revenue and expense growth, estimated market multiples, expected capital expenditures, income tax rates, costs of invested capital and a discount rate. We performed our last annual goodwill impairment evaluation during the fourth quarter of 2023 using the October 31, 2023 measurement date, which indicated no impairment.
We could record material impairment charges in the future if our estimates or assumptions with respect to such fair value determination change in the future. In this regard, we recorded material non-cash impairment charges with respect to our hospital operations reporting unit in 2016 and 2017.
40
A significant decline in operating results or other indicators of impairment at one or more of our facilities could result in a material non-cash charge to earnings to impair the value of long-lived assets.
Our operations are capital intensive and require significant investment in long-lived assets, such as property, equipment and other long-lived intangible assets, including capitalized internal-use software. If one of our facilities experiences declining operating results or is adversely impacted by one or more of these risk factors, we may not be able to recover the carrying value of those assets through our future operating cash flows. On an ongoing basis, we evaluate whether changes in future undiscounted cash flows reflect an impairment in the fair value of our long-lived assets. Additionally, if we decide to sell a business, we evaluate whether a business or a group of businesses is impaired based on an analysis of the selling price from a definitive agreement compared to the carrying value of the net assets being sold. If the carrying value of our long-lived assets is impaired, we may incur a material non-cash charge to earnings.
Risks Related to Cybersecurity and Technology
Our operations could be significantly impacted by interruptions or restrictions in access to our information systems.
Our operations depend heavily on the proper function, availability and security of our information systems, as well as those of our third-party providers, to collect, maintain, process and use sensitive data and other clinical, operational and financial information. Information systems require an ongoing commitment of significant resources to maintain and enhance existing systems and to develop new systems in order to keep pace with continual changes in information technology. Failure to adequately manage implementation of new technology, updates or enhancements of platforms or interfaces between platforms could place us at a competitive disadvantage, disrupt our operations, and have a material, adverse impact on our business and results of operations. Further, we may be adversely impacted by costs associated with new and expensive technology. In addition, we rely on third-party providers of financial, clinical, patient accounting and network information services, including those that interface with our own systems, and, as a result, we face operational challenges in maintaining multiple provider platforms and facilitating the interface of such systems with one another. We rely on these third-party providers to have appropriate controls to protect confidential information and other sensitive or regulated data. While we take steps to require third-party providers to protect confidential information and sensitive data, we do not control the information systems of third-party providers, and in some cases we may have difficulty accessing information archived on third-party systems.
Our networks and information systems, and the networks and information systems of third parties that we rely upon, are also subject to disruption due to events such as a major earthquake, natural disaster, fire, telecommunications failure, power outages, new system implementations, computer viruses, ransomware or other malware, security breaches, cyber-attacks (including ransomware), human errors (such as inadvertent misuse by employees), acts of war, terrorist or criminal activities or other catastrophic events. Disaster recovery planning, whether conducted by us or a third party, cannot account for all eventualities, and may not be sufficient to mitigate against or recover from such events. If the information systems on which we rely fail or are interrupted or if our access to these systems is limited in the future, or if we experience data loss or manipulation, it could result in unauthorized disclosure, misuse, loss or alteration of such data, interruptions and delays in our normal business operations, potential liability under applicable laws, regulatory penalties, and damage to our reputation. Any of these could have an adverse effect on our business, financial condition or results of operations.
A cyber-attack or security breach could result in the compromise of our facilities, confidential data or critical data systems and give rise to potential harm to patients, remediation and other expenses, expose us to liability under HIPAA, privacy and data protection laws and regulations, consumer protection laws, common law or other theories, subject us to litigation and federal and state governmental inquiries or actions, damage our reputation, adversely impact our financial results and otherwise be disruptive to our business.
We rely extensively on information technology systems to manage clinical and financial data, to communicate with our patients, payors, vendors and other third parties, to summarize and analyze operating results, and for a number of other critical operational functions. We have made significant investments in technology to protect our systems, equipment and medical devices and information from cybersecurity risks. These risks include incidents involving ransomware and other malicious software, phishing, or other attempts by third parties to access, acquire, use, disclose, misappropriate or manipulate our information or disrupt our operations. Although we monitor and routinely test our security systems and processes and have redundancies as well as other proactive measures designed to protect the integrity, security and availability of the systems and data we manage and control, there can be no assurance that we, or our third-party vendors and providers, will not be subject to security breaches and other cybersecurity incidents. In this regard, we are frequently the target of cybersecurity attacks and other threats that could have a security impact, and we have experienced cybersecurity incidents from time to time. In particular, on February 13, 2023, we disclosed a security incident in which a third-party vendor who provides a secure file transfer software platform utilized by our subsidiaries experienced a security
41
breach whereby PHI and personal information of certain patients of our healthcare facilities were exposed to an unauthorized third party.
The current cyber threat environment presents increased risk for all companies, particularly companies in the healthcare industry, as the volume and intensity of cyber-attacks on hospitals and health systems has continued to increase, and we expect to experience an increase in cybersecurity threats in the future. Moreover, advanced new attacks against our information systems and devices or those of our third-party vendors create risk of cybersecurity incidents, including ransomware, malware and phishing incidents. The preventive actions we take to reduce the risk of such incidents and protect our systems and data may not be sufficient in the future. In addition, cybersecurity threats continue to evolve. For example, remote code execution vulnerabilities in certain applications have presented a new attack vector for potential malicious attackers. Additionally, the rapid evaluation and increased adoption of artificial intelligence technologies may heighten our cybersecurity risks by making cyber-attacks more difficult to detect, contain and mitigate. Because the techniques used in cyber-attacks change frequently and may not be immediately recognized, we may experience security or data breaches that remain undetected for an extended time. Cybersecurity and the continued development and enhancement of our controls, process and practices designed to protect our information systems from attack, damage or unauthorized access, acquisition, use or disclosure remain a priority for us. Our ability to recover from a ransomware or other cyber-attack is dependent on these practices, including successful backup systems and other recovery procedures. We may be required to expend significant additional resources to continue to modify or enhance our protective measures or to investigate and remediate any information security vulnerabilities, and we still might not be able to anticipate or prevent certain attack methods.
Further, cybersecurity threats, including those that result in a data or security breach, could impact the integrity, availability or security of PHI and other data subject to privacy laws and regulations, disrupt our information technology systems, equipment, medical devices or business, and threaten the access and utilization of critical information technology and data. Our ability to provide various healthcare services could be affected, particularly with respect to telehealth services. In addition, medical devices that connect to hospital networks or the internet may be vulnerable to cybersecurity incidents, which may impact patient safety.
We may be at increased risk because we outsource certain services or functions to, or have systems that interface with, third parties. Some of these third parties’ information systems are also subject to the risks outlined above and may store or have access to our data and may not have effective controls, processes, or practices to protect our information from attack, damage, or unauthorized access, acquisition, use or disclosure. A breach or attack affecting any of these third parties could harm our business. In addition, the definitive agreements we enter into in connection with the divestiture of hospitals routinely obligate us to provide transition services to the buyer, including access to our legacy information systems, for a defined transition period. By providing access to our information systems to non-employees, we may be exposed to cyber-attacks, ransomware or security or data breaches that originate outside of our internal processes and practices designed to prevent such threats from occurring. Further, consumer confidence in the integrity, availability and confidentiality of information systems and information, including patient information and operations data, in the healthcare industry generally could be impacted to the extent there are successful cyber-attacks at other healthcare services companies, which could have a material adverse effect on our business, operations, or financial results.
If we or our information, systems are subject to cyber-attacks or security or data breaches in the future, or the information systems of third parties with whom we conduct business are subject to cyber-attacks or security or data breaches in the future in a manner which impacts us or our information systems, this could result in harm to patients; business and operational interruptions and delays; the loss, misappropriation, corruption or unauthorized access, acquisition, use or disclosure of data or inability to access data; litigation and potential liability under privacy, security, breach notification and consumer protection laws or other applicable laws, including HIPAA; reputational damage, federal and state governmental inquiries, civil monetary penalties, settlement agreements, corrective action plans and monitoring requirements, any of which could have an adverse effect on our business, financial condition or results of operations. Moreover, any significant cybersecurity event may require us to devote significant management time and resources to address and respond to any such event, interfere with the pursuit of other important business strategies and initiatives, and cause us to incur additional expenditures, which could be material, including to investigate such events, remedy cybersecurity problems, recover lost data, prevent future compromises and adapt systems and practices in response to such events. Moreover, there is no assurance that any remedial actions will meaningfully limit the success of future attempts to breach our information systems, particularly because malicious actors are increasingly sophisticated and utilize tools and techniques specifically designed to circumvent security measures, avoid detection and obfuscate forensic evidence, which means we may be unable to identify, investigate or remediate effectively or in a timely manner.
Additionally, while we have insurance coverage in place designed to address certain aspects of cybersecurity risks, such insurance coverage may be insufficient to cover all losses or all types of claims that may arise.
42
If we fail to comply with our obligations under license or technology agreements with third parties, we may be required to pay damages and we could lose license rights that are critical to our business.
We license certain intellectual property, including technologies and software from third parties, that is important to our business, and in the future we may enter into additional agreements that provide us with licenses to valuable intellectual property or technology. If we fail to comply with any of the obligations under our license agreements, we may be required to pay damages and the licensor may have the right to terminate the license. Termination by the licensor would cause us to lose valuable rights, and could prevent us from selling our solutions and services, or adversely impact our ability to commercialize future solutions and services. Our business would suffer if any current or future licenses terminate, if the licensors fail to abide by the terms of the license agreement, if the licensors fail to enforce licensed intellectual property against infringing third parties, if the licensed intellectual property are found to be invalid or unenforceable, or if we are unable to enter into necessary license agreements on acceptable terms or at all. Any of the foregoing could have an adverse effect on our business, financial condition or results of operations.
If the redesign and consolidation of key business functions, including through the implementation of a core enterprise resource planning system, or ERP, does not proceed as expected or is not completed successfully, our business and financial results may be adversely impacted.
We have undertaken a transformative process of redesigning numerous workflows that is intended to modernize and consolidate our technology platforms and associated processes across our organization. As part of this process, we have created and continue to expand shared business operations to carry out certain financial and operational functions, and are implementing a new ERP. Implementation of individual modules of the ERP and other aspects of this process, which began in the fourth quarter of 2023, are expected to occur over a multi-year period. The redesign of various business processes and implementation of this ERP and other aspects of this transformative process requires an investment of significant personnel and financial resources, including substantial expenditures for third-party consultants and system hardware and software. This implementation process could disrupt our operations or otherwise adversely affect us, including as the result of delays, disruptions to business continuity, higher than anticipated expenditures, potential design defects, data migration issues, diversion of management’s attention from other key priorities, increased cybersecurity risks and adverse impacts on the effectiveness of our internal controls over financial reporting. If we are unable to complete this redesign and consolidation of key business functions, including the implementation of the ERP, effectively, on a timely basis, or at all, our financial position, results of operations and cash flows may be adversely affected. Moreover, there is no assurance that this new ERP and other aspects of this process, once implemented, will meet our current or future business needs or will operate as intended.
43
Item 1B. Unresolved Staff Comments
None
Item 1C. Cybersecurity
Risk Management
We place the utmost importance on information security and privacy, including protecting the personal medical, financial and insurance information of our patients and employees, and have a cybersecurity risk management program designed to assess, identify and manage material risks from cybersecurity threats. Our cybersecurity risk management program is designed to employ industry best practices across our operations and business functions, including through monitoring and assessing our threat environment; vulnerability assessments; detecting and responding to cyber attacks, cybersecurity incidents, and data breaches; cybersecurity crisis preparedness and incident response plans; and investments in cybersecurity infrastructure and technology intended to reduce cybersecurity risk. Key aspects of our cybersecurity risk management program include the following:
We engage consulting firms and other third parties in connection with our cybersecurity risk management processes. For example, third parties are engaged from time to time to conduct evaluations of our security controls, including penetration testing and independent audits, and to advise the Board of Directors, the Audit and Compliance Committee of the Board of Directors and/or our management team regarding cybersecurity matters.
We have processes to oversee and identify material cybersecurity risks associated with our use of third-party service providers. As part of these processes, we conduct cybersecurity due diligence where deemed advisable with respect to third-party service providers that will be accessing our information technology systems, including access to view or store sensitive data, prior to their engagement. Moreover, we have processes designed to oversee and identify material cybersecurity risks associated with the information systems of third-party service providers. In addition, third-party service providers that have access to our information technology systems, including access to view or store sensitive data, are contractually obligated to report cybersecurity incidents to us so that we can assess the impact of any such incident on our business.
The current cyber threat environment presents increased risk for all companies, particularly companies in our industry, as the volume and intensity of cybersecurity attacks on hospitals and health systems has continued to increase. We are regularly the target of cybersecurity attacks and other threats that could have a security impact, and we have experienced security incidents from time to time. In particular, on February 13, 2023, we disclosed a security breach in which a third-party vendor that provides a secure file transfer software platform utilized by our subsidiaries experienced a security breach whereby personal information of certain patients of our healthcare facilities were exposed to the attacker.
We do not believe that risks we have identified to date from cybersecurity threats, including as a result of any previous cybersecurity incidents, have materially affected or are reasonably likely to materially affect us, including our business strategy, results of operations or financial condition. However, despite our security measures, there is no assurance that we, or the third parties with which we interact, will not experience a cybersecurity incident in the future that materially affects us. For additional information regarding the risks to us associated with cybersecurity incidents, see “A cyber-attack or security breach could result in the compromise of our facilities, confidential data or critical data systems and give rise to potential harm to patients, remediation and
44
other expenses, expose us to liability under HIPAA, privacy and data protection laws and regulations, consumer protection laws, common law or other theories, subject us to litigation and federal and state governmental inquiries and actions, damage our reputation, adversely impact our financial results and otherwise be disruptive to our business.” included in Part I, Item 1A of this Form 10-K.
We maintain a cybersecurity insurance policy that provides coverage in connection with cybersecurity incidents. However, costs and damages associated with cybersecurity incidents may not be fully insured under our insurance policy, and (to the extent otherwise covered) are subject to applicable deductibles.
Governance
Our cybersecurity risk management processes are integrated into our overall risk management system. Our Board of Directors is responsible for the overall supervision of our risk management activities. The Board's oversight of the material risks faced by us occurs at both the full board level and at the committee level. In addition, the Audit and Compliance Committee has primary oversight responsibility regarding our information security, data security, data privacy, and other cybersecurity programs, procedures and risks. Further, the Audit and Compliance Committee and our Board of Directors receive updates at least quarterly from management, including our Chief Information Security Officer, or the CISO, covering our programs for managing cybersecurity risks, including data privacy and data protection risks. Additionally, the Audit and Compliance Committee and the Board of Directors actively participate in discussions with management and among themselves regarding cybersecurity risks.
Risk management is administered at a management level through a multi-disciplinary Enterprise Risk Committee comprised of members of management, including our CISO. The Enterprise Risk Committee identifies and monitors what we believe to be the key risks currently facing the organization, including cybersecurity risks. A comprehensive presentation regarding our enterprise risk management process and our key risks is presented to the full Board of Directors on an annual basis.
In addition, we have established a Cyber Risk Executive Steering Committee, a multi-disciplinary management-level team chaired by our CISO which is responsible for assessing and overseeing our information security and cybersecurity risk management policies, practices and priorities and for assessing and monitoring key cybersecurity risks with respect to reporting such risks within the organization.
At a management level, our cybersecurity risk management efforts are led by our CISO. Our current CISO was appointed as our Vice President and Chief Information Security Officer in 2021. Our current CISO has expertise in cybersecurity risk management through his more than 25 years of experience in cybersecurity, technology and data privacy roles, including his service with the Company since 2021 and his service as chief information security officer at another large organization prior to being employed by us. In addition, other individuals on our IT security team have cybersecurity experience or certifications relevant to their respective role.
A key component of our enterprise risk management program is our incident response plan, which provides for controls and procedures in connection with cybersecurity incidents. Under this plan, we have established a cybersecurity incident command, a multi-disciplinary management-level team led by the CISO. The plan provides that the incident response team will conduct an initial assessment in the event of a cybersecurity incident meeting certain criteria elevated for the review of senior members of the IT security team. In such event, the plan provides that the incident response team will assess whether a cybersecurity incident has the potential to materially impact the organization and whether public disclosure is required or advisable in connection therewith, and further provides that, if appropriate, any such cybersecurity incident may be further elevated for the review of senior management, the Audit and Compliance Committee and/or the Board of Directors.
Item 2. Properties
We own our corporate headquarters building located in Franklin, Tennessee. In addition to the headquarters in Franklin, we maintain regional service centers related to certain of our shared services initiatives. These service centers are located near our corporate headquarters or in the markets in which we operate hospitals.
Most of our hospitals are general care hospitals offering a wide range of inpatient and outpatient medical services. These services generally include general acute care, emergency room, general and specialty surgery, critical care, internal medicine, obstetrics, diagnostic, psychiatric and rehabilitation services. In addition, some of our hospitals provide skilled nursing and home care services based on individual community needs.
For each of our hospitals owned or leased as of December 31, 2023, the following table shows its location, the date of its acquisition or lease inception and the number of licensed beds:
45
Hospital |
|
City |
|
Licensed |
|
|
Date of |
|
Ownership |
|
Alabama |
|
|
|
|
|
|
|
|
|
|
South Baldwin Regional Medical Center |
|
Foley |
|
|
112 |
|
|
June, 2000 |
|
Leased |
Grandview Medical Center |
|
Birmingham |
|
|
434 |
|
|
July, 2007 |
|
Owned |
Flowers Hospital |
|
Dothan |
|
|
235 |
|
|
July, 2007 |
|
Owned |
Medical Center Enterprise |
|
Enterprise |
|
|
131 |
|
|
July, 2007 |
|
Owned |
Gadsden Regional Medical Center |
|
Gadsden |
|
|
346 |
|
|
July, 2007 |
|
Owned |
Crestwood Medical Center |
|
Huntsville |
|
|
180 |
|
|
July, 2007 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
Alaska |
|
|
|
|
|
|
|
|
|
|
Mat-Su Regional Medical Center |
|
Palmer |
|
|
125 |
|
|
July, 2007 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
Arizona |
|
|
|
|
|
|
|
|
|
|
Western Arizona Regional Medical Center |
|
Bullhead City |
|
|
139 |
|
|
July, 2000 |
|
Owned |
Northwest Medical Center |
|
Tucson |
|
|
287 |
|
|
July, 2007 |
|
Owned |
Oro Valley Hospital |
|
Oro Valley |
|
|
176 |
|
|
July, 2007 |
|
Owned |
Northwest Medical Center Sahuarita |
|
Sahuarita |
|
|
18 |
|
|
November, 2020 |
|
Owned |
Northwest Medical Center Houghton |
|
Houghton |
|
|
44 |
|
|
June, 2022 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
Arkansas |
|
|
|
|
|
|
|
|
|
|
Northwest Health System |
|
|
|
|
|
|
|
|
|
|
Northwest Medical Center - Bentonville |
|
Bentonville |
|
|
128 |
|
|
July, 2007 |
|
Owned |
Northwest Medical Center - Springdale |
|
Springdale |
|
|
222 |
|
|
July, 2007 |
|
Owned |
Willow Creek Women’s Hospital |
|
Johnson |
|
|
64 |
|
|
July, 2007 |
|
Owned |
Northwest Health Physician’s Specialty Hospital |
|
Fayetteville |
|
|
20 |
|
|
April, 2016 |
|
Leased |
Siloam Springs Regional Hospital |
|
Siloam Springs |
|
|
73 |
|
|
February, 2009 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
Florida |
|
|
|
|
|
|
|
|
|
|
North Okaloosa Medical Center |
|
Crestview |
|
|
110 |
|
|
March, 1996 |
|
Owned |
Shorepoint Health Port Charlotte |
|
Port Charlotte |
|
|
254 |
|
|
January, 2014 |
|
Owned |
Shorepoint Health Punta Gorda |
|
Punta Gorda |
|
|
208 |
|
|
January, 2014 |
|
Owned |
Lower Keys Medical Center |
|
Key West |
|
|
167 |
|
|
January, 2014 |
|
Leased |
Physicians Regional Healthcare System - Collier |
|
Naples |
|
|
130 |
|
|
January, 2014 |
|
Owned |
Physicians Regional Healthcare System - Pine Ridge |
|
Naples |
|
|
227 |
|
|
January, 2014 |
|
Owned |
Santa Rosa Medical Center |
|
Milton |
|
|
129 |
|
|
January, 2014 |
|
Leased |
|
|
|
|
|
|
|
|
|
|
|
Georgia |
|
|
|
|
|
|
|
|
|
|
East Georgia Regional Medical Center |
|
Statesboro |
|
|
149 |
|
|
January, 2014 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
Indiana |
|
|
|
|
|
|
|
|
|
|
Lutheran Health Network |
|
|
|
|
|
|
|
|
|
|
Bluffton Regional Medical Center |
|
Bluffton |
|
|
40 |
|
|
July, 2007 |
|
Owned |
Dupont Hospital |
|
Fort Wayne |
|
|
131 |
|
|
July, 2007 |
|
Owned |
Lutheran Hospital |
|
Fort Wayne |
|
|
396 |
|
|
July, 2007 |
|
Owned |
Lutheran Musculoskeletal Center |
|
Fort Wayne |
|
|
37 |
|
|
July, 2007 |
|
Owned |
Lutheran Downtown Hospital |
|
Fort Wayne |
|
|
191 |
|
|
July, 2007 |
|
Owned |
Dukes Memorial Hospital |
|
Peru |
|
|
25 |
|
|
July, 2007 |
|
Owned |
Kosciusko Community Hospital |
|
Warsaw |
|
|
72 |
|
|
July, 2007 |
|
Owned |
Northwest Health - Porter Hospital |
|
Valparaiso |
|
|
301 |
|
|
May, 2007 |
|
Owned |
Northwest Health - La Porte Hospital |
|
La Porte |
|
|
227 |
|
|
March, 2016 |
|
Owned |
Northwest Health - Starke Hospital |
|
Knox |
|
|
53 |
|
|
March, 2016 |
|
Leased |
|
|
|
|
|
|
|
|
|
|
|
Mississippi |
|
|
|
|
|
|
|
|
|
|
Merit Health Wesley |
|
Hattiesburg |
|
|
211 |
|
|
July, 2007 |
|
Owned |
Merit Health River Region |
|
Vicksburg |
|
|
351 |
|
|
July, 2007 |
|
Owned |
Merit Health Biloxi |
|
Biloxi |
|
|
153 |
|
|
January, 2014 |
|
Leased |
46
Merit Health Central |
|
Jackson |
|
|
379 |
|
|
January, 2014 |
|
Leased |
Merit Health Rankin |
|
Brandon |
|
|
134 |
|
|
January, 2014 |
|
Leased |
Merit Health Madison |
|
Canton |
|
|
67 |
|
|
January, 2014 |
|
Owned |
Merit Health River Oaks |
|
Flowood |
|
|
160 |
|
|
January, 2014 |
|
Owned |
Merit Health Woman's Hospital |
|
Flowood |
|
|
109 |
|
|
January, 2014 |
|
Owned |
Merit Health Natchez |
|
Natchez |
|
|
179 |
|
|
October, 2014 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
Missouri |
|
|
|
|
|
|
|
|
|
|
Moberly Regional Medical Center |
|
Moberly |
|
|
99 |
|
|
November, 1993 |
|
Owned |
Northeast Regional Medical Center |
|
Kirksville |
|
|
93 |
|
|
December, 2000 |
|
Leased |
Poplar Bluff Regional Medical Center |
|
Poplar Bluff |
|
|
410 |
|
|
January, 2014 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
New Mexico |
|
|
|
|
|
|
|
|
|
|
Eastern New Mexico Medical Center |
|
Roswell |
|
|
162 |
|
|
April, 1998 |
|
Owned |
Carlsbad Medical Center |
|
Carlsbad |
|
|
99 |
|
|
July, 2007 |
|
Owned |
Mountain View Regional Medical Center |
|
Las Cruces |
|
|
168 |
|
|
July, 2007 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
North Carolina |
|
|
|
|
|
|
|
|
|
|
Lake Norman Regional Medical Center |
|
Mooresville |
|
|
123 |
|
|
January, 2014 |
|
Owned |
Davis Regional Medical Center |
|
Statesville |
|
|
144 |
|
|
January, 2014 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
Oklahoma |
|
|
|
|
|
|
|
|
|
|
AllianceHealth Madill |
|
Madill |
|
|
25 |
|
|
January, 2014 |
|
Leased |
AllianceHealth Durant |
|
Durant |
|
|
138 |
|
|
January, 2014 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
Pennsylvania |
|
|
|
|
|
|
|
|
|
|
Commonwealth Health Network |
|
|
|
|
|
|
|
|
|
|
Wilkes-Barre General Hospital |
|
Wilkes-Barre |
|
|
369 |
|
|
April, 2009 |
|
Owned |
Regional Hospital of Scranton |
|
Scranton |
|
|
186 |
|
|
May, 2011 |
|
Owned |
Moses Taylor Hospital |
|
Scranton |
|
|
122 |
|
|
January, 2012 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
Tennessee |
|
|
|
|
|
|
|
|
|
|
Tennova Healthcare - Cleveland |
|
Cleveland |
|
|
351 |
|
|
October, 2005 |
|
Owned |
Tennova Healthcare - Clarksville |
|
Clarksville |
|
|
270 |
|
|
July, 2007 |
|
Owned |
Tennova - Jefferson Memorial Hospital |
|
Jefferson City |
|
|
58 |
|
|
January, 2014 |
|
Leased |
Tennova - LaFollette Medical Center |
|
LaFollette |
|
|
66 |
|
|
January, 2014 |
|
Owned |
Tennova - Newport Medical Center |
|
Newport |
|
|
130 |
|
|
January, 2014 |
|
Owned |
Tennova - North Knoxville Medical Center |
|
Powell |
|
|
116 |
|
|
January, 2014 |
|
Owned |
Tennova - Turkey Creek Medical Center |
|
Knoxville |
|
|
111 |
|
|
January, 2014 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
Texas |
|
|
|
|
|
|
|
|
|
|
Lake Granbury Medical Center |
|
Granbury |
|
|
73 |
|
|
January, 1997 |
|
Leased |
Laredo Medical Center |
|
Laredo |
|
|
326 |
|
|
October, 2003 |
|
Owned |
Navarro Regional Hospital |
|
Corsicana |
|
|
162 |
|
|
July, 2007 |
|
Owned |
Longview Regional Medical Center |
|
Longview |
|
|
224 |
|
|
July, 2007 |
|
Owned |
Woodland Heights Medical Center |
|
Lufkin |
|
|
149 |
|
|
July, 2007 |
|
Owned |
DeTar Healthcare System |
|
Victoria |
|
|
278 |
|
|
July, 2007 |
|
Owned |
Cedar Park Regional Medical Center |
|
Cedar Park |
|
|
126 |
|
|
December, 2007 |
|
Owned |
|
|
|
|
|
|
|
|
|
|
|
Total Licensed Beds at December 31, 2023 |
|
|
|
|
11,902 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Total Hospitals at December 31, 2023 |
|
|
|
|
71 |
|
|
|
|
|
The real property of substantially all of our wholly-owned hospitals is also encumbered by mortgages to support obligations under the ABL Facility and outstanding senior secured notes.
47
Item 3. Legal Proceedings
From time to time, we receive inquiries or subpoenas from state regulators, state Medicaid Fraud Control units, fiscal intermediaries, CMS, the U.S. Department of Justice and other government entities regarding various Medicare and Medicaid issues. In addition, we are subject to other claims and lawsuits arising in the ordinary course of our business including lawsuits and claims related to billing and collection practices at our hospitals. Based on current knowledge, management does not believe that loss contingencies arising from pending legal, regulatory and governmental matters, including the matters described herein, will have a material adverse effect on the consolidated financial position or liquidity of the Company. However, in light of the inherent uncertainties involved in pending legal, regulatory and governmental matters, some of which are beyond our control, and the very large or indeterminate damages sought in some of these matters, an adverse outcome in one or more of these matters could be material to our results of operations or cash flows for any particular reporting period. Settlements of suits involving Medicare and Medicaid issues routinely require both monetary payments as well as corporate integrity agreements. Additionally, qui tam or “whistleblower” actions initiated under the FCA may be pending but placed under seal by the court to comply with the FCA’s requirements for filing such suits. In September 2014, the Criminal Division of the U.S. Department of Justice announced that all qui tam cases will be shared with their Division to determine if a parallel criminal investigation should be opened. The Criminal Division has also frequently stated an intention to pursue corporations in criminal prosecutions, including in its most recent Memorandum dated September 15, 2022. From time to time, we detect issues of non-compliance with Federal healthcare laws pertaining to claims submission and reimbursement practices and/or financial relationships with physicians. We avail ourselves of various mechanisms to address potential overpayments arising out of these issues, including repayment of claims, rebilling of claims, and participation in voluntary disclosure protocols offered by CMS and the Office of Inspector General. Participating in voluntary repayments and voluntary disclosure protocols can have the potential for significant settlement obligations or even enforcement action.
The following legal proceedings are described in detail because, although certain legal proceedings may not be required to be disclosed in this Part I, Item 3 under SEC rules, due to the nature of the business of the Company, we believe that the following discussion of these matters may provide useful information to security holders. This discussion does not include claims and lawsuits covered by medical professional liability, general liability or employment practices insurance and risk retention programs, none of which claims or lawsuits would in any event be required to be disclosed in this Part I, Item 3 under SEC rules.
Shareholder Litigation
Caleb Padilla, individually and on behalf of all others similarly situated v. Community Health Systems, Inc., Wayne T. Smith, Larry Cash, and Thomas J. Aaron. This purported federal securities class action was filed in the United States District Court for the Middle District of Tennessee on May 30, 2019. It seeks class certification on behalf of purchasers of our common stock between February 20, 2017 and February 27, 2018 and alleges misleading statements resulted in artificially inflated prices for our common stock. On November 20, 2019, the District Court appointed Arun Bhattacharya and Michael Gaviria as lead plaintiffs in the case. The lead plaintiffs filed a consolidated class complaint on January 21, 2020. The Company filed a motion to dismiss the consolidated class complaint on March 23, 2020, and the District Court denied that motion on August 17, 2022. We reached a tentative settlement of this matter, which was preliminarily approved by the District Court on May 31, 2023. The Court granted final approval of the settlement on October 13, 2023.
Padilla Derivative Litigation. Four purported shareholder derivative cases have been filed in two District Courts relating to the factual allegations in the Padilla litigation; three of these cases have been consolidated in In re Community Health Systems, Inc. Shareholder Derivative Litigation and are pending in the United States District Court for the District of Delaware; namely, Faisal Hussain v. Wayne T. Smith, et al, filed August 12, 2019; Susheel Tanjavoor v. Wayne T. Smith, et al., filed August 29, 2019; and Kevin Aronson v. Wayne T. Smith, et al, filed April 29, 2020. The fourth case, Roger Trombley v. Wayne T. Smith, et al, filed August 20, 2019 (now Patrick Ayers v Wayne T. Smith, et al), is pending in the United States District Court for the Middle District of Tennessee. All four cases seek relief derivatively and on behalf of Community Health Systems, Inc. against certain Company officers and directors based on alleged breaches of fiduciary duty, unjust enrichment, and other acts related to certain Company disclosures in 2017 and 2018 regarding the Company’s adoption of Accounting Standards Update 2014-09, which the Company adopted effective January 1, 2018. We have reached a tentative settlement of these cases, which was preliminarily approved by the District Court on December 4, 2023. The District Court granted final approval of the settlement on January 29, 2024 and ordered dismissal of the case.
Government Investigations and Qui Tam Litigation
U.S. ex rel Larry Bomar v. Bayfront HMA Medical Center, LLC, et al – On September 14, 2017, our former hospital in St. Petersburg, Florida received a civil investigative demand, or CID, from the United States Department of Justice for information concerning its historic participation in the Florida Low Income Pool Program. The Low Income Pool Program, or LIP, is a funding pool to support healthcare providers that provide uncompensated care to Florida residents who are uninsured or underinsured. The CID sought documentation related to agreements between the hospital and Pinellas County. On June 13, 2019, an additional ten of our
48
affiliated hospitals in Florida received CIDs related to the same subject matter, along with two CIDs addressed to our affiliated management company and the Parent Company. We cooperated fully with the investigation. On September 15, 2021, the United States District Court for the Middle District of Florida ordered the unsealing of this qui tam complaint, which contains allegations related to the information sought in the September 14, 2017 CID. Specifically, the relator claims our former hospital in St. Petersburg – Bayfront Medical Center St. Petersburg – along with other, unaffiliated hospitals violated the False Claims Act by allegedly making certain contributions to a non-profit entity for the purpose of receiving supplemental Medicaid funding. The United States has declined to intervene in the case. We filed a motion to dismiss on November 23, 2021, which the District Court granted without prejudice on January 24, 2023. The relator filed a first amended complaint on February 14, 2023, our response to which was filed on February 28, 2023. The District Court granted our motion to dismiss with prejudice on August 21, 2023. The relator has filed a notice of appeal to the United States Court of Appeals for the Eleventh Judicial Circuit. We have reached a tentative settlement of this matter, which is subject to approval by the Department of Justice.
On January 11, 2024, we received a Civil Investigative Demand from the Department of Justice for documents and information relating to a variety of subjects, including practices and procedures related to utilization review, inpatient admissions and inpatient dialysis at our hospitals. We are cooperating fully with this investigation.
Commercial Litigation and Other Lawsuits
Thomas Mason, MD, Steven Folstad, MD and Mid-Atlantic Emergency Medical Associates, PA v Health Management Associates, LLC f/k/a Health Management Associates, Inc., Mooresville Hospital Management Associates d/b/a Lake Norman Regional Medical Center, Statesville HMA, LLC d/b/a Davis Regional Medical Center, Envision Healthcare Corporation f/k/a Emergency Medical Services Corporation, Emcare Holdings, Inc., and Emergency Medical Services, LP. This alleged wrongful retaliation case is filed in the United States District Court for the Western District of North Carolina. The plaintiffs allege their agreements with the defendants were terminated in retaliation for plaintiffs’ alleged refusal to admit patients unnecessarily to the defendant hospitals or otherwise perform unnecessary diagnostic testing. The allegations of the complaint relate to time periods prior to the hospitals’ affiliation with the Company. The plaintiffs filed a Third Amended Complaint on April 26, 2019. The defendants filed motions to dismiss, which were granted in part and denied in part on September 5, 2019. We have settled this matter, and the District Court ordered dismissal of the case on November 2, 2023.
Tower Health, f/k/a Reading Health System, et al v CHS/Community Health Systems, Inc., et al. This breach of contract action is pending in the United States District Court for the Eastern District of Pennsylvania. The plaintiffs allege breaches of an asset purchase agreement in connection with the sale of Pottstown Memorial Medical Center. The alleged breaches regard plaintiffs’ contention that the defendants failed to disclose certain conditions related to the physical plant of the hospital, along with various other alleged breaches of the asset purchase agreement. The plaintiffs filed an amended complaint on July 22, 2019. Trial for this matter began May 3, 2021, and closed on October 5, 2021. On September 6, 2022, the District Court issued a Memorandum Opinion denying all of Tower Health’s claims and entering a judgment in favor of the Company. The district Court also awarded the Company its attorneys’ fees and costs. On October 4, 2022, Tower Health filed a Rule 59 motion to alter or amend the District Court’s judgment and a Rule 15 motion to amend its pleadings. The Company has filed oppositions to both motions and has separately moved for its attorney’s fees. On August 11, 2023, the District Court denied Tower Health’s Rule 59 and Rule 15 motions. Tower Health has filed a notice of appeal to the United States Court of Appeals for the Third Judicial District. Our motion for attorneys’ fees is still pending. We continue to vigorously defend this case.
Daniel H. Golden, as Litigation Trustee of the QHC Litigation Trust, and Wilmington Savings Fund Society, FSB, solely in its capacity as indenture trustee v Community Health Systems, Inc., et al. A complaint in this case was filed on October 25, 2021 in the United States Bankruptcy Court for the District of Delaware against various persons, including the Company, certain subsidiaries of the Company, certain former executive officers of the Company and Credit Suisse Securities (USA) LLC. Plaintiff Daniel H. Golden is the litigation trustee for a litigation trust, which was formed under the plan of reorganization of Quorum Health Corporation, or QHC, and certain affiliated entities confirmed by order of the United States Bankruptcy Court for the District of Delaware wherein QHC and certain affiliated entities contributed various causes of action to such litigation trust. Plaintiff Wilmington Savings Fund Society is the indenture trustee for certain notes issued by QHC. The complaint seeks damages and other forms of recovery arising out of certain alleged actions taken by the Company and the other defendants in connection with the spin-off of QHC, which was completed on April 29, 2016, and includes claims for unjust enrichment and for avoidance of certain transactions and payments by QHC to the Company connected with the spin-off, including the $1.21 billion special dividend paid by QHC to the Company as part of the spin-off transactions. We filed a motion to dismiss on January 14, 2022, and oral argument on that motion was heard on July 21, 2022. On March 16, 2023, the District Court granted in part and denied in part our motion to dismiss. We continue to vigorously defend this case.
49
Federal Trade Commission v. Novant Health, Inc. and Community Health Systems, Inc. On January 25, 2024, the Federal Trade Commission filed a Complaint for Temporary Restraining Order and Preliminary Injunction in the United States District Court for the Western District of North Carolina seeking to enjoin the consummation of our proposed sale of Lake Norman Regional Medical Center and Davis Regional Medical Center to Novant Health, Inc., or Novant, pursuant to the terms of a definitive agreement dated as of February 28, 2023, as amended, entered into by us with Novant. The FTC alleges, among other things, that the proposed sale of the two hospitals would violate federal antitrust laws. The administrative merits hearing on this matter will begin on April 29, 2024. We will vigorously defend this case and plan to consummate this contemplated transaction with Novant in accordance with the terms of the definitive agreement in the event that we and Novant prevail in this litigation.
Management of Significant Legal Proceedings
In accordance with our governance documents, including our Governance Guidelines and the charter of the Audit and Compliance Committee, our management of significant legal proceedings is overseen by the independent members of the Board of Directors and, in particular, the Audit and Compliance Committee. The Audit and Compliance Committee is charged with oversight of compliance, regulatory and litigation matters, and enterprise risk management. Management has been instructed to refer all significant legal proceedings and allegations of financial statement fraud, error, or misstatement to the Audit and Compliance Committee for its oversight and evaluation. Consistent with New York Stock Exchange and Sarbanes-Oxley independence requirements, the Audit and Compliance Committee is comprised entirely of individuals who are independent of our management, and are financially literate in accordance with New York Stock Exchange listing standards. In addition, four of the five members of the Audit and Compliance Committee are “audit committee financial experts” as defined in the Securities Exchange Act of 1934, as amended.
In addition, the Audit and Compliance Committee and the other independent members of the Board of Directors oversee the functions of the voluntary compliance program, including its auditing and monitoring functions and confidential disclosure program. In recent years, the voluntary compliance program has addressed the potential for a variety of billing errors that might be the subject of audits and payment denials by the CMS Recovery Audit Contractors’ permanent project, including MS-DRG coding, outpatient hospital and physician coding and billing, and medical necessity for services (including a focus on hospital stays of very short duration). Efforts by management, through the voluntary compliance program, to identify and limit risk from these government audits have included significant policy and guidance revisions, training and education, and auditing.
Item 4. Mine Safety Disclosures
Not applicable.
50
PART II
Item 5. Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities
We completed an initial public offering of our common stock on June 14, 2000. Our common stock began trading on June 9, 2000 and is listed on the New York Stock Exchange under the symbol CYH. As of February 14, 2024, there were approximately 185 holders of record of our common stock.
Stock Performance Graph
The following graph sets forth the cumulative return of our common stock during the five year period ended December 31, 2023, as compared to the cumulative return of the Standard & Poor’s 500 Stock Index (S&P 500) and the cumulative return of the Dow Jones Healthcare Index. The graph assumes an initial investment of $100 in our common stock and in each of the foregoing indices and the reinvestment of dividends where applicable. The comparisons in the graph below are based on historical data and are not indicative of, or intended to forecast, future performance of our common stock.
COMPARISON OF 5 YEAR CUMULATIVE TOTAL RETURN
Among Community Health Systems, Inc., the S&P 500 Index, and the Dow Jones US Health Care Index
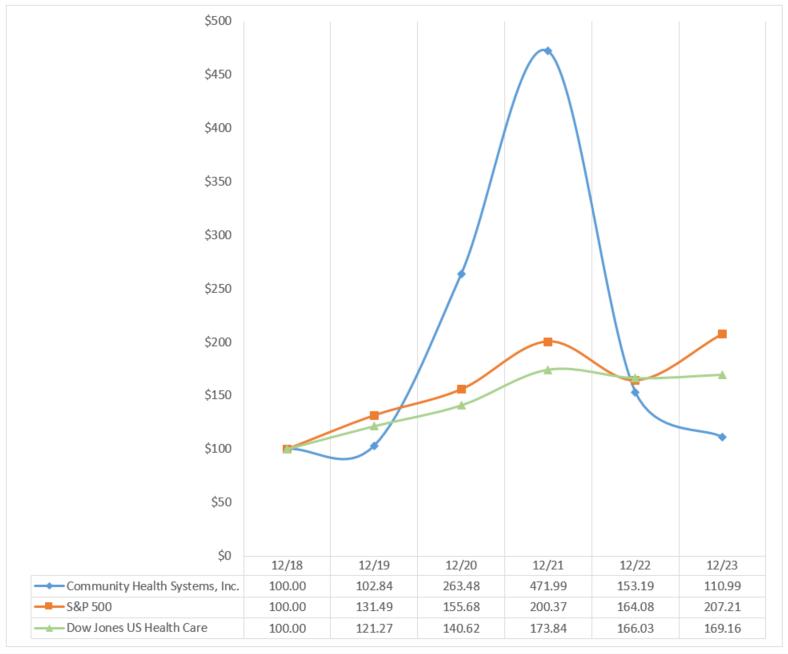
We are a holding company which operates through our subsidiaries. The ABL Facility and the indentures governing the senior and senior secured notes contain various covenants under which the assets of our subsidiaries are subject to certain restrictions relating to, among other matters, dividends and distributions, as referenced in the paragraph below.
51
The ABL Facility and the indentures governing each series of our outstanding notes restrict our subsidiaries from, among other matters, paying dividends and making distributions to us, which thereby limits our ability to pay dividends and/or repurchase stock. As of December 31, 2023, under the most restrictive test in these agreements (and subject to certain exceptions), we have approximately $300 million of capacity to pay permitted dividends and/or repurchase shares of stock or make other restricted payments.
The following table contains information about our purchases of common stock during the three months ended December 31, 2023.
Period |
|
Total |
|
|
Average |
|
|
Total |
|
|
Maximum |
|
||||
October 1, 2023 - |
|
|
|
|
|
|
|
|
|
|
|
|
||||
October 31, 2023 |
|
|
7,181 |
|
|
$ |
2.90 |
|
|
|
— |
|
|
|
— |
|
November 1, 2023 - |
|
|
|
|
|
|
|
|
|
|
|
|
||||
November 30, 2023 |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
December 1, 2023 - |
|
|
|
|
|
|
|
|
|
|
|
|
||||
December 31, 2023 |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
Total |
|
|
7,181 |
|
|
$ |
2.90 |
|
|
|
— |
|
|
|
— |
|
Item 6. Reserved
Reserved.
52
Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations
You should read this discussion together with our Consolidated Financial Statements and the accompanying Notes to Consolidated Financial Statements included elsewhere in this Form 10-K.
Executive Overview
We are one of the nation’s largest healthcare companies. Our affiliates are leading providers of healthcare services, developing and operating healthcare delivery systems in 40 distinct markets across 15 states. As of December 31, 2023, our subsidiaries own or lease 71 affiliated hospitals, with approximately 12,000 beds, and operate more than 1,000 sites of care, including physician practices, urgent care centers, freestanding emergency departments, occupational medicine clinics, imaging centers, cancer centers and ambulatory surgery centers. We generate revenues by providing a broad range of general and specialized hospital healthcare services and outpatient services to patients in the communities in which we are located. For the hospitals that we own and operate, we are paid for our services by governmental agencies, private insurers and directly by the patients we serve.
Economic conditions in the United States continue to be challenging in various respects, and the United States economy continues to experience significant inflationary pressures, elevated interest rates and challenging labor market conditions. Taking into account these factors, we have incurred in certain recent periods, and may continue to incur, increased expenses arising from factors such as wage inflation for permanent employees, increased rates for and utilization of temporary contract labor (including contract nursing personnel) and increased rates for outsourced medical specialists. While we have implemented cost containment and other measures to try to counteract these developments, we may be unable to fully offset the impact of these factors on the operation of our business.
If economic conditions in the United States further significantly deteriorate and/or public health conditions related to the COVID-19 pandemic significantly worsen, any such developments could materially and adversely affect our results of operations, financial position, and/or our cash flows.
Acquisition, Divestiture and Closure Activity
During the year ended December 31, 2023, we paid approximately $38 million to acquire the operating assets and related businesses of certain physician practices, clinics, ambulatory surgery centers and other ancillary businesses that operate within the communities served by our hospitals. We allocated the purchase price in connection with these acquisitions to property and equipment, intangible assets, working capital, noncontrolling interests and goodwill.
During 2023, we completed the divestiture of eight hospitals and the sale of a majority interest in one hospital. These hospitals represented annual net operating revenues in 2022 of approximately $594 million and we received total net proceeds of approximately $518 million in connection with these dispositions, inclusive of approximately $85 million received at a preliminary closing on December 30, 2022 in connection with the disposition of Greenbrier Valley Medical Center.
During 2022, we completed the divestiture of one hospital. This hospital represented annual net operating revenues in 2021 of approximately $18 million, and we received total net proceeds of less than $1 million in connection with this disposition.
During 2021, we completed the divestiture of five hospitals, including three which closed effective January 1, 2021 (for these hospitals we received net proceeds at a preliminary closing on December 31, 2020). These five hospitals represented annual net operating revenues in 2020 of approximately $275 million and, including the net proceeds for the three hospital divestitures that preliminarily closed on December 31, 2020, we received total net proceeds of approximately $28 million in connection with the disposition of these hospitals.
53
The following table provides a summary of hospitals that we divested (or, in the case of Lutheran Rehabilitation Hospital, in which the Company sold a majority interest) during the years ended December 31, 2023, 2022 and 2021:
Hospital |
|
Buyer |
|
City, State |
|
Licensed |
|
Effective Date |
2023 Divestitures: |
|
|
|
|
|
|
|
|
Greenbrier Valley Medical Center |
|
Vandalia Health, Inc. |
|
Ronceverte, WV |
|
122 |
|
January 1, 2023 |
Plateau Medical Center |
|
Vandalia Health, Inc. |
|
Oak Hill, WV |
|
25 |
|
April 1, 2023 |
Medical Center of South Arkansas |
|
SARH Holdings, Inc. |
|
El Dorado, AR |
|
166 |
|
July 1, 2023 |
Lutheran Rehabilitation Hospital |
|
Select Medical Corporation |
|
Fort Wayne, IN |
|
36 |
|
September 1, 2023 |
AllianceHealth Ponca City |
|
Integris Health |
|
Ponca City, OK |
|
140 |
|
November 1, 2023 |
AllianceHealth Woodward |
|
Integris Health |
|
Woodward, OK |
|
87 |
|
November 1, 2023 |
Bravera Health Brooksville |
|
Tampa General Hospital |
|
Brooksville, FL |
|
120 |
|
December 1, 2023 |
Bravera Health Spring Hill |
|
Tampa General Hospital |
|
Spring Hill, FL |
|
124 |
|
December 1, 2023 |
Bravera Health Seven Rivers |
|
Tampa General Hospital |
|
Crystal River, FL |
|
128 |
|
December 1, 2023 |
|
|
|
|
|
|
|
|
|
2022 Divestiture: |
|
|
|
|
|
|
|
|
AllianceHealth Seminole |
|
SSM Health Care of Oklahoma, Inc. |
|
Seminole, OK |
|
32 |
|
July 1, 2022 |
|
|
|
|
|
|
|
|
|
2021 Divestitures: |
|
|
|
|
|
|
|
|
Lea Regional Medical Center |
|
Covenant Health System |
|
Hobbs, NM |
|
84 |
|
January 1, 2021 |
Tennova Healthcare - Tullahoma |
|
Vanderbilt University Medical Center |
|
Tullahoma, TN |
|
135 |
|
January 1, 2021 |
Tennova Healthcare - Shelbyville |
|
Vanderbilt University Medical Center |
|
Shelbyville, TN |
|
60 |
|
January 1, 2021 |
Northwest Mississippi Medical Center |
|
Delta Health System |
|
Clarksdale, MS |
|
181 |
|
February 1, 2021 |
AllianceHealth Midwest |
|
SSM Health Care of Oklahoma, Inc. |
|
Midwest City, OK |
|
255 |
|
April 1, 2021 |
|
|
|
|
|
|
|
|
|
During the three months ended September 30, 2022, we completed the closure of Shorepoint Health Venice hospital (312 licensed beds) in Venice, Florida. We recorded an impairment charge of approximately $29 million during the year ended December 31, 2022, to adjust the fair value of the long-lived assets of this hospital, including property and equipment and capitalized software costs, based on their estimated fair value.
During the three months ended September 30, 2022, the provision of inpatient services and substantially all outpatient services ceased at First Hospital Wyoming Valley (psychiatric hospital) (149 licensed beds) in Wilkes-Barre, Pennsylvania, resulting in the closure of this facility being substantially complete as of September 30, 2022. We completed the closure of First Hospital Wyoming Valley during the three months ended December 31, 2022. We recorded an impairment charge of approximately $15 million during the year ended December 31, 2022, to adjust the fair value of the long-lived assets of this hospital, including property and equipment and capitalized software costs, based on their estimated fair value.
Effective December 31, 2022, the lease for AllianceHealth Clinton (56 licensed beds) in Clinton, Oklahoma expired and was not renewed. We recorded an impairment charge of approximately $1 million during the year ended December 31, 2022 in conjunction with exiting the lease to operate this hospital.
On July 30, 2021, we sold our unconsolidated equity interests in Macon Healthcare, LLC, a joint venture with certain subsidiaries of HCA representing two hospitals in Macon, Georgia, in which we owned a 38% interest. We received $110 million in cash in connection with the sale of these equity interests and recognized a pre-tax gain of approximately $39 million on the sale of our investments in unconsolidated affiliates during the year ended December 31, 2021.
In addition to hospitals divested in 2021, 2022 and in 2023, we have entered into a definitive agreement to sell two hospitals as noted below where the divestiture has not yet been completed. On February 28, 2023, we entered into a definitive agreement for the sale of substantially all of the assets of Lake Norman Regional Medical Center (123 licensed beds) in Mooresville, North Carolina, and Davis Regional Medical Center (144 licensed beds) in Statesville, North Carolina, to Novant Health, Inc. For additional information regarding this potential disposition, see the Current Report on Form 8-K filed by us on February 28, 2023. On January 25, 2024, the Federal Trade Commission, or FTC, filed a complaint seeking to enjoin the consummation of the sale of these hospitals to Novant. For additional information regarding this litigation, see the Legal Proceedings section of Part I, Item 3 of this Form 10-K. Taking into account this FTC action, there can be no assurance that this transaction with Novant will be completed, or if this transaction is completed, the ultimate timing of the completion of this transaction.
Moreover, we may give consideration to divesting certain additional hospitals and non-hospital businesses. Generally, these hospitals and non-hospital businesses are not in one of our strategically beneficial services areas, are less complementary to our business strategy and/or have lower operating margins. In addition, we continue to receive interest from potential acquirers for certain of our hospitals and non-hospital businesses. As such, we may sell additional hospitals and/or non-hospital businesses if we consider any such disposition to be in our best interests. We expect proceeds from any such divestitures to be used for general corporate purposes (including potential debt repayments and/or debt repurchases) and capital expenditures.
54
Overview of Operating Results
Our net operating revenues for the year ended December 31, 2023 increased $279 million to approximately $12.5 billion compared to approximately $12.2 billion for the year ended December 31, 2022. On a same-store basis, net operating revenues for the year ended December 31, 2023 increased $552 million.
We had net income of $16 million during the year ended December 31, 2023, compared to $179 million for the year ended December 31, 2022. Net income for the year ended December 31, 2023 included the following:
Net income for the year ended December 31, 2022 included the following:
Consolidated inpatient admissions for the year ended December 31, 2023, increased 0.3%, compared to the year ended December 31, 2022, and consolidated adjusted admissions for the year ended December 31, 2023, increased 1.7%, compared to the year ended December 31, 2022. Same-store inpatient admissions for the year ended December 31, 2023, increased 3.5%, compared to the year ended December 31, 2022, and same-store adjusted admissions for the year ended December 31, 2023, increased 5.3%, compared to the year ended December 31, 2022.
Self-pay revenues represented approximately 1.1% and 0.7% of net operating revenues for the years ended December 31, 2023 and 2022, respectively. The amount of foregone revenue related to providing charity care services as a percentage of net operating revenues was approximately 10.4% and 11.5% for the years ended December 31, 2023 and 2022, respectively. Direct and indirect costs incurred in providing charity care services as a percentage of net operating revenues was approximately 1.1% and 1.4% for the years ended December 31, 2023 and 2022, respectively.
Overview of Legislative and Other Governmental Developments
The healthcare industry is subject to changing political, regulatory, and economic influences that may affect our business. In recent years, the U.S. Congress and certain state legislatures have introduced and passed a large number of proposals and legislation affecting the healthcare system, including laws intended to impact access to health insurance and reduce healthcare costs and government spending. The most prominent of these efforts, the Affordable Care Act, affects how healthcare services are covered, delivered and reimbursed, and expanded health insurance coverage through a combination of public program expansion and private sector health insurance reforms. The Affordable Care Act has been, and continues to be, subject to legislative and regulatory changes and court challenges. To increase access to health insurance during the COVID-19 pandemic, the ARPA enhanced subsidies for individuals eligible to purchase coverage through Affordable Care Act marketplaces. Subsequent legislation extended these enhanced subsidies through 2025. In addition, early COVID-related legislation required states to maintain continuous Medicaid enrollment, among other conditions, to receive a temporary increase in federal funds for Medicaid expenditures. The expiration of this “continuous coverage” requirement in April 2023 has resulted in significant Medicaid coverage disruptions and dis-enrollments. CMS has required certain
55
states to pause disenrollments due to noncompliant renewal systems. These and other changes and initiatives may impact the number of individuals that elect to obtain public or private health insurance or the scope of such coverage, if purchased.
Of critical importance to us is the potential impact of any changes specific to the Medicaid program, including the funding and expansion provisions of the Affordable Care Act and subsequent legislation or agency initiatives. Historically, the states with the greatest reductions in the number of uninsured adult residents have expanded Medicaid under the Affordable Care Act. A number of states have opted out of the Medicaid coverage expansion provisions, but could ultimately decide to expand their programs at a later date. Of the 15 states in which we operated hospitals as of December 31, 2023, nine states have taken action to expand their Medicaid programs. At this time, the other six states have not, including Florida, Alabama, Tennessee, Mississippi and Texas, where we operated a significant number of hospitals as of December 31, 2023. Some states use, or have applied to use, waivers granted by CMS to implement expansion, impose different eligibility or enrollment conditions, or otherwise implement programs that vary from federal standards.
Other recent reform initiatives and proposals at the federal and state levels include those focused on price transparency and limiting out-of-network charges, which may impact prices, our competitive position and the relationships between hospitals, insurers, patients, and ancillary providers (such as anesthesiologists, radiologists, and pathologists). For example, the No Surprises Act imposes various requirements on providers and health plans intended to prevent “surprise” medical bills. Among other restrictions and requirements, the law prohibits providers from charging patients an amount beyond the in-network cost sharing amount for services rendered by out-of-network providers, subject to limited exceptions. For services for which balance billing is prohibited (even when no balance billing occurs), the No Surprises Act may limit the amounts received by out-of-network providers from health plans, and also establishes a dispute resolution process for providers and payors to handle payment disputes that cannot be resolved through direct negotiations. The regulations and related guidance implementing the No Surprises Act have been and continue to be subject to legal challenges. The No Surprises Act also requires providers to provide a good faith estimate of expected charges to uninsured or self-pay patients for scheduled items and services, in advance of the date of the scheduled item or service or upon request. Based on these estimates, patients may invoke a patient-provider dispute resolution process established by regulation to challenge charges in certain circumstances.
Other trends toward transparency and value-based purchasing may impact the competitive position and patient volumes of providers. For example, the CMS Care Compare website makes available to the public certain data that hospitals submit in connection with Medicare reimbursement claims, including hospital performance data on quality measures and patient satisfaction. In addition, Medicare reimbursement for hospitals is adjusted based on quality and efficiency measures, and CMS currently administers various accountable care organizations and bundled payment demonstration projects. The CMS Innovation Center has highlighted the need to accelerate the movement to value-based care and drive broader system transformation.
Throughout the acute phase of the COVID-19 pandemic that began in 2020, federal and state governments passed legislation, promulgated regulations and took other administrative actions intended to assist healthcare providers in providing care to COVID-19 and other patients during the public health emergency and to provide financial relief. The public health emergency declared by HHS in response to the pandemic expired in May 2023. Although federal and state governments have terminated most of the temporary measures that were implemented to assist providers, the effects of certain of these measures, including those intended to provide financial relief during the public health emergency, continue to impact providers. For example, the BCA sequestration was extended several times as part of COVID-relief and subsequent legislation, and the payment reductions are currently set to continue through April 2032. Further, the ARPA, in addition to providing funding for healthcare providers, increased the federal budget deficit in a manner that triggers an additional statutorily mandated sequestration under the Pay-As-You Go Act of 2010. As a result, an additional Medicare spending reduction of up to 4% was required to take effect in January 2022. However, Congress has delayed implementation of this payment reduction until 2025.
We received pandemic relief fund payments through various federal, state and local programs of approximately $161 million and $58 million during the years ended December 31, 2022 and 2021. Approximately $173 million and $148 million during the years ended December 31, 2022 and 2021, respectively, was recognized as pandemic relief funds within the consolidated statements of (loss) income. We did not receive or recognize any significant level of payments or benefits under the Coronavirus Aid, Relief, and Economic Security Act, or the CARES Act, or other COVID-19 related stimulus and relief legislation during the year ended December 31, 2023 and does not expect to receive or recognize any significant level of payments or benefit under the CARES Act and other existing legislation related to COVID-19 in future periods.
56
Reimbursement by government programs may be affected by broad shifts in payment policy. For example, recent changes related to the 340B Drug Pricing Program have implications for all hospitals reimbursed under the outpatient PPS, including those, like ours, that do not participate in the program. In 2018, CMS implemented a payment policy that reduced Medicare payments for 340B hospitals for most drugs obtained at 340B-discounted rates and that resulted in increased payments for non-340B hospitals. In June 2022, the U.S. Supreme Court, in American Hospital Association v. Becerra, invalidated past payment cuts for hospitals participating in the 340B Drug Pricing Program. In light of the U.S. Supreme Court decision and to achieve budget neutrality, CMS implemented a reduction of approximately 3.1% to payment rates for non-drug services under the outpatient PPS for calendar year 2023. In addition, HHS directed that $9 billion be paid to affected 340B providers in one-time lump sum payments as the remedy for calendar years 2018 through 2022. Moreover, in order to comply with budget neutrality requirements, HHS finalized a corresponding offset in future non-drug item and service payments for all outpatient PPS providers (except new providers) that will reduce the outpatient PPS conversion factor by 0.5% annually. This adjustment will start in calendar year 2026 and continue for approximately 16 years. This reduction to payment rates adversely affected our results for the year ended December 31, 2023, and the reduction to the outpatient PPS conversion factor as noted above is anticipated to adversely impact our results.
Sources of Revenue
The following table presents the approximate percentages of net operating revenues by payor source for the periods indicated. The data for the periods presented are not strictly comparable due to the effect that businesses acquired, sold, closed or opened during each of the respective periods, as applicable, have had on these statistics.
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Medicare |
|
|
19.9 |
% |
|
|
20.9 |
% |
|
|
21.4 |
% |
Medicare Managed Care |
|
|
16.8 |
|
|
|
16.1 |
|
|
|
15.1 |
|
Medicaid |
|
|
14.3 |
|
|
|
14.8 |
|
|
|
13.5 |
|
Managed Care and other third-party payors |
|
|
47.9 |
|
|
|
47.5 |
|
|
|
49.1 |
|
Self-pay |
|
|
1.1 |
|
|
|
0.7 |
|
|
|
0.9 |
|
Total |
|
|
100.0 |
% |
|
|
100.0 |
% |
|
|
100.0 |
% |
As shown above, we receive a substantial portion of our revenues from the Medicare, Medicare Managed Care and Medicaid programs. Included in Managed Care and other third-party payors is net operating revenues from insurance companies with which we have insurance provider contracts, insurance companies for which we do not have insurance provider contracts, workers’ compensation carriers and non-patient service revenue, such as gain (loss) on investments, rental income and cafeteria sales. We generally expect the portion of revenues received from the Medicare, Medicare Managed Care and Medicaid programs to increase over the long-term due to the general aging of the population and other factors, including health reform initiatives. There has been a trend toward increased enrollment in Medicare Managed Care and Medicaid managed care programs, which may adversely affect our net operating revenues. We may also be impacted by regulatory requirements imposed on insurers, such as minimum medical-loss ratios and specific benefit requirements. Furthermore, in the normal course of business, managed care programs, insurance companies and employers actively negotiate the amounts paid to hospitals. Our relationships with payors may be impacted by price transparency initiatives and out-of-network billing restrictions, including those in the No Surprises Act. There can be no assurance that we will retain our existing reimbursement arrangements or that third-party payors will not attempt to further reduce the rates they pay for our services.
Net operating revenues include amounts estimated by management to be reimbursable by Medicare and Medicaid under prospective payment systems and provisions of cost-based reimbursement and other payment methods. In addition, we are reimbursed by non-governmental payors using a variety of payment methodologies. Amounts we receive for the treatment of patients covered by Medicare, Medicaid and non-governmental payors are generally less than our standard billing rates. We account for the differences between the estimated program reimbursement rates and our standard billing rates as contractual allowance adjustments, which we deduct from gross revenues to arrive at net operating revenues. Final settlements under some of these programs are subject to adjustment based on administrative review and audit by third parties. We account for adjustments to previous program reimbursement estimates as contractual allowance adjustments and report them in the periods that such adjustments become known. Contractual allowance adjustments related to final settlements and previous program reimbursement estimates impacted net operating revenues by an insignificant amount in each of the years ended December 31, 2023, 2022 and 2021.
The payment rates under the Medicare program for hospital inpatient and outpatient acute care services are based on prospective payment systems, which depend upon a patient’s diagnosis or the clinical complexity of services provided to a patient, among other factors. These rates are indexed for inflation annually, although increases have historically been less than actual inflation. On August 1, 2023, CMS published the final rule to increase this index by 3.3% for hospital inpatient acute care services that are reimbursed under the prospective payment system for federal fiscal year 2024 (which began October 1, 2023). Together with other changes to
57
payment policies, payment rates for hospital inpatient acute care services are expected to increase approximately 3.1%. Hospitals that do not submit required patient quality data are subject to a reduction in payments. We are complying with this data submission requirement. Payments may also be affected by various other adjustments, including those that depend on patient-specific or hospital specific factors. For example, the “two midnight rule” establishes admission and medical review criteria for inpatient services limiting when services to Medicare beneficiaries are payable as inpatient hospital services. Reductions in the rate of increase or overall reductions in Medicare reimbursement may cause a decline in the growth of our net operating revenues.
Payment rates under the Medicaid program vary by state. In addition to the base payment rates for specific claims for services rendered to Medicaid enrollees, several states utilize supplemental reimbursement programs to make separate payments that are not specifically tied to an individual’s care, some of which offset a portion of the cost of providing care to Medicaid and indigent patients. These programs are funded with a combination of state and federal resources, including, in certain instances, fees or taxes levied on the providers. The programs are generally authorized by CMS for a specified period of time and require CMS’s approval to be extended. We are unable to predict whether or on what terms CMS will extend the supplemental programs in the states in which we operate. Under these supplemental programs, we recognize revenue and related expenses in the period in which amounts are estimable and payment is reasonably assured. Reimbursement under these programs is reflected in net operating revenues and included as Medicaid revenue in the table above, and fees, taxes or other program related costs are reflected in other operating expenses.
Results of Operations
Our hospitals and other sites of care offer a broad variety of inpatient and outpatient medical and surgical services. These include general acute care, emergency room, general and specialty surgery, critical care, internal medicine, obstetrics, diagnostic services, psychiatric and rehabilitation services. Utilization of services and our results of operations are dependent on a multitude of factors including seasonal fluctuations in demand. Historically, the strongest demand for hospital services generally occurs during the winter months, and the weakest demand generally occurs during the summer months.
The following tables summarize, for the periods indicated, selected operating data.
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Operating results, as a percentage of net operating revenues: |
|
|
|
|
|
|
|
|
|
|||
Net operating revenues |
|
|
100.0 |
% |
|
|
100.0 |
% |
|
|
100.0 |
% |
Operating expenses (a) |
|
|
(89.0 |
) |
|
|
(88.3 |
) |
|
|
(84.1 |
) |
Depreciation and amortization |
|
|
(4.0 |
) |
|
|
(4.4 |
) |
|
|
(4.4 |
) |
Impairment and gain (loss) on sale of businesses, net |
|
|
0.7 |
|
|
|
(0.6 |
) |
|
|
(0.2 |
) |
Income from operations |
|
|
7.7 |
|
|
|
6.7 |
|
|
|
11.3 |
|
Interest expense, net |
|
|
(6.7 |
) |
|
|
(7.0 |
) |
|
|
(7.2 |
) |
Gain (loss) from early extinguishment of debt |
|
|
0.6 |
|
|
|
2.1 |
|
|
|
(0.6 |
) |
Gain on sale of equity interests in Macon Healthcare, LLC |
|
|
— |
|
|
|
— |
|
|
|
0.3 |
|
Gain from CoreTrust Transaction |
|
|
— |
|
|
|
1.0 |
|
|
|
— |
|
Equity in earnings of unconsolidated affiliates |
|
|
0.1 |
|
|
|
0.1 |
|
|
|
0.2 |
|
Income before income taxes |
|
|
1.7 |
|
|
|
2.9 |
|
|
|
4.0 |
|
Provision for income taxes |
|
|
(1.6 |
) |
|
|
(1.4 |
) |
|
|
(1.0 |
) |
Net income |
|
|
0.1 |
|
|
|
1.5 |
|
|
|
3.0 |
|
Less: Net income attributable to noncontrolling interests |
|
|
(1.2 |
) |
|
|
(1.1 |
) |
|
|
(1.1 |
) |
Net (loss) income attributable to Community Health Systems, |
|
|
|
|
|
|
|
|
|
|||
Inc. stockholders |
|
|
(1.1 |
)% |
|
|
0.4 |
% |
|
|
1.9 |
% |
58
|
|
Year Ended December 31, |
|
|||||
|
|
2023 |
|
|
2022 |
|
||
Percentage increase (decrease) from prior year: |
|
|
|
|
|
|
||
Net operating revenues |
|
|
2.3 |
% |
|
|
(1.3 |
)% |
Admissions (b) |
|
|
0.3 |
|
|
|
(1.7 |
) |
Adjusted admissions (c) |
|
|
1.7 |
|
|
|
2.6 |
|
Average length of stay (d) |
|
|
(4.3 |
) |
|
|
(6.0 |
) |
Net (loss) income attributable to Community Health Systems, |
|
|
(389.1 |
) |
|
|
(80.0 |
) |
Same-store percentage (decrease) increase from prior year (e): |
|
|
|
|
|
|
||
Net operating revenues |
|
|
4.8 |
% |
|
|
(0.2 |
)% |
Admissions (b) |
|
|
3.5 |
|
|
|
0.5 |
|
Adjusted admissions (c) |
|
|
5.3 |
|
|
|
5.0 |
|
Items (b) – (e) are metrics used to manage our performance. These metrics provide useful insight to investors about the volume and acuity of services we provide, which aid in evaluating our financial results.
Year Ended December 31, 2023 Compared to Year Ended December 31, 2022
Net operating revenues increased by 2.3% to approximately $12.5 billion for the year ended December 31, 2023, from approximately $12.2 billion for the year ended December 31, 2022. Net operating revenues on a same-store basis from hospitals that were operated throughout both periods increased $552 million, or 4.8%, during the year ended December 31, 2023, compared to the same period in 2022. On a period-over-period basis, the increase in net operating revenues was primarily attributable to higher inpatient and outpatient volumes, increased reimbursement rates, higher acuity and an increase in non-patient revenue, partially offset by unfavorable changes in payor mix. Non-same-store net operating revenues decreased $273 million during the year ended December 31, 2023, compared to the same period in 2022, with the decrease attributable primarily to the divestiture of hospitals during 2022 and 2023. On a consolidated basis, inpatient admissions increased by 0.3% and adjusted admissions increased by 1.7% during the year ended December 31, 2023, compared to the same period in 2022. On a same-store basis, net operating revenues per adjusted admission decreased 0.5%, while inpatient admissions increased by 3.5% and adjusted admissions increased by 5.3% for the year ended December 31, 2023, compared to the same period in 2022.
Operating costs and expenses, as a percentage of net operating revenues, decreased from 93.3% during the year ended December 31, 2022 to 92.3% during the year ended December 31, 2023. Operating costs and expenses, excluding depreciation and amortization and impairment and (gain) loss on sale of businesses, as a percentage of net operating revenues, increased from 88.3% for the year ended December 31, 2022 to 89.0% for the year ended December 31, 2023. Salaries and benefits decreased as a percentage of net operating revenues from 43.6% for the year ended December 31, 2022 to 43.4% for the year ended December 31, 2023, primarily due to an increase in net operating revenues, partially offset by increased hiring commensurate with lower utilization of contract labor. Supplies, as a percentage of net operating revenues, decreased from 16.2% for the year ended December 31, 2022 to 16.0% for the year ended December 31, 2023. Other operating expenses, as a percentage of net operating revenues, decreased from 27.3% for the year ended December 31, 2022 to 27.0% for the year ended December 31, 2023, primarily due to an increase in net operating revenues and lower utilization of and rates paid for contract labor, partially offset by higher costs for professional liability insurance and higher rates paid for outsourced medical specialists. Lease cost and rent, as a percentage of net operating revenues, remained consistent at 2.6% for the years ended December 31, 2023 and 2022. Pandemic relief funds, as a percentage of net operating revenues, were 0.0% for the year ended December 31, 2023, compared to (1.4)% for the same period in 2022.
Depreciation and amortization, as a percentage of net operating revenues, decreased to 4.0% for the year ended December 31, 2023 from 4.4% for the year ended December 31, 2022.
59
Impairment and (gain) loss on sale of businesses, net was a gain of $87 million for the year ended December 31, 2023, compared to expense of $71 million for the same period in 2022. The gain in 2023 and the expense in 2022 related primarily to divestiture activity during each respective period as discussed more specifically under “Acquisition, Divestiture and Closure Activity” herein.
Interest expense, net, decreased by $28 million to $830 million for the year ended December 31, 2023 compared to $858 million for the same period in 2022. This was primarily due to our refinancing activity during 2023 and 2022.
Gain from early extinguishment of debt of $72 million was recognized during the year ended December 31, 2023, compared to a gain from early extinguishment of debt of $253 million in the same period in 2022, as a result of our refinancing activity during the years ended December 31, 2023 and 2022.
There was no gain from the CoreTrust Transaction during the year ended December 31, 2023. Gain from the CoreTrust Transaction of $119 million was recognized during the year ended December 31, 2022.
Equity in earnings of unconsolidated affiliates, as a percentage of net operating revenues, remained consistent at (0.1)% for the years ended December 31, 2023 and 2022.
The net results of the above-mentioned changes resulted in income before income taxes decreasing $142 million to $207 million for the year ended December 31, 2023 from $349 million for the same period in 2022.
Our provision for income taxes for the years ended December 31, 2023 and 2022 was $191 million and $170 million, respectively, and the effective tax rates were 92.3% and 48.7% for the years ended December 31, 2023 and 2022, respectively. The increase in the provision for income taxes for the year ended December 31, 2023, compared to the same period in 2022 was primarily due to non-deductible goodwill related to divested hospitals in 2023 compared to 2022. The difference in our effective tax rate for the year ended December 31, 2023, compared to the same period in 2022 was due to the aforementioned increase in the provision for income taxes and the decrease in income before taxes.
Net income, as a percentage of net operating revenues, was 0.1% for the year ended December 31, 2023, compared to 1.5% for the same period in 2022.
Net income attributable to noncontrolling interests, as a percentage of net operating revenues, was 1.2% for the year ended December 31, 2023, compared to 1.1% for the same period in 2022.
Net (loss) income attributable to Community Health Systems, Inc. was $(133) million for the year ended December 31, 2023, compared to net income of $46 million for the same period in 2022.
Year Ended December 31, 2022 Compared to Year Ended December 31, 2021
Net operating revenues decreased by 1.3% to approximately $12.2 billion for the year ended December 31, 2022, from approximately $12.4 billion for the year ended December 31, 2021. Net operating revenues on a same-store basis from hospitals that were operated throughout both periods decreased $27 million, or 0.2%, during the year ended December 31, 2022, compared to the same period in 2021. On a period-over-period basis, there was a decline in net operating revenues as a result of fewer inpatient admissions, which was partially offset by an increase in outpatient visits and surgeries. Also, lower overall acuity of services was partially offset by improved reimbursement rates. Non-same-store net operating revenues decreased $130 million during the year ended December 31, 2022, compared to the same period in 2021, with the decrease attributable primarily to the divestiture of hospitals during 2021 and 2022. On a consolidated basis, inpatient admissions decreased by 1.7% during the year ended December 31, 2022, compared to the same period in 2021. Also on a consolidated basis, adjusted admissions increased by 2.6% during the year ended December 31, 2022, as compared to the same period in 2021. On a same-store basis, net operating revenues per adjusted admission decreased 5.0%, while inpatient admissions increased by 0.5% and adjusted admissions increased by 5.0% for the year ended December 31, 2022, compared to the same period in 2021.
Operating costs and expenses, as a percentage of net operating revenues, increased from 88.7% during the year ended December 31, 2021 to 93.3% during the year ended December 31, 2022. Operating costs and expenses, excluding depreciation and amortization and impairment and (gain) loss on sale of businesses, as a percentage of net operating revenues, increased from 84.1% for the year ended December 31, 2021 to 88.3% for the year ended December 31, 2022. Salaries and benefits increased as a percentage of net operating revenues from 42.4% for the year ended December 31, 2021 to 43.6% for the year ended December 31, 2022, primarily due to wage increases driven by inflation and competitive labor market conditions. Supplies, as a percentage of net operating revenues, decreased from 16.5% for the year ended December 31, 2021 to 16.2% for the year ended December 31, 2022. Other operating expenses, as a percentage of net operating revenues, increased from 23.9% for the year ended December 31, 2021 to 27.3% for the year ended December 31, 2022, primarily due to higher costs for contract labor, professional liability insurance and medical specialist fees. Lease cost and rent, as a percentage of net operating revenues, increased from 2.5% for the year ended December 31, 2021 to
60
2.6% for the year ended December 31, 2022. Pandemic relief funds, as a percentage of net operating revenues, were (1.4)% for the year ended December 31, 2022, compared to (1.2)% for the same period in 2021.
Depreciation and amortization, as a percentage of net operating revenues, remained consistent at 4.4% for both years ended December 31, 2022 and 2021.
Impairment and (gain) loss on sale of businesses was $71 million for the year ended December 31, 2022, which primarily related to a hospital divestiture and the closure or non-renewal of leases for three hospitals as discussed more specifically under “Acquisition, Divestiture, Closures and Other Activity” herein, compared to $24 million for the same period in 2021, which related primarily to divestitures during the period.
Interest expense, net, decreased by $27 million to $858 million for the year ended December 31, 2022 compared to $885 million for the same period in 2021. This was primarily due to our debt refinancing activity during 2021 and 2022.
Gain from early extinguishment of debt of $253 million was recognized during the year ended December 31, 2022, compared to a loss from early extinguishment of debt of $79 million in the same period in 2021, as a result of the refinancing of certain of our outstanding notes in each period as well as open market and privately negotiated repurchases of certain of our outstanding notes completed during the year ended December 31, 2022.
There was no pre-tax gain recognized on the sale of unconsolidated equity interests during the year ended December 31, 2022. A pre-tax gain of $39 million was recognized during the year ended December 31, 2021 on the sale of unconsolidated equity interests in Macon Healthcare, LLC, a joint venture with certain subsidiaries of HCA representing two hospitals in Macon, Georgia, in which we owned a 38% interest.
Gain from the CoreTrust Transaction of $119 million was recognized during the year ended December 31, 2022, as discussed below under the heading “Liquidity and Capital Resources.” There was no gain from the CoreTrust Transaction recognized during the year ended December 31, 2021.
Equity in earnings of unconsolidated affiliates, as a percentage of net operating revenues, decreased to (0.1)% for the year ended December 31, 2022 from (0.2)% for the year ended December 31, 2021, primarily due to the sale of our unconsolidated equity interests in Macon Healthcare, LLC during the year ended December 31, 2021.
The net results of the above-mentioned changes resulted in income before income taxes decreasing $150 million to $349 million for the year ended December 31, 2022 from $499 million for the year ended December 31, 2021.
Our provision for income taxes for the years ended December 31, 2022 and 2021 was $170 million and $131 million, respectively, and the effective tax rates were 48.7% and 26.3% for the years ended December 31, 2022 and 2021, respectively. The increase in the provision for income taxes for the year ended December 31, 2022, compared to the same period in 2021 was primarily due to an increase in non-deductible interest for 2022 compared to 2021, compounded by an adverse change in the Internal Revenue Code Section 163(j) limit for deductible interest expense beginning in 2022. The difference in our effective tax rate for the year ended December 31, 2022, compared to the same period in 2021 was due to the aforementioned increase in the provision for income taxes and the decline in income before taxes.
Net income, as a percentage of net operating revenues, was 1.5% for the year ended December 31, 2022, compared to 3.0% for the same period in 2021.
Net income attributable to noncontrolling interests, as a percentage of net operating revenues, remained consistent at 1.1% for both years ended December 31, 2022 and 2021.
Net income attributable to Community Health Systems, Inc. was $46 million for the year ended December 31, 2022, compared to $230 million for the same period in 2021.
Liquidity and Capital Resources
2023 Compared to 2022
Net cash provided by operating activities was approximately $210 million for the year ended December 31, 2023, compared to $300 million for the year ended December 31, 2022. The decrease in cash provided by operating activities is partially the result of the payment of accumulated benefits under the Company's supplemental executive retirement plan, or SERP. Because securities are held in a rabbi trust to be used for the payment of SERP benefits, the aforementioned cash outflow is offset by inflows from sales of investments, which are reflected as a cash inflow from investing activities as noted below. Total cash paid for interest decreased to
61
approximately $801 million for the year ended December 31, 2023, from approximately $835 million for the year ended December 31, 2022. Cash paid for income taxes, net of refunds received, resulted in a net payment of $91 million and $6 million during the years ended December 31, 2023 and 2022, respectively.
Our net cash used in investing activities was approximately $26 million for the year ended December 31, 2023, compared to approximately $259 million for the year ended December 31, 2022, a decrease of approximately $233 million. The decrease in net cash used in investing activities during the year ended December 31, 2023, compared to the prior year, was primarily impacted by an increase of $99 million in cash from the net impact of the purchases and sales of available-for-sale debt and equity securities, including securities sold to pay SERP benefits as noted above, an increase of $343 million in cash proceeds from dispositions of hospitals and other ancillary operations, a decrease of $8 million in cash used to purchase investments in unconsolidated affiliates, an increase of $29 million in cash paid for acquisitions of facilities and other related businesses, an increase of $52 million in cash used for the purchase of property and equipment, an increase of $5 million in cash used to purchase other investments, a decrease of $10 million in cash proceeds from the sale of property and equipment, and a decrease resulting from $121 million in cash representing our share of proceeds from the CoreTrust Transaction distributed during the year ended December 31, 2022, compared to the year ended December 31, 2023.
Our net cash used in financing activities was $264 million for the year ended December 31, 2023, compared to $430 million for the year ended December 31, 2022, a decrease of $166 million. This was primarily due to the net effect of our debt repayments, refinancing activities, and cash paid for deferred financing costs and other debt-related costs during the years ended December 31, 2023 and 2022.
2022 Compared to 2021
Net cash provided by operating activities was approximately $300 million for the year ended December 31, 2022, compared to net cash used in operating activities of $131 million for the year ended December 31, 2021, with the change primarily attributable to the repayment of Medicare accelerated payments in 2021. Total cash paid for interest increased to approximately $835 million for the year ended December 31, 2022, from approximately $778 million for the year ended December 31, 2021. Cash paid for income taxes, net of refunds received, resulted in a net payment of $6 million and $4 million during the years ended December 31, 2022 and 2021, respectively.
Our net cash used in investing activities was approximately $259 million for the year ended December 31, 2022, compared to approximately $524 million for the year ended December 31, 2021, a decrease of approximately $265 million. The decrease in net cash used in investing activities during the year ended December 31, 2022, compared to the prior year, primarily resulted from a decrease of $54 million in cash used for the purchase of property and equipment, an increase of $28 million in cash proceeds from the sale of property and equipment, a decrease of $53 million in cash used to purchase other investments, a decrease of $65 million in cash used in the net impact of the purchases and sales of available-for-sale debt and equity securities, an increase resulting from $121 million in cash representing our share of proceeds from the CoreTrust Transaction distributed during the year ended December 31, 2022, and an increase of $72 million in cash proceeds from dispositions of hospitals and other ancillary operations. These items, which decreased cash used in investing activities, were partially offset by an increase of $6 million in cash paid for acquisitions of facilities and other related businesses, an increase of $12 million in cash used to purchase investments in unconsolidated affiliates, and a decrease of $110 million in cash from the sale of equity interests in Macon Healthcare, LLC during the year ended December 31, 2022, compared to the year ended December 31, 2021.
Our net cash used in financing activities was $430 million for the year ended December 31, 2022, compared to approximately $514 million for the year ended December 31, 2021, a decrease of approximately $84 million. This was primarily due to the net effect of our debt repayments, refinancing activities, and cash paid for deferred financing costs and other debt-related costs during the years ended December 31, 2022 and 2021.
Liquidity
Net working capital was approximately $1.1 billion and $896 million at December 31, 2023 and December 31, 2022, respectively. Net working capital increased by approximately $170 million between December 31, 2022 and December 31, 2023. The increase is primarily due to the increase in accounts receivable, other current assets and prepaid expenses and taxes as well as decreases in current operating lease liabilities, accrued liabilities for employee compensation, accrued interest, and other current accrued liabilities during the year ended December 31, 2023, partially offset by a decrease in cash, supplies and prepaid income taxes and an increase in accounts payable.
62
In addition to cash flows from operations, available sources of capital include amounts available under the asset-based loan (ABL) credit agreement, or the ABL Credit Agreement, as amended and restated on November 22, 2021, and anticipated access to public and private debt markets as well as proceeds from the disposition of hospitals or other investments such as our minority equity interests in various businesses, as applicable.
Pursuant to the ABL Credit Agreement, the lenders have extended to CHS/Community Health Systems, Inc., or CHS, a revolving asset-based loan facility. The maximum aggregate amount under the ABL Facility is $1.0 billion, subject to borrowing base capacity. At December 31, 2023, we had outstanding borrowings of $247 million and approximately $637 million of additional borrowing capacity (after taking into consideration $81 million of outstanding letters of credit) under the ABL Facility. Principal amounts outstanding under the ABL Facility, if any, will be due and payable in full on November 22, 2026.
2023 Financing Activity
On December 22, 2023, we completed a private offering of $1.000 billion aggregate principal amount of 10⅞% Senior Secured Notes due January 15, 2032, or the 10⅞% Senior Secured Notes due 2032. The proceeds of the offering were used, together with cash on hand, to redeem $985 million aggregate principal amount of 8% Senior Secured Notes due 2026 via a tender offer, which was funded on December 28, 2023, and to pay related fees and expenses. The 10⅞% Senior Secured Notes due 2032 bear interest at a rate of 10.875% per year payable semi-annually in arrears on February 15 and August 15 of each year, commencing on August 15, 2024.
During the year ended December 31, 2023, we extinguished a portion of certain series of our outstanding notes through a combination of open market and privately negotiated repurchases, as follows (in millions):
|
|
Principal Amount |
|
|
6% Senior Secured Notes due 2029 |
|
$ |
256 |
|
6⅞% Junior-Priority Secured Notes due 2029 |
|
|
142 |
|
6⅛% Junior-Priority Secured Notes due 2030 |
|
|
4 |
|
Total principal amount of debt extinguished |
|
$ |
402 |
|
A pre-tax gain from early extinguishment of debt of approximately $72 million was recognized associated with these financing activities during the year ended December 31, 2023.
2022 Financing Activity
On February 4, 2022, we completed a private offering of $1.535 billion aggregate principal amount of 5¼% Senior Secured Notes due May 15, 2030, or the 5¼% Senior Secured Notes due 2030. The proceeds of the offering were used to redeem the 6⅝% Senior Secured Notes due 2025 on February 4, 2022, and to pay related fees and expenses. The 5¼% Senior Secured Notes due 2030 bear interest at a rate of 5.250% per year payable semi-annually in arrears on May 15 and November 15, commencing on November 15, 2022.
During the year ended December 31, 2022, we extinguished a portion of certain series of our outstanding notes through a combination of open market and privately negotiated repurchases, as follows (in millions):
|
|
Principal Amount |
|
|
6⅞% Senior Notes due 2028 |
|
$ |
11 |
|
4¾% Senior Secured Notes due 2031 |
|
|
37 |
|
6⅞% Junior-Priority Secured Notes due 2029 |
|
|
389 |
|
6⅛% Junior-Priority Secured Notes due 2030 |
|
|
208 |
|
Total principal amount of debt extinguished |
|
$ |
645 |
|
A pre-tax gain from early extinguishment of debt of approximately $253 million was recognized associated with these financing activities during the year ended December 31, 2022.
Additional Liquidity Information
For information regarding our amended and restated asset-based loan (ABL) credit agreement and our other outstanding indebtedness, see Note 6 of the Notes to Consolidated Financial Statements included under Part II, Item 8 of this Form 10-K. Our ability to meet the restricted covenants and financial ratios and tests in the ABL Facility and the indentures governing our outstanding notes can be affected by events beyond our control, and we cannot assure you that we will meet those tests. A breach of any of these covenants could result in a default under the ABL Facility and/or the indentures that govern our outstanding notes. Upon the occurrence of an event of default under the ABL Facility or indentures that govern our outstanding notes, all amounts outstanding
63
under the ABL Facility and the indentures that govern our outstanding notes may become immediately due and payable and all commitments under the ABL Facility to extend further credit may be terminated.
As of December 31, 2023, approximately $21 million of our outstanding debt of approximately $11.5 billion is due within the next 12 months and approximately 98% of our outstanding debt has a fixed rate of interest. Our debt as a percentage of total capitalization was 111% at December 31, 2023, compared to 112% at December 31, 2022.
Net proceeds from divestitures, if any, are expected to be used for general corporate purposes (including potential debt repayments and/or debt repurchases) and capital expenditures.
Ongoing negative economic conditions may negatively impact our service mix, revenue mix, payor mix and patient volumes, as well as our ability to collect outstanding receivables. Any material increase in our billing cycles or deterioration in the collectability of our accounts receivable would adversely affect our cash flows and results of operations and may require an increased level of working capital.
We believe that our current levels of cash, internally generated cash flows and current levels of availability for additional borrowing under the ABL Facility, our anticipated continued access to the capital markets, and the use of proceeds from any potential future dispositions as noted above, will be sufficient to finance acquisitions, capital expenditures, working capital requirements, and any debt repurchases or other debt repayments we may elect to make or be required to make through the next 12 months and the foreseeable future thereafter. However, ongoing negative economic conditions (including inflationary conditions and elevated interest rate levels) have resulted in, and may continue to result in, significant disruptions of financial and capital markets, which could reduce our ability to access capital and negatively affect our liquidity in the future.
As noted above, during the years ended December 31, 2023 and 2022, we extinguished a portion of certain series of our outstanding notes through open market and privately negotiated repurchases, and we may elect from time to time to continue to purchase our outstanding debt in open market purchases, privately negotiated transactions or otherwise. Any such debt repurchases will depend upon prevailing market conditions, our liquidity requirements, contractual restrictions, applicable securities laws requirements, and other factors.
Capital Resources
Material cash requirements from known contractual and other obligations primarily consist of purchase obligations, long-term debt and related interest payments, operating leases, finance leasing and financing obligations, and capital expenditures related to routine capital, information systems infrastructure and applications, replacement or de novo construction projects and bed expansion projects, certain commitments and other investments. Refer to Notes 6, 9 and 15 of the Notes to Consolidated Financial Statements for amounts outstanding as of December 31, 2023 related to long-term debt, and related interest payments, operating leases, finance leasing and financing obligations, and certain commitments.
Purchase obligations include supplies and third-party services purchased in the normal course of business. Open purchase orders total $342 million as of December 31, 2023 and substantially all such amounts are due in the next 12 months. Other investments includes, among other things, purchases of investments in unconsolidated affiliates which are expected to be incurred within the next 24 months.
Cash expenditures for purchases of facilities and other related businesses were approximately $38 million in 2023, $9 million in 2022 and $3 million in 2021. Our expenditures for the years ended December 31, 2023, 2022 and 2021, were primarily related to physician practices, clinics, ambulatory surgery centers and other ancillary businesses, including the purchase of certain assets from American Physician Partners as described in Note 3 of the Notes to Consolidated Financial Statements included under Part II, Item 8 of this Form 10-K.
Excluding the cost to construct replacement and de novo hospitals, our cash expenditures for routine capital for the year ended December 31, 2023 totaled $466 million compared to $358 million in 2022 and $321 million in 2021. These capital expenditures related primarily to the purchase of additional equipment, major and minor renovations that result in additional bed capacity, and information systems infrastructure. The costs to construct replacement hospitals and de novo hospitals during the year ended December 31, 2023 were approximately $1 million. Costs to construct replacement hospitals totaled $17 million and $63 million for the years ended December 31, 2022 and 2021, respectively, primarily related to the construction of a replacement facility in Fort Wayne, Indiana. During the years ended December 31, 2022 and 2021, we also had cash expenditures of $40 million and $85 million, respectively, that represent both planning and construction costs primarily for de novo hospitals.
64
Pursuant to a hospital purchase agreement from our March 1, 2016 acquisition of Northwest Health - Starke, formerly known as Starke Hospital, we committed to spend up to $15 million toward the construction of a replacement facility in Knox, Indiana. Construction is required to be completed within five years of the date we enter into a new lease with Starke County, Indiana, the hospital lessor, or in the event we do not enter into a new lease with Starke County, construction shall be completed by September 30, 2026. We have not entered into a new lease with the lessor for Northwest Health - Starke.
In addition to the commitment to spend up to $15 million toward the construction of a replacement facility in Knox, Indiana, other off-balance sheet arrangements consist of letters of credit issued on the ABL Facility, primarily in support of potential insurance-related claims and specified outstanding bonds of approximately $81 million as well as approximately $6 million representing the maximum potential amount of future payments under physician recruiting guarantee commitments in excess of the liability recorded at December 31, 2023.
We expect total capital expenditures of approximately $350 million to $400 million in 2024.
Reimbursement, Legislative and Regulatory Changes
Ongoing legislative and regulatory efforts, and judicial interpretations, could reduce or otherwise adversely affect the payments we receive from Medicare and Medicaid and other payors. Within the statutory framework of the Medicare and Medicaid programs, there are substantial areas subject to administrative rulings, interpretations and discretion, and which are at times subject to court challenges, which may further affect payments made under those programs. Further, the federal and state governments might, in the future, reduce the funds available under those programs, require repayment of previously received funds or require more stringent utilization and quality reviews of hospital facilities. Additionally, there may be a continued rise in managed care programs and further restructuring of the financing and delivery of healthcare in the United States. These events could cause our future financial results to be adversely impacted. We cannot estimate the impact of Medicare and Medicaid reimbursement changes that have been enacted or otherwise determined, or that are currently or may in the future be under consideration. We cannot predict whether additional reimbursement reductions will be made or whether any such changes or other restructuring of the financing and delivery of healthcare would have a material adverse effect on our business, financial conditions, results of operations, cash flow, capital resources and liquidity.
Critical Accounting Policies
The discussion and analysis of our financial condition and results of operations are based upon our consolidated financial statements, which have been prepared in accordance with U.S. GAAP. The preparation of these financial statements requires us to make estimates and judgments that affect the reported amount of assets and liabilities, revenues and expenses, and related disclosure of contingent assets and liabilities at the date of our consolidated financial statements. Actual results may differ from these estimates under different assumptions or conditions.
Critical accounting policies are defined as those policies that involve a significant level of estimation uncertainty and have had or are reasonably likely to have a material impact on the financial condition or results of operations of the registrant. We believe that our critical accounting policies are limited to those described below. The following information should be read in conjunction with our significant accounting policies included in Note 1 of the Notes to Consolidated Financial Statements included under Part II, Item 8 of this Form 10-K.
Revenue Recognition
Net operating revenues include amounts estimated by management to be reimbursable by Medicare and Medicaid under prospective payment systems and provisions of cost-reimbursement and other payment methods. In addition, we are reimbursed by non-governmental payors using a variety of payment methodologies. Amounts we receive for treatment of patients covered by these programs are generally less than our standard billing rates. Explicit price concessions are recorded for contractual allowances that are calculated and recorded through a combination of internally- and externally-developed data collection and analysis tools to automate the monthly estimation of required contractual allowances. Within these automated systems, payors’ historical paid claims data and contracted amounts are utilized to calculate the contractual allowances. This data is updated on a monthly basis. All hospital contractual allowance calculations are subjected to monthly review by management to ensure reasonableness and accuracy. We account for the differences between the estimated program reimbursement rates and the standard billing rates as contractual allowance adjustments, which is one component of the deductions from gross revenues to arrive at net operating revenues. The process of estimating contractual allowances requires us to estimate the amount expected to be received based on payor contract provisions. The key assumption in this process is the estimated contractual reimbursement percentage, which is based on payor classification, historical paid claims data and, when applicable, application of the expected managed care plan reimbursement based on contract terms.
65
Due to the complexities involved in these estimates, actual payments we receive could be different from the amounts we estimate and record. If the actual contractual reimbursement percentage under government programs and managed care contracts differed by 1% at December 31, 2023 from our estimated reimbursement percentage, net income for the year ended December 31, 2023 would have changed by approximately $97 million, and net accounts receivable at December 31, 2023 would have changed by $124 million. Final settlements under some of these programs are subject to adjustment based on administrative review and audit by third parties. We account for adjustments to previous program reimbursement estimates as contractual allowance adjustments and report them in the periods that such adjustments become known. Contractual allowance adjustments related to final settlements and previous program reimbursement estimates impacted net operating revenues by an insignificant amount for each of the years ended December 31, 2023, 2022 and 2021.
Patient Accounts Receivable
Substantially all of our accounts receivable are related to providing healthcare services to patients at our hospitals and affiliated businesses. Collection of these accounts receivable is our primary source of cash and is critical to our operating performance. Our primary collection risks relate to uninsured patients and outstanding patient balances for which the primary insurance payor has paid some but not all of the outstanding balance, with the remaining outstanding balance (generally deductibles and co-payments) owed by the patient. For all procedures scheduled in advance, our policy is to verify insurance coverage prior to the date of the procedure. Insurance coverage is not verified in advance of procedures for walk-in and emergency room patients.
We estimate any adjustments to the transaction price for implicit price concessions by reserving a percentage of all self-pay accounts receivable without regard to aging category, based on collection history, adjusted for expected recoveries and any anticipated changes in trends. Our ability to estimate the transaction price and any implicit price concessions is not impacted by not utilizing an aging of our net accounts receivable as we believe that substantially all of the risk exists at the point in time such accounts are identified as self-pay. The percentage used to reserve for all self-pay accounts is based on our collection history. We believe that we collect substantially all of our third-party insured receivables, which include receivables from governmental agencies.
Patient accounts receivable can be impacted by the effectiveness of our collection efforts and, as described in our significant accounting policies included in Note 1 of the Notes to Consolidated Financial Statements included under Part II, Item 8 of this Form 10-K, numerous factors may affect the net realizable value of accounts receivable. If the actual collection percentage differed by 1% at December 31, 2023 from our estimated collection percentage as a result of a change in expected recoveries, net income for the year ended December 31, 2023 would have changed by $37 million, and net accounts receivable at December 31, 2023 would have changed by $48 million. We also continually review our overall reserve adequacy by monitoring historical cash collections as a percentage of trailing net operating revenues, as well as by analyzing current period net operating revenues and admissions by payor classification, days revenue outstanding, the composition of self-pay receivables between pure self-pay patients and the patient responsibility portion of third-party insured receivables and the impact of recent acquisitions and dispositions.
Our policy is to write-off gross accounts receivable if the balance is under $10.00 or when such amounts are placed with outside collection agencies. We believe this policy accurately reflects our ongoing collection efforts and is consistent with industry practices. We had approximately $1.7 billion at both December 31, 2023 and 2022, being pursued by various outside collection agencies. We expect to collect less than 4%, net of estimated collection fees, of the amounts being pursued by outside collection agencies. As these amounts have been written-off, they are not included in our accounts receivable. Collections on amounts previously written-off are recognized as a recovery of net operating revenues when received. However, we take into consideration estimated collections of these future amounts written-off in determining the implicit price concessions used to measure the transaction price for the applicable portfolio of patient accounts receivable.
All of the following information is derived from our hospitals, excluding clinics, unless otherwise noted.
Patient accounts receivable from our hospitals represent approximately 98% of our total consolidated accounts receivable.
Days revenue outstanding, adjusted for the impact of receivables for state Medicaid supplemental payment programs and divested facilities, was 58 days and 56 days at December 31, 2023 and 2022, respectively.
Total gross accounts receivable (prior to allowance for contractual adjustments and implicit price concessions) was approximately $16.8 billion as of December 31, 2023 and approximately $15.9 billion as of December 31, 2022. The approximate percentage of total gross accounts receivable (prior to allowance for contractual adjustments and implicit price concessions) summarized by aging categories is as follows:
66
As of December 31, 2023: |
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
% of Gross Receivables |
|
|||||||||||||
Payor |
|
0 - 90 Days |
|
|
90 - 180 Days |
|
|
180 - 365 Days |
|
|
Over 365 Days |
|
||||
Medicare |
|
|
10 |
% |
|
|
1 |
% |
|
|
1 |
% |
|
|
— |
% |
Medicare Managed Care |
|
|
16 |
% |
|
|
3 |
% |
|
|
3 |
% |
|
|
2 |
% |
Medicaid |
|
|
6 |
% |
|
|
1 |
% |
|
|
1 |
% |
|
|
1 |
% |
Other third-party payors |
|
|
18 |
% |
|
|
3 |
% |
|
|
3 |
% |
|
|
3 |
% |
Self-Pay |
|
|
7 |
% |
|
|
6 |
% |
|
|
7 |
% |
|
|
8 |
% |
As of December 31, 2022: |
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
% of Gross Receivables |
|
|||||||||||||
Payor |
|
0 - 90 Days |
|
|
90 - 180 Days |
|
|
180 - 365 Days |
|
|
Over 365 Days |
|
||||
Medicare |
|
|
11 |
% |
|
|
1 |
% |
|
|
— |
% |
|
|
— |
% |
Medicare Managed Care |
|
|
15 |
% |
|
|
3 |
% |
|
|
3 |
% |
|
|
1 |
% |
Medicaid |
|
|
7 |
% |
|
|
1 |
% |
|
|
1 |
% |
|
|
1 |
% |
Managed Care and other third-party payors |
|
|
18 |
% |
|
|
3 |
% |
|
|
3 |
% |
|
|
2 |
% |
Self-Pay |
|
|
7 |
% |
|
|
6 |
% |
|
|
8 |
% |
|
|
9 |
% |
The approximate percentage of total gross accounts receivable (prior to allowances for contractual adjustments and implicit price concessions) summarized by payor type is as follows:
|
|
December 31, |
|
|||||
|
|
2023 |
|
|
2022 |
|
||
Insured receivables |
|
|
72.1 |
% |
|
|
69.5 |
% |
Self-pay receivables |
|
|
27.9 |
|
|
|
30.5 |
|
Total |
|
|
100.0 |
% |
|
|
100.0 |
% |
The combined total at our hospitals and clinics for the estimated implicit price concessions for self-pay accounts receivable and allowances for other self-pay discounts and contractuals, as a percentage of gross self-pay receivables, was approximately 91% at both December 31, 2023 and 2022. If the receivables that have been written-off, but where collections are still being pursued by outside collection agencies, were included in both the allowances and gross self-pay receivables specified above, the percentage of combined allowances to total self-pay receivables would have been 93% at both December 31, 2023 and 2022.
Goodwill
At December 31, 2023, we had approximately $4.0 billion of goodwill recorded, all of which resides at our hospital operations reporting unit. Goodwill represents the excess of the fair value of the consideration conveyed in an acquisition over the fair value of net assets acquired. Goodwill is evaluated for impairment annually and when an event occurs or circumstances change that, more likely than not, reduce the fair value of the reporting unit below its carrying value. We performed our last annual goodwill impairment evaluation during the fourth quarter of 2023 using the October 31, 2023 measurement date, which indicated no impairment.
The determination of fair value in our goodwill impairment analysis is based on an estimate of fair value for the hospital operations reporting unit utilizing known and estimated inputs at the evaluation date. Some of those inputs include, but are not limited to, the most recent price of our common stock and fair value of our long-term debt, our recent financial results, estimates of future revenue and expense growth, estimated market multiples, expected capital expenditures, income tax rates, costs of invested capital and a discount rate.
Future estimates of fair value could be adversely affected if the actual outcome of one or more of the assumptions described above changes materially in the future, including as a result of any decline in or increased volatility of our stock price and the fair value of our long-term debt, lower than expected hospital volumes and/or net operating revenues, higher market interest rates, increased operating costs or other adverse impacts on our financial results. Such changes impacting the calculation of our fair value could result in a material impairment charge in the future.
67
Professional Liability Claims
As part of our business of providing healthcare services, we are subject to legal actions alleging liability on our part. We accrue for losses resulting from such liability claims, as well as loss adjustment expenses that are out-of-pocket and directly related to such liability claims. These direct out-of-pocket expenses include fees of outside counsel and experts. We do not accrue for costs that are part of our corporate overhead, such as the costs of our in-house legal and risk management departments. The losses resulting from professional liability claims primarily consist of estimates for known claims, as well as estimates for incurred but not reported claims. The estimates are based on specific claim facts, our historical claim reporting and payment patterns, the nature and level of our hospital operations, and actuarially determined projections. The actuarially determined projections are based on our actual claim data, including historic reporting and payment patterns, which have been gathered over the life of the Company. As discussed below, since we purchase excess insurance on a claims-made basis that transfers risk to third-party insurers, the estimated liability for professional and general liability claims does include an amount for the losses covered by our excess insurance. We also record a receivable for the expected reimbursement of losses covered by our excess insurance. Since we believe that the amount and timing of our future claims payments are reliably determinable, we discount the amount we accrue for losses resulting from professional liability claims.
The net present value of the projected payments was discounted using weighted-average interest rates of 3.7% in 2023, 3.8% in 2022 and 1.8% in 2021. This liability is adjusted for new claims information in the period such information becomes known to us. Professional liability expense includes the losses resulting from professional liability claims and loss adjustment expense, as well as excess insurance premiums, and is presented within other operating expenses in the accompanying consolidated statements of (loss) income.
Our processes for obtaining and analyzing claims and incident data are standardized across all of our businesses and have been consistent for many years. We monitor the outcomes of the medical care services that we provide and for each reported claim, we obtain various information concerning the facts and circumstances related to that claim. In addition, we routinely monitor current key statistics and volume indicators in our assessment of utilizing historical trends. The average lag period between claim occurrence and payment of a final settlement is between three and four years, although the facts and circumstances of individual claims could result in the timing of such payments being different from this average. Since claims are paid promptly after settlement with the claimant is reached, settled claims represent approximately 1% of the total liability at the end of any period.
For purposes of estimating our individual claim accruals, we utilize specific claim information, including the nature of the claim, the expected claim amount, the year in which the claim occurred and the laws of the jurisdiction in which the claim occurred. Once the case accruals for known claims are determined, information is stratified by loss layers and retentions, accident years, reported years and geography. Several actuarial methods are used against this data to produce estimates of ultimate paid losses and reserves for incurred but not reported claims. Each of these methods uses our company-specific historical claims data and other information. Company-specific data includes information regarding our business, including historical paid losses and loss adjustment expenses, historical and current case loss reserves, actual and projected hospital statistical data, a variety of hospital census information, employed physician information, professional liability retentions for each policy year, geographic information and other data. Significant assumptions are made on the basis of the aforementioned information in estimating reserves for incurred but not reported claims. A 1% change in assumptions for either severity or frequency as of December 31, 2023 would have increased or decreased the reserve between $5 million to $15 million.
Based on these analyses, we determine our estimate of the professional liability claims. The determination of management’s estimate, including the preparation of the reserve analysis that supports such estimate, involves subjective judgment of management. Changes in reserve data or the trends and factors that influence reserve data may signal fundamental shifts in our future claim development patterns or may simply reflect single-period anomalies. Even if a change reflects a fundamental shift, the full extent of the change may not become evident until years later. Moreover, since our methods and models use different types of data and we select our liability from the results of all of these methods, we typically cannot quantify the precise impact of such factors on our estimates of the liability. Due to our standardized and consistent processes for handling claims and the long history and depth of our company-specific data, our methodologies have historically produced reliably determinable estimates of ultimate paid losses. Management considers any changes in the amount and pattern of its historical paid losses up through the most recent reporting period to identify any fundamental shifts or trends in claim development experience in determining the estimate of professional liability claims. However, due to the subjective nature of this estimate and the impact that previously unforeseen shifts in actual claim experience can have, future estimates of professional liability could be adversely impacted when actual paid losses develop unexpectedly based on assumptions and settlement events that were not previously known or anticipated.
68
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Accrual for professional liability claims, beginning of year |
|
$ |
467 |
|
|
$ |
533 |
|
|
$ |
602 |
|
Liability for insured claims (1) |
|
|
17 |
|
|
|
(5 |
) |
|
|
(22 |
) |
Expense (income) related to: |
|
|
|
|
|
|
|
|
|
|||
Current accident year |
|
|
98 |
|
|
|
92 |
|
|
|
108 |
|
Prior accident years |
|
|
69 |
|
|
|
19 |
|
|
|
(18 |
) |
Expense (income) from discounting |
|
|
1 |
|
|
|
(18 |
) |
|
|
(4 |
) |
Total incurred loss and loss expense (2) |
|
|
168 |
|
|
|
93 |
|
|
|
86 |
|
Paid claims and expenses related to: |
|
|
|
|
|
|
|
|
|
|||
Current accident year |
|
|
— |
|
|
|
— |
|
|
|
(1 |
) |
Prior accident years |
|
|
(209 |
) |
|
|
(154 |
) |
|
|
(132 |
) |
Total paid claims and expenses |
|
|
(209 |
) |
|
|
(154 |
) |
|
|
(133 |
) |
Accrual for professional liability claims, end of year |
|
$ |
443 |
|
|
$ |
467 |
|
|
$ |
533 |
|
In the ordinary course of business, our expense with respect to professional liability claims, which is actuarially determined, is limited to amounts not covered by third-party insurance policies, which typically provide coverage for professional liability claims. During the year ended December 31, 2020, we incurred expenses in the amount of approximately $50 million related to the settlement of a professional liability claim for which our third-party insurers’ obligation to provide coverage to us in connection with the underlying loss was being litigated. The subject of the litigation for the recovery of the full amount of the $50 million settlement was whether the claim was covered under the subject policies. This litigation was settled during the year ended December 31, 2021, and in connection with this settlement, approximately $22 million was recovered from various third-party insurers related to their obligation to provide coverage for the professional liability claim. During the year ended December 31, 2022, we experienced an increase in the amounts paid or expected to be paid to settle outstanding professional liability claims related to divested locations, compared to the same period in the prior year and to previous actuarially determined estimates. This resulted in a change in estimate of $15 million during the three months and year ended December 31, 2022. During the year ended December 31, 2023, we experienced an increase in the amounts paid or expected to be paid to settle outstanding professional liability claims, compared to the same period in the prior year and to previous actuarially determined estimates due to adverse claim developments. There were no other significant changes in our estimate of the reserve for professional liability claims during the years ended December 31, 2023, 2022 and 2021.
We are primarily self-insured for professional liability claims; however, we obtain excess insurance that transfers the risk of loss to a third-party insurer for claims in excess of our self-insured retentions. Our excess insurance is underwritten on a claims-made basis. For claims reported prior to June 1, 2002, substantially all of our professional and general liability risks were subject to a less than $1 million per occurrence self-insured retention and for claims reported from June 1, 2002 through June 1, 2003, these self-insured retentions were $2 million per occurrence. Substantially all claims reported after June 1, 2003 and before June 1, 2005 are self-insured up to $4 million per claim. Substantially all claims reported on or after June 1, 2005 and before June 1, 2014 are self-insured up to $5 million per claim. Substantially all claims reported on or after June 1, 2014 and before June 1, 2018 are self-insured up to $10 million per claim. Substantially all claims reported on or after June 1, 2018 are self-insured up to $15 million per claim. Management, on occasion, has selectively increased the insured risk at certain hospitals based upon insurance pricing and other factors and may continue that practice in the future.
Excess insurance for all hospitals has been purchased through commercial insurance companies and generally covers us for liabilities in excess of the self-insured retentions. The excess coverage consists of multiple layers of insurance, the sum of which totals up to $95 million per occurrence and in the aggregate for claims reported on or after June 1, 2003, up to $145 million per occurrence and in the aggregate for claims reported on or after January 1, 2008, up to $195 million per occurrence and in the aggregate for claims reported on or after June 1, 2010, and up to at least $215 million per occurrence and in the aggregate for claims reported on or after June 1, 2015. In addition, for integrated occurrence professional liability claims, there is an additional $50 million of excess coverage for claims reported on or after June 1, 2014 and an additional $75 million of excess coverage for claims reported on or after June 1, 2015 through June 1, 2020. The $75 million in integrated occurrence coverage will also apply to claims reported between June 1, 2020 and June 1, 2024 for events that occurred prior to June 1, 2020 but which were not previously known or reported. For certain policy years prior to June 1, 2014, if the first aggregate layer of excess coverage becomes fully utilized, then the self-insured retention will increase to $10 million per claim for any subsequent claims in that policy year until our total aggregate coverage is met. Beginning June 1, 2018, this drop-down provision in the excess policies attaches over the $15 million per claim self-insured retention.
69
Income Taxes
We must make estimates in recording provision for income taxes, including determination of deferred tax assets and deferred tax liabilities and any valuation allowances that might be required against the deferred tax assets. We believe that future income will enable us to realize certain deferred tax assets, subject to the valuation allowance we have established.
The total amount of unrecognized benefit that would impact the effective tax rate, if recognized, was $45 million as of December 31, 2023. A total of $2 million of interest and penalties is included in the amount of liability for uncertain tax positions at December 31, 2023. It is our policy to recognize interest and penalties related to unrecognized benefits in our consolidated statements of income as income tax expense.
It is possible the amount of unrecognized tax benefit could change in the next 12 months as a result of a lapse of the statute of limitations and settlements with taxing authorities; however, we do not anticipate the change will have a material impact on our consolidated results of operations or consolidated financial position.
Our federal income tax return for the 2018 tax year is under examination by the Internal Revenue Service. We believe the result of this examination will not be material to our consolidated results of operations or consolidated financial position. In addition, we have extended our federal statute of limitations through June 30, 2025 for the tax period ended December 31, 2018.
Recent Accounting Pronouncements
In November 2023, the Financial Accounting Standards Board, or FASB, issued Accounting Standards Update, or ASU, 2023-07, “Segment Reporting (Topic 280), Improvements to Reportable Segment Disclosures.” This ASU includes additional requirements for the disclosure of significant segment expenses and segment measure(s) of profit or loss, as well as new disclosure requirements for entities with a single reportable segment and certain qualitative information about the chief operating decision maker. This ASU is effective for annual periods beginning after December 15, 2023 and interim periods beginning after December 15, 2024. The amendments in this ASU must be applied retrospectively to all periods presented. Early adoption is permitted. We are currently evaluating the impact that adoption of this ASU will have on our consolidated financial statements.
In December 2023, the FASB issued ASU 2023-09, “Income Taxes (Topic 740), Improvements to Income Tax Disclosures.” This ASU establishes new requirements for the categorization and disaggregation of information in the rate reconciliation as well as for disaggregation of income taxes paid. Additionally, this ASU modifies and eliminates certain existing requirements for indefinitely reinvested foreign earnings and unrecognized tax benefits. This ASU is effective for annual periods beginning after December 15, 2024 and interim periods beginning after December 15, 2025. The amendments in this ASU should be applied on a prospective basis and early adoption is permitted. We are currently evaluating the impact that adoption of this ASU will have on our consolidated financial statements.
We have evaluated all other recently issued, but not yet effective, ASUs and do not expect the eventual adoption of these ASUs to have a material impact on our consolidated financial position or results of operations.
FORWARD-LOOKING STATEMENTS
This Form 10-K contains forward-looking statements within the meaning of Section 27A of the Securities Act of 1933, as amended, Section 21E of the Securities Exchange Act of 1934, as amended, and the Private Securities Litigation Reform Act of 1995 that involve risk and uncertainties. Statements that are predictive in nature, that depend upon or refer to future events or conditions or that include words such as “expects,” “anticipates,” “intends,” “plans,” “believes,” “estimates,” “thinks,” and similar expressions are forward-looking statements. These statements involve known and unknown risks, uncertainties, and other factors that may cause our actual results and performance to be materially different from any future results or performance expressed or implied by these forward-looking statements. A number of factors could affect the future results of the Company or the healthcare industry generally and could cause the Company’s expected results to differ materially from those expressed in this Form 10-K. These factors include, among other things:
70
71
Although we believe that these forward-looking statements are based upon reasonable assumptions, these assumptions are inherently subject to significant regulatory, economic and competitive uncertainties and contingencies, which are difficult or impossible to predict accurately and may be beyond our control. Accordingly, we cannot give any assurance that our expectations will in fact occur, and we caution that actual results may differ materially from those in the forward-looking statements. Given these uncertainties, prospective investors are cautioned not to place undue reliance on these forward-looking statements. These forward-looking statements are made as of the date of this filing. We undertake no obligation to revise or update any forward-looking statements, or to make any other forward-looking statements, whether as a result of new information, future events or otherwise.
Item 7A. Quantitative and Qualitative Disclosures about Market Risk
We are exposed to market risk related to changes in market value of marketable securities including debt and equity securities held by our wholly-owned captive insurance subsidiaries as well as securities held for certain deferred compensation plans. Available-for-sale debt securities are reported at fair value as determined by quoted market prices, with unrealized gains and losses reported as a separate component of stockholders’ deficit. Trading securities are reported at fair value with unrealized gains and losses included in earnings. Other comprehensive income, net of tax, included an unrealized gain of $6 million during the year ended December 31, 2023.
We are exposed to market risk related to market illiquidity. Investments in debt and equity securities of our insurance subsidiaries could be impaired by the inability to access the capital markets. Should the insurance subsidiaries require significant amounts of cash in excess of normal cash requirements to pay claims and other expenses on short notice, we may have difficulty selling these investments in a timely manner or be forced to sell them at a price less than what we might otherwise have been able to in a normal market environment. We may be required to recognize credit-related impairments on our investment securities in future periods should issuers default on interest payments or should the fair market valuations of the securities deteriorate due to ratings downgrades or other issue-specific factors.
We are also exposed to market risk related to changes in interest rates, primarily as a result of the ABL Facility, which bears interest based on floating rates. At December 31, 2023, we had outstanding borrowings of $247 million under the ABL Facility.
The estimated fair value of our long-term debt, excluding finance leases, was approximately $9.6 billion at December 31, 2023. The estimates of fair value are based upon the quoted market prices for the same or similar issues of long-term debt with the same maturities. Based on a hypothetical 1% increase in interest rates, the potential annualized reduction to future pre-tax earnings would be approximately $118 million. To mitigate the impact of fluctuations in interest rates, we generally target a majority of our debt portfolio to be maintained at fixed rates.
72
Item 8. Financial Statements and Supplementary Data
Index to Financial Statements
|
|
Page |
Community Health Systems, Inc. Consolidated Financial Statements: |
|
|
Report of Independent Registered Public Accounting Firm (PCAOB ID No. |
|
74 |
Consolidated Statements of (Loss) Income for the Years Ended December 31, 2023, 2022 and 2021 |
|
77 |
|
78 |
|
Consolidated Balance Sheets as of December 31, 2023 and 2022 |
|
79 |
|
80 |
|
Consolidated Statements of Cash Flows for the Years Ended December 31, 2023, 2022 and 2021 |
|
81 |
|
82 |
73
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the stockholders and the Board of Directors of Community Health Systems, Inc.
Opinion on the Financial Statements
We have audited the accompanying consolidated balance sheets of Community Health Systems, Inc. and subsidiaries (the “Companyˮ) as of December 31, 2023 and 2022, the related consolidated statements of (loss) income, comprehensive (loss) income, stockholders’ deficit, and cash flows, for each of the three years in the period ended December 31, 2023, and the related notes (collectively referred to as the “financial statementsˮ). In our opinion, the financial statements present fairly, in all material respects, the financial position of the Company as of December 31, 2023 and 2022, and the results of its operations and its cash flows for each of the three years in the period ended December 31, 2023, in conformity with accounting principles generally accepted in the United States of America.
We have also audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the Company's internal control over financial reporting as of December 31, 2023, based on criteria established in Internal Control — Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission and our report dated February 21, 2024 expressed an unqualified opinion on the Company's internal control over financial reporting.
Basis for Opinion
These financial statements are the responsibility of the Company's management. Our responsibility is to express an opinion on the Company's financial statements based on our audits. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
Critical Audit Matters
The critical audit matters communicated below are matters arising from the current-period audit of the financial statements that were communicated or required to be communicated to the audit committee and that (1) relate to accounts or disclosures that are material to the financial statements and (2) involved our especially challenging, subjective, or complex judgments. The communication of critical audit matters does not alter in any way our opinion on the financial statements, taken as a whole, and we are not, by communicating the critical audit matters below, providing separate opinions on the critical audit matters or on the accounts or disclosures to which they relate.
Patient Accounts Receivable — Refer to Note 1 to the financial statements
Critical Audit Matter Description
Patient accounts receivable are recorded net of implicit price concessions for insured and self-pay patients. The Company’s primary collection risks relate to uninsured patients and outstanding patient balances for which the primary insurance payor has paid some, but not all of the outstanding balance, with the remaining outstanding balance (generally deductibles and co-payments) owed by the patient. The Company estimates any adjustments to the transaction price for implicit price concessions by reserving a percentage of all self-pay accounts receivable without regard to aging category, based on collection history, adjusted for expected recoveries and any anticipated changes in trends.
74
Given that auditing management’s estimate of self-pay price concessions was complex and judgmental due to the significant data inputs and subjective assumptions utilized in determining related amounts, performing audit procedures to evaluate whether the self-pay price concessions were appropriately recorded as of December 31, 2023, required a high degree of auditor judgment and an increased extent of effort.
How the Critical Audit Matter Was Addressed in the Audit
Our audit procedures related to the net realizable value of self-pay accounts receivable included the following, among others:
Professional Liability Claims — Refer to Note 15 to the financial statements
Critical Audit Matter Description
As part of the Company’s business of providing health care services, they are subject to legal actions alleging liability on their part. The Company accrues for losses resulting from such liability claims, as well as loss adjustment expenses that are out-of-pocket and directly related to such liability claims. These direct out-of-pocket expenses include fees of outside counsel and experts.
The Company is self-insured for professional liability claims up to certain self-insured retention limits based on the policy year. Professional liabilities consist of the projected settlement value of reported and unreported claims. The self-insurance reserves are estimated based on the Company’s historical claims experience, supplemented with industry experience, as necessary, and is established using actuarial methods followed in the insurance industry.
Given the subjectivity of estimating the projected settlement value of reported and unreported claims, performing audit procedures to evaluate whether professional liability claims were appropriately recorded as of December 31, 2023, required a high degree of auditor judgment and an increased extent of effort, including the need to involve our actuarial specialists.
How the Critical Audit Matter Was Addressed in the Audit
Our audit procedures related to the self-insured professional liability claims included the following, among others:
75
Goodwill Impairment – Refer to Notes 1 and 4 to the financial statements
Critical Audit Matter Description
Goodwill is evaluated for impairment annually and when an event occurs or circumstances change that, more likely than not, reduce the fair value of the reporting unit below its' carrying value. The Company estimates the fair value of the reporting unit using both a discounted cash flow model as well as a market multiple model.
The determination of fair value using the discounted cash flow model requires management to make significant estimates and assumptions related to forecasts of revenue growth rates, EBITDA (earnings before interest, income taxes, and depreciation and amortization) margins, and a discount rate. The determination of fair value using the market multiple model requires management to make significant assumptions related to revenue and EBITDA multiples. The fair value of the Company’s hospital reporting unit exceeded the carrying value as of the annual measurement date of October 31st and, therefore, no impairment was recognized.
Given the significant estimates and assumptions management makes to estimate the fair value of the hospital reporting unit and the sensitivity of such assumptions, performing audit procedures to evaluate the reasonableness of management’s estimates and assumptions related to forecasts of future revenues, EBITDA margins, and revenue and EBITDA multiples, and the selection of the discount rates for the hospital reporting unit required a high degree of auditor judgment and an increased extent of effort, including the need to involve our fair value specialists.
How the Critical Audit Matter Was Addressed in the Audit
Our audit procedures related to the fair value of the hospital reporting unit included the following, among others:
/s/
February 21, 2024
We have served as the Company’s auditor since 1996.
76
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF (LOSS) INCOME
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
|
|
(In millions, except share and per share data) |
|
|||||||||
Net operating revenues |
|
$ |
|
|
$ |
|
|
$ |
|
|||
Operating costs and expenses: |
|
|
|
|
|
|
|
|
|
|||
Salaries and benefits |
|
|
|
|
|
|
|
|
|
|||
Supplies |
|
|
|
|
|
|
|
|
|
|||
Other operating expenses |
|
|
|
|
|
|
|
|
|
|||
Lease cost and rent |
|
|
|
|
|
|
|
|
|
|||
Pandemic relief funds |
|
|
— |
|
|
|
( |
) |
|
|
( |
) |
Depreciation and amortization |
|
|
|
|
|
|
|
|
|
|||
Impairment and (gain) loss on sale of businesses, net |
|
|
( |
) |
|
|
|
|
|
|
||
Total operating costs and expenses |
|
|
|
|
|
|
|
|
|
|||
Income from operations |
|
|
|
|
|
|
|
|
|
|||
Interest expense, net of interest income of $ |
|
|
|
|
|
|
|
|
|
|||
(Gain) loss from early extinguishment of debt |
|
|
( |
) |
|
|
( |
) |
|
|
|
|
Gain on sale of equity interests in Macon Healthcare, LLC |
|
|
— |
|
|
|
— |
|
|
|
( |
) |
Gain from CoreTrust Transaction |
|
|
— |
|
|
|
( |
) |
|
|
— |
|
Equity in earnings of unconsolidated affiliates |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Income before income taxes |
|
|
|
|
|
|
|
|
|
|||
Provision for income taxes |
|
|
|
|
|
|
|
|
|
|||
Net income |
|
|
|
|
|
|
|
|
|
|||
Less: Net income attributable to noncontrolling interests |
|
|
|
|
|
|
|
|
|
|||
Net (loss) income attributable to Community Health |
|
$ |
( |
) |
|
$ |
|
|
$ |
|
||
(Loss) earnings per share attributable to Community Health Systems, |
|
|
|
|
|
|
|
|
|
|||
Basic |
|
$ |
( |
) |
|
$ |
|
|
$ |
|
||
Diluted |
|
$ |
( |
) |
|
$ |
|
|
$ |
|
||
Weighted-average number of shares outstanding: |
|
|
|
|
|
|
|
|
|
|||
Basic |
|
|
|
|
|
|
|
|
|
|||
Diluted |
|
|
|
|
|
|
|
|
|
|||
See accompanying notes to the consolidated financial statements.
77
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF COMPREHENSIVE (LOSS) INCOME
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
|
|
|
|
|
(In millions) |
|
|
|
|
|||
Net income |
|
$ |
|
|
$ |
|
|
$ |
|
|||
Other comprehensive income (loss), net of income taxes: |
|
|
|
|
|
|
|
|
|
|||
Net change in fair value of available-for-sale debt securities, net |
|
|
|
|
|
( |
) |
|
|
( |
) |
|
Amortization and recognition of unrecognized pension cost |
|
|
|
|
|
|
|
|
|
|||
Other comprehensive income (loss) |
|
|
|
|
|
( |
) |
|
|
( |
) |
|
Comprehensive income |
|
|
|
|
|
|
|
|
|
|||
Less: Comprehensive income attributable to noncontrolling interests |
|
|
|
|
|
|
|
|
|
|||
Comprehensive (loss) income attributable to Community Health Systems, |
|
$ |
( |
) |
|
$ |
|
|
$ |
|
||
See accompanying notes to the consolidated financial statements.
78
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
CONSOLIDATED BALANCE SHEETS
|
|
December 31, |
|
|
December 31, |
|
||
|
|
(In millions, except share data) |
|
|||||
ASSETS |
|
|
|
|
|
|
||
Current assets: |
|
|
|
|
|
|
||
Cash and cash equivalents |
|
$ |
|
|
$ |
|
||
Patient accounts receivable (Note 1) |
|
|
|
|
|
|
||
Supplies |
|
|
|
|
|
|
||
Prepaid income taxes |
|
|
|
|
|
|
||
Prepaid expenses and taxes |
|
|
|
|
|
|
||
Other current assets |
|
|
|
|
|
|
||
Total current assets |
|
|
|
|
|
|
||
Property and equipment |
|
|
|
|
|
|
||
Land and improvements |
|
|
|
|
|
|
||
Buildings and improvements |
|
|
|
|
|
|
||
Equipment and fixtures |
|
|
|
|
|
|
||
Property and equipment |
|
|
|
|
|
|
||
Less accumulated depreciation and amortization |
|
|
( |
) |
|
|
( |
) |
Property and equipment, net |
|
|
|
|
|
|
||
Goodwill |
|
|
|
|
|
|
||
Deferred income taxes |
|
|
|
|
|
|
||
Other assets, net of accumulated amortization of $ |
|
|
|
|
|
|
||
Total assets |
|
$ |
|
|
$ |
|
||
LIABILITIES AND STOCKHOLDERS’ DEFICIT |
|
|
|
|
|
|
||
Current liabilities: |
|
|
|
|
|
|
||
Current maturities of long-term debt |
|
$ |
|
|
$ |
|
||
Current operating lease liabilities |
|
|
|
|
|
|
||
Accounts payable |
|
|
|
|
|
|
||
Accrued liabilities: |
|
|
|
|
|
|
||
Employee compensation |
|
|
|
|
|
|
||
Accrued interest |
|
|
|
|
|
|
||
Other |
|
|
|
|
|
|
||
Total current liabilities |
|
|
|
|
|
|
||
Long-term debt |
|
|
|
|
|
|
||
Deferred income taxes |
|
|
|
|
|
|
||
Long-term operating lease liabilities |
|
|
|
|
|
|
||
Other long-term liabilities |
|
|
|
|
|
|
||
Total liabilities |
|
|
|
|
|
|
||
Redeemable noncontrolling interests in equity of consolidated subsidiaries |
|
|
|
|
|
|
||
(Note 15) |
|
|
|
|
|
|
||
STOCKHOLDERS’ DEFICIT |
|
|
|
|
|
|
||
Community Health Systems, Inc. stockholders’ deficit: |
|
|
|
|
|
|
||
Preferred stock, $ |
|
|
— |
|
|
|
— |
|
Common stock, $ |
|
|
|
|
|
|
||
Additional paid-in capital |
|
|
|
|
|
|
||
Accumulated other comprehensive loss |
|
|
( |
) |
|
|
( |
) |
Accumulated deficit |
|
|
( |
) |
|
|
( |
) |
Total Community Health Systems, Inc. stockholders’ deficit |
|
|
( |
) |
|
|
( |
) |
Noncontrolling interests in equity of consolidated subsidiaries |
|
|
|
|
|
|
||
Total stockholders’ deficit |
|
|
( |
) |
|
|
( |
) |
Total liabilities and stockholders’ deficit |
|
$ |
|
|
$ |
|
||
See accompanying notes to the consolidated financial statements.
79
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF STOCKHOLDERS’ DEFICIT
|
|
|
|
|
|
Community Health Systems, Inc. Stockholders |
|
|
|
|
|
|
|
||||||||||||||||||||
|
|
Redeemable |
|
|
|
Common Stock |
|
|
Additional |
|
|
Accumulated |
|
|
Accumulated |
|
|
Noncontrolling |
|
|
Total |
|
|||||||||||
|
|
Interests |
|
|
|
Shares |
|
|
Amount |
|
|
Capital |
|
|
Loss |
|
|
Deficit |
|
|
Interests |
|
|
Deficit |
|
||||||||
|
|
|
|
|
|
(In millions, except share data) |
|
||||||||||||||||||||||||||
Balance, December 31, 2020 |
|
$ |
|
|
|
|
|
|
$ |
|
|
$ |
|
|
$ |
( |
) |
|
$ |
( |
) |
|
$ |
|
|
$ |
( |
) |
|||||
Comprehensive income (loss) |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
|
|
|
|
|
|
|
|
||||
Contributions from noncontrolling interests |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
Distributions to noncontrolling interests |
|
|
( |
) |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
|
( |
) |
Purchase of subsidiary shares from noncontrolling interests |
|
|
( |
) |
|
|
|
— |
|
|
|
— |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
|
|
||
Other reclassifications of noncontrolling interests |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
|
|||
Disposition of less-than-wholly owned hospital |
|
|
( |
) |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
Noncontrolling interests in acquired entity |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
Adjustment to redemption value of redeemable |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
Cancellation of restricted stock for tax withholdings on |
|
|
— |
|
|
|
|
( |
) |
|
|
— |
|
|
|
( |
) |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
Issuance of common stock in connection with the exercise |
|
|
— |
|
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
Stock-based compensation |
|
|
— |
|
|
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
|
|||
Balance, December 31, 2021 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
( |
) |
|
|
( |
) |
|
|
|
|
|
( |
) |
|||||
Comprehensive income (loss) |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
|
|
|
|
|
|
|
|
||||
Contributions from noncontrolling interests |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
|
|
|
|
|||
Distributions to noncontrolling interests |
|
|
( |
) |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
|
( |
) |
Purchase of subsidiary shares from noncontrolling interests |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
Noncontrolling interests in acquired entity |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
|
|
|
|
|||
Adjustment to redemption value of redeemable |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
Cancellation of restricted stock for tax withholdings on |
|
|
— |
|
|
|
|
( |
) |
|
|
— |
|
|
|
( |
) |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
Issuance of common stock in connection with the exercise |
|
|
— |
|
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
Stock-based compensation |
|
|
— |
|
|
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
|
|||
Balance, December 31, 2022 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
( |
) |
|
|
( |
) |
|
|
|
|
|
( |
) |
|||||
Comprehensive income (loss) |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
|
|
|
( |
) |
|
|
|
|
|
( |
) |
|||
Contributions from noncontrolling interests |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
|
|
|
|
|||
Distributions to noncontrolling interests |
|
|
( |
) |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
|
( |
) |
Purchase of subsidiary shares from noncontrolling interests |
|
|
( |
) |
|
|
|
— |
|
|
|
— |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
|
||
Other reclassifications of noncontrolling interests |
|
|
( |
) |
|
|
|
— |
|
|
|
— |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
|
|
|
|
|||
Noncontrolling interests in acquired entity |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
Adjustment to redemption value of redeemable |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
Cancellation of restricted stock for tax withholdings on |
|
|
— |
|
|
|
|
( |
) |
|
|
— |
|
|
|
( |
) |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
Issuance of common stock in connection with the exercise |
|
|
— |
|
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
Stock-based compensation |
|
|
— |
|
|
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
|
|||
Balance, December 31, 2023 |
|
$ |
|
|
|
|
|
|
$ |
|
|
$ |
|
|
$ |
( |
) |
|
$ |
( |
) |
|
$ |
|
|
$ |
( |
) |
|||||
See accompanying notes to the consolidated financial statements.
80
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CASH FLOWS
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
|
|
(In millions) |
|
|||||||||
Cash flows from operating activities: |
|
|
|
|
|
|
|
|
|
|||
Net income |
|
$ |
|
|
$ |
|
|
$ |
|
|||
Adjustments to reconcile net income to net cash provided by |
|
|
|
|
|
|
|
|
|
|||
Depreciation and amortization |
|
|
|
|
|
|
|
|
|
|||
Deferred income taxes |
|
|
|
|
|
|
|
|
|
|||
Stock-based compensation expense |
|
|
|
|
|
|
|
|
|
|||
Impairment and (gain) loss on sale of businesses, net |
|
|
( |
) |
|
|
|
|
|
|
||
(Gain) loss from early extinguishment of debt |
|
|
( |
) |
|
|
( |
) |
|
|
|
|
Gain on sale of equity interests in Macon Healthcare, LLC |
|
|
— |
|
|
|
— |
|
|
|
( |
) |
Gain from CoreTrust Transaction |
|
|
— |
|
|
|
( |
) |
|
|
— |
|
Other non-cash expenses, net |
|
|
|
|
|
|
|
|
|
|||
Changes in operating assets and liabilities, net of effects of acquisitions |
|
|
|
|
|
|
|
|
|
|||
Patient accounts receivable |
|
|
( |
) |
|
|
|
|
|
( |
) |
|
Supplies, prepaid expenses and other current assets |
|
|
( |
) |
|
|
( |
) |
|
|
|
|
Repayment/derecognition of Medicare accelerated payments |
|
|
— |
|
|
|
— |
|
|
|
( |
) |
Accounts payable, accrued liabilities and income taxes |
|
|
( |
) |
|
|
( |
) |
|
|
|
|
Other |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Net cash provided by (used in) operating activities |
|
|
|
|
|
|
|
|
( |
) |
||
Cash flows from investing activities: |
|
|
|
|
|
|
|
|
|
|||
Acquisitions of facilities and other related businesses |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Purchases of property and equipment |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Proceeds from disposition of hospitals and other ancillary operations |
|
|
|
|
|
|
|
|
|
|||
Proceeds from sale of property and equipment |
|
|
|
|
|
|
|
|
|
|||
Purchases of available-for-sale debt securities and equity securities |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Proceeds from sales of available-for-sale debt securities and equity |
|
|
|
|
|
|
|
|
|
|||
Purchases of investments in unconsolidated affiliates |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Proceeds from sale of equity interests in Macon Healthcare, LLC |
|
|
— |
|
|
|
— |
|
|
|
|
|
Distribution of CoreTrust Transaction proceeds |
|
|
— |
|
|
|
|
|
|
— |
|
|
Increase in other investments |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Net cash used in investing activities |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Cash flows from financing activities: |
|
|
|
|
|
|
|
|
|
|||
Repurchase of restricted stock shares for payroll tax withholding |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Deferred financing costs and other debt-related costs |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Proceeds from noncontrolling investors in joint ventures |
|
|
|
|
|
|
|
|
— |
|
||
Redemption of noncontrolling investments in joint ventures |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Distributions to noncontrolling investors in joint ventures |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Other borrowings |
|
|
|
|
|
|
|
|
|
|||
Issuance of long-term debt |
|
|
|
|
|
|
|
|
|
|||
Proceeds from ABL Facility |
|
|
|
|
|
|
|
|
— |
|
||
Repayments of long-term indebtedness |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Net cash used in financing activities |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Net change in cash and cash equivalents |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Cash and cash equivalents at beginning of period |
|
|
|
|
|
|
|
|
|
|||
Cash and cash equivalents at end of period |
|
$ |
|
|
$ |
|
|
$ |
|
|||
Supplemental disclosure of cash flow information: |
|
|
|
|
|
|
|
|
|
|||
Interest payments |
|
$ |
( |
) |
|
$ |
( |
) |
|
$ |
( |
) |
Income tax (payments) refunds, net |
|
$ |
( |
) |
|
$ |
( |
) |
|
$ |
( |
) |
See accompanying notes to the consolidated financial statements.
81
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
1. BASIS OF PRESENTATION AND SIGNIFICANT ACCOUNTING POLICIES
Business. Community Health Systems, Inc. is a holding company and operates no business in its own name. On a consolidated basis, Community Health Systems, Inc. and its subsidiaries (collectively the “Company”) own, lease and operate general acute care hospitals as well as outpatient facilities in communities across the country. As of December 31, 2023, the Company’s subsidiaries own or lease
As of December 31, 2023, Indiana, Alabama, Texas and Florida represent the only areas of significant geographic concentration. Net operating revenues generated by the Company’s hospitals in Indiana, as a percentage of consolidated net operating revenues, were
Use of Estimates. The preparation of financial statements in conformity with U.S. generally accepted accounting principles (“U.S. GAAP”) requires management to make estimates and assumptions that affect the amounts reported in the consolidated financial statements. Actual results could differ from these estimates under different assumptions or conditions.
Principles of Consolidation. The consolidated financial statements include the accounts of the Parent Company, its subsidiaries, all of which are controlled by the Parent Company through majority voting control, and variable interest entities for which the Company is the primary beneficiary. All intercompany accounts, profits and transactions have been eliminated. Noncontrolling interests in less-than-wholly-owned consolidated subsidiaries of the Parent Company are presented as a component of total equity to distinguish between the interests of the Parent Company and the interests of the noncontrolling owners. Revenues, expenses and income from these subsidiaries are included in the consolidated amounts as presented in the consolidated statements of (loss) income, along with a net income measure that separately presents the amounts attributable to the controlling interests and the amounts attributable to the noncontrolling interests for each of the periods presented. Noncontrolling interests that are redeemable or may become redeemable at a fixed or determinable price at the option of the holder or upon the occurrence of an event outside of the control of the Company are presented in mezzanine equity in the consolidated balance sheets.
Cost of Revenue. Substantially all of the Company’s operating costs and expenses are “cost of revenue” items. Operating costs that could be classified as general and administrative by the Company would include the Company’s corporate office costs at its Franklin, Tennessee office, which were collectively $
Cash Equivalents. The Company considers highly liquid investments with original maturities of three months or less to be cash equivalents.
Supplies. Supplies, principally medical supplies, are stated at the lower of cost (first-in, first-out basis) or market.
Marketable Securities. The Company’s marketable securities consist of debt securities that are classified as trading or available-for-sale and equity securities. Available-for-sale debt securities are reported at fair value as determined by quoted market prices, with unrealized gains and losses reported as a separate component of stockholders’ deficit. Trading securities are reported at fair value with unrealized gains and losses included in earnings. Other comprehensive income (loss), net of tax, included an unrealized gain of $
Property and Equipment. Property and equipment are recorded at cost. Depreciation is recognized using the straight-line method over the estimated useful lives of the land and improvements (
82
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Interest capitalized related to construction in progress was $
The Company also leases certain facilities and equipment under finance leases (see Note 9). Such assets are amortized on a straight-line basis over the lesser of the term of the lease or the remaining useful lives of the applicable assets. During the year ended December 31, 2023, the Company had non-cash investing activity of $
Goodwill. Goodwill represents the excess of the fair value of the consideration conveyed in the acquisition over the fair value of net assets acquired. Goodwill arising from business combinations is not amortized. Goodwill is required to be evaluated for impairment at the same time every year and when an event occurs or circumstances change such that it is more likely than not that impairment may exist. The Company performs its annual testing of impairment for goodwill in the fourth quarter of each year. There was
Net Operating Revenues
Net operating revenues are recorded at the transaction price estimated by the Company to reflect the total consideration due from patients and third-party payors in exchange for providing goods and services in patient care. These services are considered to be a single performance obligation and have a duration of less than one year. Revenues are recorded as these goods and services are provided. The transaction price, which involves significant estimates, is determined based on the Company’s standard charges for the goods and services provided, with a reduction recorded for price concessions related to third-party contractual arrangements as well as patient discounts and other patient price concessions. During each of the years ended December 31, 2023, 2022 and 2021, the impact of changes to the inputs used to determine the transaction price was considered immaterial.
Currently, several states utilize supplemental reimbursement programs for the purpose of providing reimbursement to providers that is not specifically tied to an individual’s care, some of which offsets a portion of the cost of providing care to Medicaid and indigent patients. These programs are authorized by Centers for Medicare & Medicaid Services (“CMS”) and are funded with a combination of state and federal resources, including, in certain instances, fees or taxes levied on the providers. Under these supplemental programs, the Company recognizes revenue and related expenses in the period in which amounts are estimable and payment is reasonably assured. Reimbursement under these programs is reflected in net operating revenues. Taxes or other program-related costs are reflected in other operating expenses.
The Company’s net operating revenues during the years ended December 31, 2023, 2022 and 2021 have been presented in the following table based on an allocation of the estimated transaction price with the patient between the primary patient classification of insurance coverage (in millions):
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Medicare |
|
$ |
|
|
$ |
|
|
$ |
|
|||
Medicare Managed Care |
|
|
|
|
|
|
|
|
|
|||
Medicaid |
|
|
|
|
|
|
|
|
|
|||
Managed Care and other third-party payors |
|
|
|
|
|
|
|
|
|
|||
Self-pay |
|
|
|
|
|
|
|
|
|
|||
Total |
|
$ |
|
|
$ |
|
|
$ |
|
|||
83
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Patient Accounts Receivable
Patient accounts receivable are recorded at net realizable value based on certain assumptions determined by each payor. For third-party payors including Medicare, Medicare Managed Care, Medicaid and Managed Care, the net realizable value is based on the estimated contractual reimbursement percentage, which is based on current contract prices or historical paid claims data by payor. For self-pay accounts receivable, which includes patients who are uninsured and the patient responsibility portion for patients with insurance, the net realizable value is determined using estimates of historical collection experience without regard to aging category. These estimates are adjusted for estimated conversions of patient responsibility portions, expected recoveries and any anticipated changes in trends.
Patient accounts receivable can be impacted by the effectiveness of the Company’s collection efforts. Additionally, significant changes in payor mix, business office operations, economic conditions or trends in federal and state governmental healthcare coverage could affect the net realizable value of accounts receivable. The Company also continually reviews the net realizable value of accounts receivable by monitoring historical cash collections as a percentage of trailing net operating revenues, as well as by analyzing current period net operating revenues and admissions by payor classification, days revenue outstanding, the composition of self-pay receivables between pure self-pay patients and the patient responsibility portion of third-party insured receivables, the impact of recent acquisitions and dispositions and the impact of current macroeconomic conditions and other events.
Final settlements for some payors and programs are subject to adjustment based on administrative review and audit by third parties. As a result of these final settlements, the Company has recorded amounts due to third-party payors of $
Charity Care
In the ordinary course of business, the Company renders services to patients who are financially unable to pay for hospital care. The Company’s policy is to not pursue collections for such amounts; therefore, the related charges for those patients who are financially unable to pay and that otherwise do not qualify for reimbursement from a governmental program are not reported in net operating revenues, and are thus classified as charity care. The Company determines amounts that qualify for charity care based on the patient’s household income relative to the federal poverty level guidelines, as established by the federal government.
These charity care services are estimated to be $
Leases. Leases are recorded in the consolidated balance sheets through recognition of a liability for the discounted present value of future fixed lease payments and a corresponding ROU asset. The ROU asset recorded at commencement of the lease represents the right to use the underlying asset over the lease term in exchange for the lease payments. Leases with an initial term of 12 months or less that do not have an option to purchase the underlying asset that is deemed reasonably certain to be exercised are not recorded in the consolidated balance sheets; rather, rent expense for these leases is recognized on a straight-line basis over the lease term, or when incurred if a month-to-month lease. When readily determinable, the Company uses the interest rate implicit in a lease to determine the present value of future lease payments. For leases where the implicit rate is not readily determinable, the Company’s incremental borrowing rate is utilized. The Company calculates its incremental borrowing rate on a quarterly basis using a third-party financial model that estimates the rate of interest the Company would have to pay to borrow an amount equal to the total lease payments on a collateralized basis over a term similar to the lease. The Company’s lease agreements do not contain any material residual value guarantees or material restrictive covenants.
84
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Physician Income Guarantees. The Company enters into physician recruiting agreements under which it supplements physician income to a minimum amount over a period of time, typically
Concentrations of Credit Risk. The Company grants unsecured credit to its patients, most of whom reside in the service area of the Company’s facilities and are insured under third-party payor agreements. Because of the economic diversity of the Company’s facilities and non-governmental third-party payors, Medicare represents the only significant concentration of credit risk from payors. Accounts receivable, net of contractual allowances, from Medicare was $
Accounting for the Impairment or Disposal of Long-Lived Assets. During the year ended December 31, 2023, the Company recorded a net gain of approximately $
During the year ended December 31, 2022, the Company recorded an impairment charge of approximately $
Income Taxes. The Company accounts for income taxes under the asset and liability method, in which deferred income tax assets and liabilities are recognized for the tax consequences of “temporary differences” by applying enacted statutory tax rates applicable to future years to differences between the financial statement carrying amounts and the tax bases of existing assets and liabilities. The effect on deferred taxes of a change in tax rates is recognized in the consolidated statements of (loss) income during the period in which the tax rate change becomes law.
Other Comprehensive Loss. Other comprehensive loss is the change in equity of a business enterprise during a period from transactions and other events and circumstances from non-owner sources.
Segment Reporting. A public company is required to report annual and interim financial and descriptive information about its reportable operating segments. Operating segments, as defined, are components of an enterprise about which separate financial information is available that is evaluated regularly by the chief operating decision maker in deciding how to allocate resources and in assessing performance. Aggregation of similar operating segments into a single reportable operating segment is permitted if the businesses have similar economic characteristics and meet the criteria established by U.S. GAAP. The Company operates a single operating segment represented by hospital operations (which includes the Company's acute care hospitals and related healthcare entities that provide inpatient and outpatient healthcare services).
CO
85
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
The Company received pandemic relief fund payments through various federal, state and local programs of approximately $
New Accounting Pronouncements. In November 2023, the Financial Accounting Standards Board (“FASB”) issued Accounting Standards Update (“ASU”) 2023-07, “Segment Reporting (Topic 280), Improvements to Reportable Segment Disclosures.” This ASU includes additional requirements for the disclosure of significant segment expenses and segment measure(s) of profit or loss, as well as new disclosure requirements for entities with a single reportable segment and certain qualitative information about the chief operating decision maker. This ASU is effective for annual periods beginning after December 15, 2023 and interim periods beginning after December 15, 2024. The amendments in this ASU must be applied retrospectively to all periods presented. Early adoption is permitted. The Company is currently evaluating the impact that
In December 2023, the FASB issued ASU 2023-09, “Income Taxes (Topic 740), Improvements to Income Tax Disclosures.” This ASU establishes new requirements for the categorization and disaggregation of information in the rate reconciliation as well as for disaggregation of income taxes paid. Additionally, this ASU modifies and eliminates certain existing requirements for indefinitely reinvested foreign earnings and unrecognized tax benefits. This ASU is effective for annual periods beginning after December 15, 2024 and interim periods beginning after December 15, 2025. The amendments in this ASU should be applied on a prospective basis and early adoption is permitted. The Company is currently evaluating the impact that adoption of this ASU will have on its consolidated financial statements.
The Company has evaluated all other recently issued, but not yet effective, ASUs and does not expect the eventual adoption of these ASUs to have a
2. ACCOUNTING FOR STOCK-BASED COMPENSATION
Stock-based compensation awards have been granted under the Community Health Systems, Inc. Amended and Restated 2009 Stock Option and Award Plan, which was most recently amended and restated as of March 22, 2023 and most recently approved by the Company’s stockholders at the annual meeting of stockholders held on May 9, 2023 (the “2009 Plan”).
The 2009 Plan provides for the grant of incentive stock options intended to qualify under Section 422 of the Internal Revenue Code (“IRC”) and for the grant of stock options which do not so qualify, stock appreciation rights, restricted stock, restricted stock units (“RSUs”), performance-based shares or units and other share awards. Persons eligible to receive grants under the 2009 Plan include the Company’s directors, officers, employees and consultants. To date, all options granted under the 2009 Plan have been “nonqualified” stock options for tax purposes. Generally, these options vest in
The following table reflects the impact of total compensation expense related to stock-based equity plans on the reported operating results for the respective periods (in millions):
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Effect on income before income taxes |
|
$ |
( |
) |
|
$ |
( |
) |
|
$ |
( |
) |
Effect on net income |
|
$ |
( |
) |
|
$ |
( |
) |
|
$ |
( |
) |
At December 31, 2023, $
86
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
The fair value of stock options was estimated using the Black Scholes option pricing model with the following assumptions and weighted-average fair values during the years ended December 31, 2023, 2022 and 2021:
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Expected volatility |
|
|
|
|
|
|
||||||
Expected dividends |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Expected term |
|
|
|
|
|
|
||||||
Risk-free interest rate |
|
|
|
|
|
|
||||||
In determining the expected term, the Company examined concentrations of option holdings and historical patterns of option exercises and forfeitures, as well as forward-looking factors, in an effort to determine if there were any discernible employee populations. From this analysis, in determining the expected term for the year ended December 31, 2023, the Company identified one population, consisting of persons receiving grants of stock options. Additionally, in determining the expected term for the years ended December 31, 2022 and 2021, two populations were identified, one consisting of certain senior executives who have since retired as executive officers, and the other consisting of substantially all other recipients.
The expected volatility rate was estimated based on historical volatility. In determining expected volatility, the Company also reviewed the market-based implied volatility of actively traded options of its common stock and determined that historical volatility utilized to estimate the expected volatility rate did not differ significantly from the implied volatility.
The expected term computation is based on historical exercise and cancellation patterns and forward-looking factors, where present, for each population identified. The risk-free interest rate is based on the U.S. Treasury yield curve in effect at the time of the grant. The pre-vesting forfeiture rate is based on historical rates and forward-looking factors for each population identified. The Company adjusts the estimated forfeiture rate to its actual experience.
Options outstanding and exercisable under the 2009 Plan as of December 31, 2023, and changes during each of the years in the three-year period prior to December 31, 2023, were as follows (in millions, except share and per share data):
|
|
Shares |
|
|
Weighted- |
|
|
Weighted- |
|
Aggregate |
|
|||
Outstanding at December 31, 2020 |
|
|
|
|
$ |
|
|
|
|
|
|
|||
Granted |
|
|
|
|
|
|
|
|
|
|
|
|||
Exercised |
|
|
( |
) |
|
|
|
|
|
|
|
|
||
Forfeited and cancelled |
|
|
( |
) |
|
|
|
|
|
|
|
|
||
Outstanding at December 31, 2021 |
|
|
|
|
|
|
|
|
|
|
|
|||
Granted |
|
|
|
|
|
|
|
|
|
|
|
|||
Exercised |
|
|
( |
) |
|
|
|
|
|
|
|
|
||
Forfeited and cancelled |
|
|
( |
) |
|
|
|
|
|
|
|
|
||
Outstanding at December 31, 2022 |
|
|
|
|
|
|
|
|
|
|
|
|||
Granted |
|
|
|
|
|
|
|
|
|
|
|
|||
Exercised |
|
|
( |
) |
|
|
|
|
|
|
|
|
||
Forfeited and cancelled |
|
|
— |
|
|
|
— |
|
|
|
|
|
|
|
Outstanding at December 31, 2023 |
|
|
|
|
$ |
|
|
|
$ |
— |
|
|||
Exercisable at December 31, 2023 |
|
|
|
|
$ |
|
|
|
$ |
— |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|||
The weighted-average grant date fair value of stock options granted during the years ended December 31, 2023, 2022 and 2021, was $
87
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
2021 was less than $
The Company has also awarded restricted stock under the 2009 Plan to employees of certain subsidiaries. With respect to time-based vesting restricted stock that has been awarded under the 2009 Plan, the restrictions on these shares have generally lapsed in
Restricted stock outstanding under the 2009 Plan as of December 31, 2023, and changes during each of the years in the three-year period prior to December 31, 2023, were as follows:
|
|
Shares |
|
|
Weighted- |
|
||
Unvested at December 31, 2020 |
|
|
|
|
$ |
|
||
Granted |
|
|
|
|
|
|
||
Vested |
|
|
( |
) |
|
|
|
|
Forfeited |
|
|
( |
) |
|
|
|
|
Unvested at December 31, 2021 |
|
|
|
|
|
|
||
Granted |
|
|
|
|
|
|
||
Vested |
|
|
( |
) |
|
|
|
|
Forfeited |
|
|
( |
) |
|
|
|
|
Unvested at December 31, 2022 |
|
|
|
|
|
|
||
Granted |
|
|
|
|
|
|
||
Vested |
|
|
( |
) |
|
|
|
|
Forfeited |
|
|
( |
) |
|
|
|
|
Unvested at December 31, 2023 |
|
|
|
|
|
|
||
RSUs have been granted to the Company’s non-management directors under the 2009 Plan. Each of the Company’s then serving non-management directors received grants under the 2009 Plan of
88
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
RSUs outstanding under the 2009 Plan as of December 31, 2023, and changes during each of the years in the three-year period prior to December 31, 2023, were as follows:
|
|
Shares |
|
|
Weighted- |
|
||
Unvested at December 31, 2020 |
|
|
|
|
$ |
|
||
Granted |
|
|
|
|
|
|
||
Vested |
|
|
( |
) |
|
|
|
|
Forfeited |
|
|
— |
|
|
|
— |
|
Unvested at December 31, 2021 |
|
|
|
|
|
|
||
Granted |
|
|
|
|
|
|
||
Vested |
|
|
( |
) |
|
|
|
|
Forfeited |
|
|
— |
|
|
|
— |
|
Unvested at December 31, 2022 |
|
|
|
|
|
|
||
Granted |
|
|
|
|
|
|
||
Vested |
|
|
( |
) |
|
|
|
|
Forfeited |
|
|
— |
|
|
|
— |
|
Unvested at December 31, 2023 |
|
|
|
|
|
|
||
3. ACQUISITIONS, DIVESTITURES AND CLOSURES
Acquisitions
The Company accounts for all transactions that represent business combinations using the acquisition method of accounting, where the identifiable assets acquired, the liabilities assumed and any noncontrolling interest in the acquired entity are recognized and measured at their fair values on the date the Company obtains control in the acquiree. Such fair values that are not finalized for reporting periods following the acquisition date are estimated and recorded as provisional amounts. Adjustments to these provisional amounts during the measurement period (defined as the date through which all information required to identify and measure the consideration transferred, the assets acquired, the liabilities assumed and any noncontrolling interests has been obtained, limited to one year from the acquisition date) are recorded when identified. Goodwill is determined as the excess of the fair value of the consideration conveyed in the acquisition over the fair value of the net assets acquired.
The Company accounts for asset acquisitions pursuant to a cost accumulation model. Direct transaction costs are recognized as part of the cost of an acquisition. The Company also evaluates which elements of a transaction should be accounted for as part of an asset acquisition and which should be accounted for separately. The cost of an asset acquisition, including transaction costs, is allocated to identifiable assets acquired and liabilities assumed based on a relative fair value basis. Goodwill is not recognized in an asset acquisition.
During the years ended December 31, 2023, 2022 and 2021, one or more subsidiaries of the Company paid approximately $
89
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Divestitures
Hospital |
|
Buyer |
|
City, State |
|
Licensed |
|
Effective Date |
2023 Divestitures: |
|
|
|
|
|
|
|
|
Greenbrier Valley Medical Center |
|
Vandalia Health, Inc. |
|
Ronceverte, WV |
|
|
||
Plateau Medical Center |
|
Vandalia Health, Inc. |
|
Oak Hill, WV |
|
|
||
Medical Center of South Arkansas |
|
SARH Holdings, Inc. |
|
El Dorado, AR |
|
|
||
Lutheran Rehabilitation Hospital |
|
Select Medical Corporation |
|
Fort Wayne, IN |
|
|
||
AllianceHealth Ponca City |
|
Integris Health |
|
Ponca City, OK |
|
|
||
AllianceHealth Woodward |
|
Integris Health |
|
Woodward, OK |
|
|
||
Bravera Health Brooksville |
|
Tampa General Hospital |
|
Brooksville, FL |
|
|
||
Bravera Health Spring Hill |
|
Tampa General Hospital |
|
Spring Hill, FL |
|
|
||
Bravera Health Seven Rivers |
|
Tampa General Hospital |
|
Crystal River, FL |
|
|
||
|
|
|
|
|
|
|
|
|
2022 Divestitures: |
|
|
|
|
|
|
|
|
AllianceHealth Seminole |
|
SSM Health Care of Oklahoma, Inc. |
|
Seminole, OK |
|
|
||
|
|
|
|
|
|
|
|
|
2021 Divestitures: |
|
|
|
|
|
|
|
|
Lea Regional Medical Center |
|
Covenant Health System |
|
Hobbs, NM |
|
|
||
Tennova Healthcare - Tullahoma |
|
Vanderbilt University Medical Center |
|
Tullahoma, TN |
|
|
||
Tennova Healthcare - Shelbyville |
|
Vanderbilt University Medical Center |
|
Shelbyville, TN |
|
|
||
Northwest Mississippi Medical Center |
|
Delta Health System |
|
Clarksdale, MS |
|
|
||
AllianceHealth Midwest |
|
SSM Health Care of Oklahoma, Inc. |
|
Midwest City, OK |
|
|
||
|
|
|
|
|
|
|
|
|
On February 28, 2023, the Company entered into a definitive agreement for the sale of substantially all of the assets of Lake Norman Regional Medical Center (
The following table discloses amounts included in the consolidated balance sheet for hospitals and other assets classified as held-for-sale as of December 31, 2023 and 2022 (in millions). Other assets, net primarily includes goodwill and the net property and equipment for hospitals held-for-sale. No hospitals were classified as held-for-sale as of December 31, 2021 and no divestitures or potential divestitures meet the criteria for reporting as a discontinued operation as of December 31, 2023, 2022, or 2021.
|
December 31, |
|
|||||
|
2023 |
|
|
2022 |
|
||
Other current assets |
$ |
|
|
$ |
|
||
Other assets, net |
|
|
|
|
|
||
Accrued liabilities |
|
( |
) |
|
|
( |
) |
Closures
During the three months ended September 30, 2022, the Company completed the closure of Shorepoint Health Venice hospital (
During the three months ended September 30, 2022, the provision of inpatient services and substantially all outpatient services ceased at First Hospital Wyoming Valley (psychiatric hospital) (
90
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Other
On December 31, 2022, the lease for AllianceHealth Clinton (
4. GOODWILL AND OTHER INTANGIBLE ASSETS
Goodwill
The changes in the carrying amount of goodwill for the years ended 2023 and 2022 are as follows (in millions):
Balance, beginning balance |
|
2023 |
|
|
2022 |
|
||
Goodwill |
|
$ |
|
|
$ |
|
||
Accumulated impairment losses |
|
|
( |
) |
|
|
( |
) |
|
|
|
|
|
|
|
||
Goodwill acquired as part of acquisitions during current year |
|
|
|
|
|
|
||
Goodwill allocated to hospitals divested or held-for-sale |
|
|
( |
) |
|
|
( |
) |
|
|
|
|
|
|
|
||
Balance, end of year |
|
|
|
|
|
|
||
Goodwill |
|
|
|
|
|
|
||
Accumulated impairment losses |
|
|
( |
) |
|
|
( |
) |
|
|
$ |
|
|
$ |
|
||
Goodwill is allocated to each identified reporting unit, which is defined as an operating segment or one level below the operating segment (referred to as a component of the entity). Management has determined that the Company’s operating segment meets the criteria to be classified as a reporting unit. At December 31, 2023, after giving effect to the 2023 acquisition and divestiture activity, the Company had approximately $
Goodwill is evaluated for impairment annually and when an event occurs or circumstances change that, more likely than not, reduce the fair value of the reporting unit below its carrying value. The Company performed its last annual goodwill impairment evaluation during the fourth quarter of 2023 using an October 31, 2023 measurement date, which indicated
The Company estimates the fair value of the reporting unit using both a discounted cash flow model as well as a market multiple model. The cash flow forecasts are adjusted by an appropriate discount rate based on the Company’s estimate of a market participant’s weighted-average cost of capital. These models are both based on the Company’s best estimate of future revenues and operating costs and are reconciled to the Company’s consolidated market capitalization, with consideration of the amount a potential acquirer would be required to pay, in the form of a control premium, in order to gain sufficient ownership to set policies, direct operations and control management decisions.
The determination of fair value in the Company’s goodwill impairment analysis is based on an estimate of fair value for the reporting unit utilizing known and estimated inputs at the evaluation date. Some of those inputs include, but are not limited to, the most recent price of the Company’s common stock and fair value of long-term debt, the Company’s recent financial results, estimates of future revenue and expense growth, estimated market multiples, expected capital expenditures, income tax rates, costs of invested capital and a discount rate.
Future estimates of fair value could be adversely affected if the actual outcome of one or more of the assumptions described above changes materially in the future, including as a result of any decline in the Company’s stock price and the fair value of its long-term debt, an increase in the volatility of the Company’s stock price and the fair value of its long-term debt, lower-than-expected hospital volumes and/or net operating revenues, higher market interest rates, increased operating costs or other adverse impacts on the Company’s financial results. Such changes impacting the calculation of fair value could result in a material impairment charge in the future.
The determination of fair value of the Company’s hospital operations reporting unit as part of its goodwill impairment measurement represents a Level 3 fair value measurement in the fair value hierarchy due to its use of internal projections and unobservable measurement inputs.
91
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Intangible Assets
During the year ended December 31, 2023, the Company acquired goodwill and a definite-lived intangible asset for the acquisition of an assembled workforce.
The weighted-average remaining amortization period for the intangible assets subject to amortization is approximately three years. There are no expected residual values related to these intangible assets. Amortization expense on these intangible assets was $
The gross carrying amount of capitalized software for internal use was approximately $
5. INCOME TAXES
The provision for income taxes consists of the following (in millions):
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Current: |
|
|
|
|
|
|
|
|
|
|||
Federal |
|
$ |
|
|
$ |
— |
|
|
$ |
( |
) |
|
State |
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
( |
) |
||
Deferred: |
|
|
|
|
|
|
|
|
|
|||
Federal |
|
|
( |
) |
|
|
|
|
|
|
||
State |
|
|
|
|
|
( |
) |
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|||
Total provision for income taxes for income |
|
$ |
|
|
$ |
|
|
$ |
|
|||
92
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
The following table reconciles the differences between the statutory federal income tax rate and the effective tax rate (dollars in millions):
|
|
Year Ended December 31, |
|
|||||||||||||||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||||||||||||||
|
|
Amount |
|
|
% |
|
|
Amount |
|
|
% |
|
|
Amount |
|
|
% |
|
||||||
Provision for income taxes at statutory |
|
$ |
|
|
|
% |
|
$ |
|
|
|
% |
|
$ |
|
|
|
% |
||||||
State income taxes, net of federal income tax benefit |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
Net income attributable to noncontrolling interests |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Change in valuation allowance |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
Change in uncertain tax position |
|
|
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
||
Nondeductible goodwill |
|
|
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
||
Amended return adjustments |
|
|
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
( |
) |
|
|
( |
) |
||
Other |
|
|
|
|
|
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
||
Provision for income taxes and |
|
$ |
|
|
|
% |
|
$ |
|
|
|
% |
|
$ |
|
|
|
% |
||||||
The Company’s effective tax rates were
Deferred income taxes are based on the estimated future tax effects of differences between the financial statement and tax bases of assets and liabilities under the provisions of the enacted tax laws. Deferred income taxes as of December 31, 2023 and 2022 consist of (in millions):
|
|
December 31, |
|
|||||||||||||
|
|
2023 |
|
|
2022 |
|
||||||||||
|
|
Assets |
|
|
Liabilities |
|
|
Assets |
|
|
Liabilities |
|
||||
Net operating loss and credit carryforwards |
|
$ |
|
|
$ |
— |
|
|
$ |
|
|
$ |
— |
|
||
Property and equipment |
|
|
— |
|
|
|
|
|
|
— |
|
|
|
|
||
Self-insurance liabilities |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Prepaid expenses |
|
|
— |
|
|
|
|
|
|
— |
|
|
|
|
||
Intangibles |
|
|
— |
|
|
|
|
|
|
— |
|
|
|
|
||
Investments in unconsolidated affiliates |
|
|
— |
|
|
|
|
|
|
— |
|
|
|
|
||
Other liabilities |
|
|
— |
|
|
|
|
|
|
— |
|
|
|
|
||
Long-term debt and interest |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Accounts receivable |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
IRC Section 163(j) interest limitation |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Accrued vacation |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Accrued bonus |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Other comprehensive income |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Right-of-use assets |
|
|
— |
|
|
|
|
|
|
— |
|
|
|
|
||
Right-of-use liability |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Stock-based compensation |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Deferred compensation |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
IRC Section 481(a) adjustments |
|
|
— |
|
|
|
|
|
|
— |
|
|
|
|
||
Other |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Total |
|
|
|
|
|
|
|
|
|
|
|
|
||||
Valuation allowance |
|
|
( |
) |
|
|
— |
|
|
|
( |
) |
|
|
— |
|
Total deferred income taxes |
|
$ |
|
|
$ |
|
|
$ |
|
|
$ |
|
||||
93
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
The Company believes that the net deferred tax assets will ultimately be realized, except as noted below. Its conclusion is based on its estimate of future taxable income and the expected timing of temporary difference reversals. The Company has gross state net operating loss carryforwards of approximately $
The valuation allowance for federal and state jurisdictions where the Company concluded that the associated deferred tax assets would not be realized increased by $
The total amount of unrecognized benefit that would affect the effective tax rate, if recognized, was $
It is possible the amount of unrecognized tax benefit could change in the next 12 months as a result of a lapse of the statute of limitations and settlements with taxing authorities; however, the Company does not anticipate the change will have a material impact on the Company’s consolidated results of operations or consolidated financial position.
The following is a tabular reconciliation of the total amount of unrecognized tax benefit for the years ended December 31, 2023, 2022 and 2021 (in millions):
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Unrecognized tax benefit, beginning of year |
|
$ |
|
|
$ |
|
|
$ |
|
|||
Gross increases — tax positions in current period |
|
|
|
|
|
|
|
|
|
|||
Reductions — tax positions in prior period |
|
|
( |
) |
|
|
— |
|
|
|
( |
) |
Unrecognized tax benefit, end of year |
|
$ |
|
|
$ |
|
|
$ |
|
|||
The Company’s income tax return for the tax year remains under examination by the Internal Revenue Service. The Company believes the result of this examination will not be material to its consolidated results of operations or consolidated financial position. The Company has extended the federal statute of limitations through June 30, 2025 for Community Health Systems, Inc. for the tax period ended December 31, 2018.
Cash paid for income taxes, net of refunds received, was $
94
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
6. LONG-TERM DEBT
Long-term debt, net of unamortized debt issuance costs and discounts or premiums, consists of the following (in millions):
|
|
December 31, |
|
|||||
|
|
2023 |
|
|
2022 |
|
||
|
$ |
|
|
$ |
|
|||
|
|
|
|
|
|
|||
Senior Secured Notes due |
|
|
|
|
|
|
||
% Senior Notes due |
|
|
|
|
|
|
||
|
|
|
|
|
|
|||
¼% Senior Secured Notes due |
|
|
|
|
|
|
||
% Senior Secured Notes due |
|
|
|
|
|
|
||
% Senior Secured Notes due |
|
|
|
|
|
— |
|
|
% Junior-Priority Secured Notes due |
|
|
|
|
|
|
||
⅛% Junior-Priority Secured Notes due |
|
|
|
|
|
|
||
ABL Facility |
|
|
|
|
|
|
||
Finance lease and financing obligations |
|
|
|
|
|
|
||
Other |
|
|
|
|
|
|
||
Less: Unamortized deferred debt issuance costs and note discount |
|
|
( |
) |
|
|
( |
) |
Total debt |
|
|
|
|
|
|
||
Less: Current maturities |
|
|
( |
) |
|
|
( |
) |
Total long-term debt |
|
$ |
|
|
$ |
|
||
8% Senior Secured Notes due 2026
On
The 8% Senior Secured Notes due 2026 and the related guarantees are secured by shared (i) first-priority liens on the Non-ABL Priority Collateral and (ii) second-priority liens on the ABL Priority Collateral that secures on a first-priority basis the ABL Facility, in each case subject to permitted liens described in the indenture governing the 8% Senior Secured Notes due 2026.
After March 15, 2022, CHS is entitled, at its option, to redeem all or a portion of the 8% Senior Secured Notes due 2026 upon not less than 15 nor more than 60 days’ notice, at the following redemption prices (expressed as a percentage of principal amount on the redemption date), plus accrued and unpaid interest, if any, to the redemption date (subject to the right of holders of record on the relevant record date to receive interest due on the relevant interest payment date), if redeemed during the periods set forth below:
Period |
|
Redemption Price |
|
|
|
|
% |
||
|
|
% |
||
95
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
8% Senior Secured Notes due 2027
On November 19, 2019, CHS issued approximately $
The 8% Senior Secured Notes due 2027 and the related guarantees are secured by shared (i) first-priority liens on the Non-ABL Priority Collateral and (ii) second-priority liens on the ABL Priority Collateral that secures on a first-priority basis the ABL Facility, in each case subject to permitted liens described in the indenture governing the 8% Senior Secured Notes due 2027.
CHS may redeem some or all of the 8% Senior Secured Notes due 2027 at any time on or after December 15, 2022 upon not less than
Period |
|
Redemption Price |
|
|
|
|
% |
||
|
|
% |
||
5⅝% Senior Secured Notes due 2027
On
The 5⅝% Senior Secured Notes due 2027 and the related guarantees are secured by shared (i) first-priority liens on the Non-ABL Priority Collateral and (ii) second-priority liens on the ABL Priority Collateral that secures on a first-priority basis the ABL Facility, in each case subject to permitted liens described in the indenture governing the 5⅝% Senior Secured Notes due 2027.
At any time and from time to time on or after December 15, 2023, CHS may redeem the 5⅝% Senior Secured Notes due 2027 in whole or in part, upon not less than
Period |
|
Redemption Price |
|
|
|
|
% |
||
|
|
% |
||
|
|
% |
||
96
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
6⅞% Senior Notes due 2028
On November 19, 2019, CHS issued approximately $
CHS may redeem some or all of the 6⅞% Senior Notes due 2028 at any time on or after April 1, 2023 upon not less than
Period |
|
Redemption Price |
|
|
|
|
% |
||
|
|
% |
||
|
|
% |
||
On December 7, 2020, CHS entered into a privately negotiated agreement with a multi-asset investment manager who has certain funds and accounts which are holders of the 6⅞% Senior Notes due 2028. Pursuant to the agreement, the Company exchanged $
During the year ended December 31, 2020, the Company extinguished $
6% Senior Secured Notes due 2029
On December 28, 2020, CHS completed a private offering of $
The 6% Senior Secured Notes due 2029 and the related guarantees are secured by shared (i) first-priority liens on the Non-ABL Priority Collateral and (ii) second-priority liens on the ABL Priority Collateral that secures on a first-priority basis the ABL Facility, in each case subject to permitted liens described in the indenture governing the 6% Senior Secured Notes due 2029.
CHS is entitled, at its option, to redeem all or a portion of the 6% Senior Secured Notes due 2029 at any time prior to January 15, 2024, upon not less than
97
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
CHS may redeem up to
At any time and from time to time on or after January 15, 2024, CHS may redeem the 6% Senior Secured Notes due 2029 in whole or in part, upon not less than
Period |
|
Redemption Price |
|
|
|
|
% |
||
|
|
% |
||
|
|
% |
||
5¼% Senior Secured Notes due 2030
On
The 5¼% Senior Secured Notes due 2030 and the related guarantees are secured by shared (i) first-priority liens on the Non-ABL Priority Collateral and (ii) second-priority liens on the ABL Priority Collateral that secures on a first-priority basis the ABL Facility, in each case subject to permitted liens described in the indenture governing the 5¼% Senior Secured Notes due 2030.
CHS is entitled, at its option, to redeem all or a portion of the 5¼% Senior Secured Notes due 2030 at any time prior to May 15, 2025, upon not less than
CHS may redeem up to
At any time and from time to time on or after
Period |
|
Redemption Price |
|
|
|
|
% |
||
|
|
% |
||
|
|
% |
||
98
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
4¾% Senior Secured Notes due 2031
On
The 4¾% Senior Secured Notes due 2031 and the related guarantees are secured by shared (i) first-priority liens on the Non-ABL Priority Collateral and (ii) second-priority liens on the ABL Priority Collateral that secures on a first-priority basis the ABL Facility, in each case subject to permitted liens described in the indenture governing the 4¾% Senior Secured Notes due 2031.
CHS is entitled, at its option, to redeem all or a portion of the ¾% Senior Secured Notes due
CHS may redeem up to
At any time and from time to time on or after
Period |
|
Redemption |
|
|
|
|
% |
||
|
|
% |
||
|
|
% |
||
|
|
% |
||
10⅞% Senior Secured Notes due 2032
On December 22, 2023, CHS completed a private offering of $
The 10⅞% Senior Secured Notes due 2032 and the related guarantees are secured by shared (i) first-priority liens on the Non-ABL Priority Collateral and (ii) second-priority liens on the ABL Priority Collateral that secures on a first-priority basis the ABL Facility, in each case subject to permitted liens described in the indenture governing the 10⅞% Senior Secured Notes due 2032.
99
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
CHS is entitled, at its option, to redeem all or a portion of the ⅞% Senior Secured Notes due
CHS may redeem up to
At any time and from time to time on or after
Period |
|
Redemption |
|
|
|
|
% |
||
|
|
% |
||
|
|
% |
||
6⅞% Junior-Priority Secured Notes due 2029
On
The ⅞% Junior-Priority Secured Notes due
At any time and from time to time prior to
CHS may redeem up to
100
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
At any time and from time to time on or after
Period |
|
Redemption |
|
|
|
|
% |
||
|
|
% |
||
|
|
% |
||
6⅛% Junior-Priority Secured Notes due 2030
On
The 6⅛% Junior-Priority Secured Notes due 2030 and the related guarantees are secured by shared (i) second-priority liens on the Non-ABL Priority Collateral and (ii) third-priority liens on the ABL Priority Collateral that secures on a first-priority basis the ABL Facility, in each case subject to permitted liens described in the indenture governing the 6⅛% Junior-Priority Secured Notes due 2030.
CHS is entitled, at its option, to redeem all or a portion of the 6⅛% Junior-Priority Secured Notes due 2030 at any time prior to
CHS may redeem up to
At any time and from time to time on or after
Period |
|
Redemption Price |
|
|
|
|
% |
||
|
|
% |
||
|
|
% |
||
101
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
During the years ended December 31, 2023 and 2022, the Company extinguished a portion of certain series of its outstanding notes through open market repurchases, and privately negotiated repurchases with a limited number of holders, as follows (in millions):
|
December 31, |
|
|||||
|
2023 |
|
|
2022 |
|
||
⅞% Senior Notes due |
$ |
— |
|
|
$ |
|
|
|
|
|
|
— |
|
||
% Senior Secured Notes due |
|
— |
|
|
|
|
|
% Junior-Priority Secured Notes due |
|
|
|
|
|
||
% Junior-Priority Secured Notes due |
|
|
|
|
|
||
Total principal amount of debt extinguished |
$ |
|
|
$ |
|
||
Financing and repayment transactions discussed above, including open market and privately negotiated repurchases, resulted in a pre-tax and after-tax gain from early extinguishment of debt of $
ABL Facility
On November 22, 2021, the Company and CHS entered into an amendment and restatement agreement (the “Amendment”) to refinance and replace the asset-based loan (ABL) credit agreement (the “ABL Credit Agreement” and, as amended by the Amendment, the “Amended and Restated ABL Credit Agreement”), dated as of April 3, 2018, with JPMorgan Chase Bank, N.A., as administrative agent, and the lenders and other agents party thereto. Pursuant to the Amended and Restated ABL Credit Agreement, the lenders have extended to CHS a revolving asset-based loan facility in the maximum aggregate principal amount of $
Borrowings under the ABL Facility bear interest at a rate per annum equal to an applicable percentage, plus, at the borrower’s option, either (a) a base rate or (b) the Federal Reserve’s secured overnight financing rate (“SOFR”). The applicable margin under the ABL Facility is determined based on excess availability as a percentage of the maximum commitment amount under the ABL Facility at a rate per annum of
Principal amounts outstanding under the ABL Facility will be due and payable in full on November 22, 2026. The ABL Facility includes a 91-day springing maturity applicable if more than $
The ABL Facility contains customary representations and warranties, subject to limitations and exceptions, and customary covenants restricting the Company’s ability, subject to certain exceptions, to, among other things (1) declare dividends, make distributions or redeem or repurchase capital stock, (2) prepay, redeem or repurchase other debt, (3) incur liens or grant negative pledges, (4) make loans and investments and enter into acquisitions and joint ventures, (5) incur additional indebtedness or provide certain guarantees, (6) engage in mergers, acquisitions and asset sales, (7) conduct transactions with affiliates, (8) alter the nature of the Company’s, CHS’ or the guarantors’ businesses, (9) grant certain guarantees with respect to physician practices, (10) engage in
102
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
sale and leaseback transactions or (11) change the Company’s fiscal year. The Company is also required to comply with a consolidated fixed coverage ratio, upon certain triggering events described below, and various affirmative covenants. The consolidated fixed coverage ratio is calculated as the ratio of (x) consolidated EBITDA (as defined in the ABL Facility) less capital expenditures to (y) the sum of consolidated interest expense (as defined in the ABL Facility), scheduled principal payments, income taxes and restricted payments made in cash or in permitted investments. For purposes of calculating the consolidated fixed charge coverage ratio, the calculation of consolidated EBITDA as defined in the ABL Facility is a trailing 12-month calculation that begins with the Company’s consolidated net income, with certain adjustments for interest, taxes, depreciation and amortization, net income attributable to noncontrolling interests, stock compensation expense, restructuring costs, and the financial impact of other non-cash or non-recurring items recorded during any such 12-month period. The consolidated fixed charge coverage ratio is a required covenant only in periods where the total borrowings outstanding under the ABL Facility reduce the amount available in the facility to less than the greater of (i) $
In addition, in the event the amount of borrowings and letters of credit outstanding at any time under the ABL Facility exceeds the borrowing base at such time, the Company will be required to, first, repay outstanding borrowings and, second, replace or cash collateralize outstanding letters of credit, in an aggregate amount sufficient to eliminate such excess.
Events of default under the ABL Facility include, but are not limited to, (1) CHS’ failure to pay principal, interest, fees or other amounts under the ABL Facility Agreement when due (taking into account any applicable grace period), (2) any representation or warranty proving to have been materially incorrect when made, (3) covenant defaults subject, with respect to certain covenants, to an available cure and applicable grace periods, (4) bankruptcy and insolvency events, (5) a cross default to certain other debt, (6) certain undischarged judgments (not paid within an applicable grace period), (7) a change of control (as defined), (8) certain ERISA-related defaults and (9) the invalidity or impairment of specified security interests, guarantees or subordination provisions in favor of the ABL agent or lenders under the ABL Facility.
As of December 31, 2023, the scheduled maturities of long-term debt outstanding, including finance lease and financing obligations for each of the next five years and thereafter are as follows (in millions):
Year Ending December 31, |
|
Amount |
|
|
2024 |
|
$ |
|
|
2025 |
|
|
|
|
2026 |
|
|
|
|
2027 |
|
|
|
|
2028 |
|
|
|
|
Thereafter |
|
|
|
|
Total maturities |
|
|
|
|
Less: Deferred debt issuance costs |
|
|
( |
) |
Less: Unamortized note discount |
|
|
( |
) |
Total long-term debt |
|
$ |
|
|
The Company paid interest of $
103
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
7. FAIR VALUE OF FINANCIAL INSTRUMENTS
The fair value of financial instruments has been estimated by the Company using available market information as of December 31, 2023 and 2022, and valuation methodologies considered appropriate. The estimates presented in the table below are not necessarily indicative of amounts the Company could realize in a current market exchange (in millions):
|
|
December 31, 2023 |
|
|
December 31, 2022 |
|
||||||||||
|
|
Carrying |
|
|
Estimated |
|
|
Carrying |
|
|
Estimated |
|
||||
|
|
Amount |
|
|
Value |
|
|
Amount |
|
|
Value |
|
||||
Assets: |
|
|
|
|
|
|
|
|
|
|
|
|
||||
Cash and cash equivalents |
|
$ |
|
|
$ |
|
|
$ |
|
|
$ |
|
||||
Investments in equity securities |
|
|
|
|
|
|
|
|
|
|
|
|
||||
Available-for-sale debt securities |
|
|
|
|
|
|
|
|
|
|
|
|
||||
Trading securities |
|
|
|
|
|
|
|
|
|
|
|
|
||||
Liabilities: |
|
|
|
|
|
|
|
|
|
|
|
|
||||
8% Senior Secured Notes due 2026 |
|
|
|
|
|
|
|
|
|
|
|
|
||||
8% Senior Secured Notes due 2027 |
|
|
|
|
|
|
|
|
|
|
|
|
||||
5⅝% Senior Secured Notes due 2027 |
|
|
|
|
|
|
|
|
|
|
|
|
||||
6⅞% Senior Notes due 2028 |
|
|
|
|
|
|
|
|
|
|
|
|
||||
6% Senior Secured Notes due 2029 |
|
|
|
|
|
|
|
|
|
|
|
|
||||
5¼% Senior Secured Notes due 2030 |
|
|
|
|
|
|
|
|
|
|
|
|
||||
4¾% Senior Secured Notes due 2031 |
|
|
|
|
|
|
|
|
|
|
|
|
||||
10⅞% Senior Secured Notes due 2032 |
|
|
|
|
|
|
|
|
— |
|
|
|
— |
|
||
6⅞% Junior-Priority Secured Notes due 2029 |
|
|
|
|
|
|
|
|
|
|
|
|
||||
6⅛% Junior-Priority Secured Notes due 2030 |
|
|
|
|
|
|
|
|
|
|
|
|
||||
ABL Facility and other debt |
|
|
|
|
|
|
|
|
|
|
|
|
||||
The carrying value of the Company’s long-term debt in the above table is presented net of unamortized deferred debt issuance costs. The estimated fair value is determined using the methodologies discussed below in accordance with accounting standards related to the determination of fair value based on the U.S. GAAP fair value hierarchy as discussed in Note 8. The estimated fair value for financial instruments with a fair value that does not equal its carrying value is considered a Level 1 valuation. The Company utilizes the market approach and obtains indicative pricing through publicly available subscription services such as Bloomberg to determine fair values where relevant.
Cash and cash equivalents. The carrying amount approximates fair value due to the short-term maturity of these instruments (less than three months).
Investments in equity securities. Estimated fair value is based on closing price as quoted in public markets.
Available-for-sale debt securities. Estimated fair value is based on closing price as quoted in public markets or other various valuation techniques.
Trading securities. Estimated fair value is based on closing price as quoted in public markets.
Senior Notes, Senior Secured Notes and Junior-Priority Secured Notes. Estimated fair value is based on the closing market price for these notes.
ABL Facility and other debt. The carrying amount of the ABL Facility and all other debt approximates fair value due to the nature of these obligations.
104
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
8. FAIR VALUE
Fair Value Hierarchy
Fair value is a market-based measurement, not an entity-specific measurement. Therefore, a fair value measurement should be determined based on the assumptions that market participants would use in pricing the asset or liability. As a basis for considering market participant assumptions in fair value measurements, the Company utilizes the U.S. GAAP fair value hierarchy that distinguishes between market participant assumptions based on market data obtained from sources independent of the reporting entity (observable inputs that are classified within Levels 1 and 2 of the hierarchy) and the reporting entity’s own assumption about market participant assumptions (unobservable inputs classified within Level 3 of the hierarchy).
The inputs used to measure fair value are classified into the following fair value hierarchy:
Level 1: |
|
Quoted market prices in active markets for identical assets or liabilities. |
Level 2: |
|
Observable market-based inputs or unobservable inputs that are corroborated by market data. |
Level 3: |
|
Unobservable inputs that are supported by little or no market activity and are significant to the fair value of the assets or liabilities. Level 3 includes values determined using pricing models, discounted cash flow methodologies, or similar techniques reflecting the Company’s own assumptions. |
In instances where the determination of the fair value hierarchy measurement is based on inputs from different levels of the fair value hierarchy, the level in the fair value hierarchy within which the entire fair value measurement falls is based on the lowest level input that is significant to the fair value measurement in its entirety. The Company’s assessment of the significance of a particular input to the fair value measurement in its entirety requires judgment of factors specific to the asset or liability. Transfers between levels within the fair value hierarchy are recognized by the Company on the date of the change in circumstances that requires such transfer. There were
The following table sets forth, by level within the fair value hierarchy, the financial assets recorded at fair value on a recurring basis as of December 31, 2023 and 2022 (in millions):
|
|
December 31, 2023 |
|
|
Level 1 |
|
|
Level 2 |
|
|
Level 3 |
|
||||
Investments in equity securities |
|
$ |
|
|
$ |
|
|
$ |
— |
|
|
$ |
— |
|
||
Available-for-sale debt securities |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Trading securities |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Total assets |
|
$ |
|
|
$ |
|
|
$ |
|
|
$ |
— |
|
|||
|
|
December 31, 2022 |
|
|
Level 1 |
|
|
Level 2 |
|
|
Level 3 |
|
||||
Investments in equity securities |
|
$ |
|
|
$ |
|
|
$ |
— |
|
|
$ |
— |
|
||
Available-for-sale debt securities |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Trading securities |
|
|
|
|
|
— |
|
|
|
|
|
|
— |
|
||
Total assets |
|
$ |
|
|
$ |
|
|
$ |
|
|
$ |
— |
|
|||
Investments in Equity Securities, Available-for-Sale Debt Securities and Trading Securities
Investments in equity securities classified as Level 1 are measured using quoted market prices. Level 2 available-for-sale debt securities and trading securities primarily consist of bonds and notes issued by the United States government and its agencies and domestic and foreign corporations. The estimated fair values of these securities are determined using various valuation techniques, including a multi-dimensional relational model that incorporates standard observable inputs and assumptions such as benchmark yields, reported trades, broker/dealer quotes, issuer spreads, benchmark securities, bids/offers and other pertinent reference data.
105
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Supplemental information regarding the Company’s available-for-sale debt securities (all of which had no withdrawal restrictions) is set forth in the table below (in millions):
|
|
|
|
|
Gross |
|
|
Gross |
|
|
Estimated |
|
||||
|
|
Amortized |
|
|
Unrealized |
|
|
Unrealized |
|
|
Fair |
|
||||
|
|
Cost |
|
|
Gains |
|
|
Losses |
|
|
Values |
|
||||
As of December 31, 2023: |
|
|
|
|
|
|
|
|
|
|
|
|
||||
Government |
|
$ |
|
|
$ |
— |
|
|
$ |
( |
) |
|
$ |
|
||
Corporate |
|
|
|
|
|
— |
|
|
|
( |
) |
|
|
|
||
Mortgage and asset-backed securities |
|
|
|
|
|
— |
|
|
|
( |
) |
|
|
|
||
Total available-for-sale debt securities |
|
$ |
|
|
$ |
— |
|
|
$ |
( |
) |
|
$ |
|
||
|
|
|
|
|
Gross |
|
|
Gross |
|
|
Estimated |
|
||||
|
|
Amortized |
|
|
Unrealized |
|
|
Unrealized |
|
|
Fair |
|
||||
|
|
Cost |
|
|
Gains |
|
|
Losses |
|
|
Values |
|
||||
As of December 31, 2022: |
|
|
|
|
|
|
|
|
|
|
|
|
||||
Government |
|
$ |
|
|
$ |
— |
|
|
$ |
( |
) |
|
$ |
|
||
Corporate |
|
|
|
|
|
— |
|
|
|
( |
) |
|
|
|
||
Mortgage and asset-backed securities |
|
|
|
|
|
— |
|
|
|
( |
) |
|
|
|
||
Total available-for-sale debt securities |
|
$ |
|
|
$ |
— |
|
|
$ |
( |
) |
|
$ |
|
||
As of December 31, 2023 and 2022, investments with aggregate estimated fair values of approximately $
The contractual maturities of debt-based securities held by the Company as of December 31, 2023 and 2022, excluding mutual fund holdings, are set forth in the table below (in millions). Expected maturities will differ from contractual maturities because the issuers of the debt securities may have the right to prepay their obligations without prepayment penalties.
|
|
December 31, 2023 |
|
|
December 31, 2022 |
|
||||||||||
|
|
Amortized |
|
|
Estimated |
|
|
Amortized |
|
|
Estimated |
|
||||
|
|
Cost |
|
|
Fair Values |
|
|
Cost |
|
|
Fair Values |
|
||||
Within 1 year |
|
$ |
|
|
$ |
|
|
$ |
|
|
$ |
|
||||
After 1 year and through year 5 |
|
|
|
|
|
|
|
|
|
|
|
|
||||
After 5 years and through year 10 |
|
|
|
|
|
|
|
|
|
|
|
|
||||
After 10 years |
|
|
|
|
|
|
|
|
|
|
|
|
||||
Gross realized gains and losses on sales of available-for-sale debt securities are summarized in the table below (in millions):
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Realized gains |
|
$ |
— |
|
|
$ |
— |
|
|
$ |
|
|
Realized losses |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Other investment income, which includes interest and dividends, related to all investment securities was $
106
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Net losses and gains recognized during the years ended December 31, 2023, 2022 and 2021 for investments in equity securities, which are broken out between investments sold during the year and investments held at the end of the year, are summarized in the table below (in millions):
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Net gains and (losses) recognized during the year on equity securities |
|
$ |
|
|
$ |
( |
) |
|
$ |
|
||
Less: Net (losses) and gains recognized during the year on equity |
|
|
( |
) |
|
|
( |
) |
|
|
|
|
Unrealized gains and (losses) recognized during the year on equity |
|
$ |
|
|
$ |
( |
) |
|
$ |
|
||
9. LEASES
The Company utilizes operating and finance leases for the use of certain hospitals, medical office buildings, and medical equipment. All lease agreements generally require the Company to pay maintenance, repairs, property taxes and insurance costs, which are variable amounts based on actual costs incurred during each applicable period. Such costs are not included in the determination of the ROU asset or lease liability. Variable lease cost also includes escalating rent payments that are not fixed at commencement but are based on an index that is determined in future periods over the lease term based on changes in the Consumer Price Index or other measures of cost inflation. Most leases include one or more options to renew the lease at the end of the initial term, with renewal terms that generally extend the lease at the then market rate of rental payment. Certain leases also include an option to buy the underlying asset at or a short time prior to the termination of the lease. All such options are at the Company’s discretion and are evaluated at the commencement of the lease, with only those that are reasonably certain of exercise included in determining the appropriate lease term.
The components of lease cost and rent expense for the years ended December 31, 2023, 2022 and 2021 are as follows (in millions):
|
|
Year Ended December 31, |
|
|||||||||
Lease Cost |
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Operating lease cost: |
|
|
|
|
|
|
|
|
|
|||
Operating lease cost |
|
$ |
|
|
$ |
|
|
$ |
|
|||
Short-term rent expense |
|
|
|
|
|
|
|
|
|
|||
Variable lease cost |
|
|
|
|
|
|
|
|
|
|||
Sublease income |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Total operating lease cost |
|
$ |
|
|
$ |
|
|
$ |
|
|||
Finance lease cost: |
|
|
|
|
|
|
|
|
|
|||
Amortization of ROU assets |
|
$ |
|
|
$ |
|
|
$ |
|
|||
Interest on finance lease liabilities |
|
|
|
|
|
|
|
|
|
|||
Total finance lease cost |
|
$ |
|
|
$ |
|
|
$ |
|
|||
107
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Supplemental balance sheet information related to leases was as follows (in millions):
|
|
Balance Sheet Classification |
|
December 31, 2023 |
|
|
December 31, 2022 |
|
||
Operating Leases: |
|
|
|
|
|
|
|
|
||
Operating Lease ROU Assets |
|
|
$ |
|
|
$ |
|
|||
|
|
|
|
|
|
|
|
|
||
Finance Leases: |
|
|
|
|
|
|
|
|
||
Finance Lease ROU Assets |
|
Property and equipment |
|
|
|
|
|
|
||
|
|
Land and improvements |
|
$ |
— |
|
|
$ |
— |
|
|
|
Buildings and improvements |
|
|
|
|
|
|
||
|
|
Equipment and fixtures |
|
|
|
|
|
|
||
|
|
Property and equipment |
|
|
|
|
|
|
||
|
|
Less accumulated depreciation and amortization |
|
|
( |
) |
|
|
( |
) |
|
|
Property and equipment, net |
|
$ |
|
|
$ |
|
||
|
|
|
|
|
|
|
|
|
||
Current finance lease liabilities |
|
|
$ |
|
|
$ |
|
|||
Long-term finance lease liabilities |
|
|
|
|
|
|
|
|||
Supplemental cash flow information related to leases for the years ended December 31, 2023, 2022 and 2021 are as follows (in millions):
|
|
Year Ended December 31, |
|
|||||||||
Cash flow information |
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Cash paid for amounts included in the measurement of lease liabilities: |
|
|
|
|
|
|
|
|
|
|||
Operating cash flows from operating leases (1) |
|
$ |
|
|
$ |
|
|
$ |
|
|||
Operating cash flows from finance leases |
|
|
|
|
|
|
|
|
|
|||
Financing cash flows from finance leases |
|
|
|
|
|
|
|
|
|
|||
ROU assets obtained in exchange for new finance lease liabilities |
|
|
|
|
|
|
|
|
|
|||
ROU assets obtained in exchange for new operating lease liabilities |
|
|
|
|
|
|
|
|
|
|||
Weighted-average remaining lease term: |
|
|
|
|
|
|
|
|
|
|||
Operating leases |
|
|
|
|
|
|
||||||
Finance leases |
|
|
|
|
|
|
||||||
Weighted-average discount rate: |
|
|
|
|
|
|
|
|
|
|||
Operating leases |
|
|
% |
|
|
% |
|
|
% |
|||
Finance leases |
|
|
% |
|
|
% |
|
|
% |
|||
Commitments relating to noncancellable operating and finance leases and financing obligations for each of the next five years and thereafter are as follows (in millions):
|
|
|
|
|
|
|
|
Financing |
|
|||
Year Ending December 31, |
|
Operating |
|
|
Finance |
|
|
Obligations |
|
|||
2024 |
|
$ |
|
|
$ |
|
|
$ |
|
|||
2025 |
|
|
|
|
|
|
|
|
|
|||
2026 |
|
|
|
|
|
|
|
|
|
|||
2027 |
|
|
|
|
|
|
|
|
|
|||
2028 |
|
|
|
|
|
|
|
|
|
|||
Thereafter |
|
|
|
|
|
|
|
|
|
|||
Total minimum future payments |
|
|
|
|
|
|
|
|
|
|||
Less: Imputed interest |
|
|
( |
) |
|
|
( |
) |
|
|
|
|
Total liabilities |
|
|
|
|
|
|
|
|
|
|||
Less: Current portion |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Long-term liabilities |
|
$ |
|
|
$ |
|
|
$ |
|
|||
108
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
As of December 31, 2023, there were approximately $
10. EMPLOYEE BENEFIT PLANS
The Company maintains various benefit plans, including defined contribution plans, defined benefit plans and deferred compensation plans, for which certain of the Company’s subsidiaries are the plan sponsors. The CHS/Community Health Systems, Inc. Retirement Savings Plan is a defined contribution plan that covers the majority of the Company’s employees. Employees at locations whose employment is covered by collective bargaining agreements are generally eligible to participate in the CHS/Community Health Systems, Inc. Standard 401(k) Plan. Total expense to the Company under the 401(k) plans was $
The Company maintains unfunded deferred compensation plans that allow participants to defer receipt of a portion of their compensation. The liability for the deferred compensation plans was $
The Company provides an unfunded Supplemental Executive Retirement Plan (“SERP”) for certain members of its executive management. The Company uses a December 31 measurement date for the benefit obligations and a January 1 measurement date for its net periodic costs for the SERP. Variances from actuarially assumed rates will result in increases or decreases in benefit obligations and net periodic cost in future periods. Benefits expense under the SERP was $
During 2021 and 2023, certain members of executive management of the Company that were participants in the SERP retired and met the requirements for payout of their SERP retirement benefit. The SERP payout provisions require payment to the participant in an actuarially determined lump sum amount six months after the participant retires from the Company. There were
As of December 31, 2023, the Company had assets of $
The Company maintains the CHS/Community Health Systems, Inc. Retirement Income Plan (“Pension Plan”), which is a defined benefit, non-contributory pension plan that covers certain employees at three of its formerly owned hospitals. The Pension Plan provides benefits to covered individuals satisfying certain age and service requirements. Employer contributions to the Pension Plan are in accordance with the minimum funding requirements of the Employee Retirement Income Security Act of 1974, as amended. The Company does not expect to make contributions to the Pension Plan in 2024.
In September 2021, the lifetime obligation of the Pension Plan with respect to certain participants was transferred to a third-party insurer via an irrevocable annuity contract. The third-party insurer began paying benefits to the participants as of November 1, 2021. This action resulted in a partial plan settlement and recognition of a less than $
The Company uses a December 31 measurement date for the benefit obligations and a January 1 measurement date for its net periodic costs for the Pension Plan. Variances from actuarially assumed rates will result in increases or decreases in benefit obligations, net periodic cost and funding requirements in future periods. Benefits expense under the Pension Plan was less than $
109
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
11. STOCKHOLDERS’ DEFICIT
Authorized capital shares of the Company include
The Company is a holding company, which operates through its subsidiaries. The ABL Facility and the indentures governing each series of the Company’s outstanding notes contain various covenants under which the assets of the subsidiaries of the Company are subject to certain restrictions relating to, among other matters, dividends and distributions, as referenced in the paragraph below.
The ABL Facility and the indentures governing each series of the Company’s outstanding notes restrict the Company’s subsidiaries from, among other matters, paying dividends and making distributions to the Company, which thereby limits the Company’s ability to pay dividends and/or repurchase stock. As of December 31, 2023, under the most restrictive test in these agreements (and subject to certain exceptions), the Company has approximately $
The following schedule discloses the effects of changes in the Company’s ownership interest in its less-than-wholly-owned subsidiaries on Community Health Systems, Inc. stockholders’ deficit (in millions):
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Net (loss) income attributable to Community Health Systems, |
|
|
|
|
|
|
|
|
|
|||
Inc. stockholders |
|
$ |
( |
) |
|
$ |
|
|
$ |
|
||
Transfers to the noncontrolling interests: |
|
|
|
|
|
|
|
|
|
|||
Net increase (decrease) in Community Health Systems, Inc. |
|
|
|
|
|
( |
) |
|
|
|
||
Net transfers to the noncontrolling interests |
|
|
|
|
|
( |
) |
|
|
|
||
Change to Community Health Systems, Inc. stockholders’ deficit |
|
$ |
( |
) |
|
$ |
|
|
$ |
|
||
12. EARNINGS PER SHARE
The following table sets forth the components of the denominator for the computation of basic and diluted (loss) earnings per share for net (loss) income attributable to Community Health Systems, Inc. stockholders:
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Weighted-average number of shares outstanding — basic |
|
|
|
|
|
|
|
|
|
|||
Effect of dilutive securities: |
|
|
|
|
|
|
|
|
|
|||
Restricted stock awards |
|
|
— |
|
|
|
|
|
|
|
||
Employee stock options |
|
|
— |
|
|
|
|
|
|
|
||
Other equity-based awards |
|
|
— |
|
|
|
|
|
|
|
||
Weighted-average number of shares outstanding — diluted |
|
|
|
|
|
|
|
|
|
|||
The Company generated a net loss attributable to Community Health Systems, Inc. stockholders for the year ended December 31, 2023, so the effect of dilutive securities is not considered because their effect would be antidilutive. If the Company had generated net income, the effect of stock awards and options on the diluted shares calculation would have been an increase of
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Dilutive securities outstanding not included in the computation of earnings |
|
|
|
|
|
|
|
|
|
|||
Employee stock options and restricted stock awards |
|
|
|
|
|
|
|
|
|
|||
110
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
13. EQUITY INVESTMENTS
On
On
In March 2005, the Company began purchasing items, primarily medical supplies, medical equipment and pharmaceuticals, under an agreement with HealthTrust Purchasing Group, L.P. (“HealthTrust”), a group purchasing organization in which the Company is a noncontrolling partner. Effective October 1, 2022, HealthTrust completed the sale of a majority interest in CoreTrust Holdings, LLC (“CoreTrust”) to a third party. Proceeds for the sale of interest in CoreTrust were distributed to members of HealthTrust and the Company received approximately $
The Company’s investment in all of its unconsolidated affiliates was $
14. COMPREHENSIVE LOSS
The following tables present information about items reclassified out of accumulated other comprehensive loss (“AOCL”) by component for the years ended December 31, 2023 and 2022 (in millions, net of tax):
|
|
|
Change in |
|
|
|
|
|
|
|
|||
|
|
|
Fair Value of |
|
|
Change in |
|
|
|
|
|||
|
|
|
Available-for-Sale |
|
|
Unrecognized |
|
|
|
|
|||
|
|
|
Debt |
|
|
Pension Cost |
|
|
|
|
|||
|
|
|
Securities |
|
|
Components |
|
|
AOCL |
|
|||
Balance as of December 31, 2022 |
|
|
$ |
( |
) |
|
$ |
( |
) |
|
$ |
( |
) |
Other comprehensive income |
|
|
|
|
|
|
|
|
|
|
|||
before reclassifications |
|
|
|
|
|
|
|
|
|
|
|||
Amounts reclassified from |
|
|
|
|
|
|
|
|
|
|
|||
AOCL |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
Net current-period other |
|
|
|
|
|
|
|
|
|
|
|||
comprehensive income |
|
|
|
|
|
|
|
|
|
|
|||
Balance as of December 31, 2023 |
|
|
$ |
( |
) |
|
$ |
( |
) |
|
$ |
( |
) |
111
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
|
|
Change in |
|
|
|
|
|
|
|
|||
|
|
Fair Value of |
|
|
Change in |
|
|
|
|
|||
|
|
Available-for-Sale |
|
|
Unrecognized |
|
|
|
|
|||
|
|
Debt |
|
|
Pension Cost |
|
|
|
|
|||
|
|
Securities |
|
|
Components |
|
|
AOCL |
|
|||
Balance as of December 31, 2021 |
|
$ |
( |
) |
|
$ |
( |
) |
|
$ |
( |
) |
Other comprehensive (loss) |
|
|
|
|
|
|
|
|
|
|||
income before reclassifications |
|
|
( |
) |
|
|
|
|
|
( |
) |
|
Amounts reclassified from |
|
|
|
|
|
|
|
|
|
|||
AOCL |
|
|
( |
) |
|
|
— |
|
|
|
( |
) |
Net current-period other |
|
|
|
|
|
|
|
|
|
|||
comprehensive (loss) income |
|
|
( |
) |
|
|
|
|
|
( |
) |
|
Balance as of December 31, 2022 |
|
$ |
( |
) |
|
$ |
( |
) |
|
$ |
( |
) |
There were
15. COMMITMENTS AND CONTINGENCIES
Construction and Other Capital Commitments. Pursuant to a hospital purchase agreement from the Company’s March 1, 2016 acquisition of Northwest Health – Starke, formerly known as Starke Hospital, the Company is committed to spend up to $
Physician Recruiting Commitments. As part of its physician recruitment strategy, the Company provides income guarantee agreements to certain physicians who agree to relocate to its communities and commit to remain in practice there. Under such agreements, the Company is required to make payments to the physicians in excess of the amounts they earned in their practice up to the amount of the income guarantee. These income guarantee periods are typically for
112
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Professional Liability Claims. As part of the Company's business of providing healthcare services, it is subject to legal actions alleging liability on its part. The Company accrues for losses resulting from such liability claims, as well as loss adjustment expenses that are out-of-pocket and directly related to such liability claims. These direct out-of-pocket expenses include fees of outside counsel and experts. The Company does not accrue for costs that are part of corporate overhead, such as the costs of in-house legal and risk management departments. The losses resulting from professional liability claims primarily consist of estimates for known claims, as well as estimates for incurred but not reported claims. The estimates are based on specific claim facts, historical claim reporting and payment patterns, the nature and level of hospital operations, and actuarially determined projections. The actuarially determined projections are based on the Company's actual claim data, including historic reporting and payment patterns, which have been gathered over the life of the Company. As discussed below, since the Company purchases excess insurance on a claims-made basis that transfers risk to third-party insurers, the estimated liability for professional and general liability claims does include an amount for the losses covered by excess insurance. The Company also records a receivable for the expected reimbursement of losses covered by this excess insurance. Since the Company believes that the amount and timing of its future claims payments are reliably determinable, it discounts the amount that is accrued for losses resulting from professional liability claims.
The net present value of the projected payments was discounted using weighted-average interest rates of
The Company’s processes for obtaining and analyzing claims and incident data are standardized across all of its businesses and have been consistent for many years. The Company monitors the outcomes of the medical care services that it provides and for each reported claim, the Company obtains various information concerning the facts and circumstances related to that claim. In addition, the Company routinely monitors current key statistics and volume indicators in its assessment of utilizing historical trends. The average lag period between claim occurrence and payment of a final settlement is between and
For purposes of estimating its individual claim accruals, the Company utilizes specific claim information, including the nature of the claim, the expected claim amount, the year in which the claim occurred and the laws of the jurisdiction in which the claim occurred. Once the case accruals for known claims are determined, information is stratified by loss layers and retentions, accident years, reported years and geography. Several actuarial methods are used against this data to produce estimates of ultimate paid losses and reserves for incurred but not reported claims. Each of these methods uses company-specific historical claims data and other information. This company-specific data includes information regarding the Company’s business, including historical paid losses and loss adjustment expenses, historical and current case loss reserves, actual and projected hospital statistical data, a variety of hospital census information, employed physician information, professional liability retentions for each policy year, geographic information and other data.
Based on these analyses, the Company determines its estimate of the professional liability claims. The determination of management’s estimate, including the preparation of the reserve analysis that supports such estimate, involves subjective judgment of management. Changes in reserve data or the trends and factors that influence reserve data may signal fundamental shifts in the Company’s future claim development patterns or may simply reflect single-period anomalies. Even if a change reflects a fundamental shift, the full extent of the change may not become evident until years later. Moreover, since the Company’s methods and models use different types of data and the Company selects its liability from the results of all of these methods, it typically cannot quantify the precise impact of such factors on its estimates of the liability. Due to the Company’s standardized and consistent processes for handling claims and the long history and depth of company-specific data, the Company’s methodologies have produced reliably determinable estimates of ultimate paid losses. Management considers any changes in the amount and pattern of its historical paid losses up through the most recent reporting period to identify any fundamental shifts or trends in claim development experience in determining the estimate of professional liability claims. However, due to the subjective nature of this estimate and the impact that previously unforeseen shifts in actual claim experience can have, future estimates of professional liability could be adversely impacted when actual paid losses develop unexpectedly based on assumptions and settlement events that were not previously known or anticipated.
113
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
During the year ended December 31, 2020, the Company incurred expenses in the amount of approximately $
The Company is primarily self-insured for professional liability claims; however, the Company obtains excess insurance that transfers the risk of loss to a third-party insurer for claims in excess of the Company’s self-insured retentions. The Company’s excess insurance is underwritten on a claims-made basis. For claims reported prior to June 1, 2002, substantially all of the Company’s professional and general liability risks were subject to a less than $
Excess insurance for all hospitals has been purchased through commercial insurance companies and generally covers the Company for liabilities in excess of the self-insured retentions. The excess coverage consists of multiple layers of insurance, the sum of which totals up to $
Legal Matters. The Company is a party to various legal, regulatory and governmental proceedings incidental to its business. Based on current knowledge, management does not believe that loss contingencies arising from pending legal, regulatory and governmental matters will have a material adverse effect on the consolidated financial position or liquidity of the Company. However, in light of the inherent uncertainties involved in pending legal, regulatory and governmental matters, some of which are beyond the Company’s control, and the very large or indeterminate damages sought in some of these matters, an adverse outcome in one or more of these matters could be material to the Company’s results of operations or cash flows for any particular reporting period.
With respect to all legal, regulatory and governmental proceedings, the Company considers the likelihood of a negative outcome. If the Company determines the likelihood of a negative outcome with respect to any such matter is probable and the amount of the loss can be reasonably estimated, the Company records an accrual for the estimated loss for the expected outcome of the matter. If the likelihood of a negative outcome with respect to material matters is reasonably possible and the Company is able to determine an estimate of the possible loss or a range of loss, whether in excess of a related accrued liability or where there is no accrued liability, the Company discloses the estimate of the possible loss or range of loss. However, the Company is unable to estimate a possible loss or range of loss in some instances based on the significant uncertainties involved in, and/or the preliminary nature of, certain legal, regulatory and governmental matters.
114
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Summary of Recorded Amounts
The table below presents a reconciliation of the beginning and ending liability balances (in millions) during the years ended December 31, 2023 and 2022, with respect to the Company’s determination of the contingencies of the Company in respect of which an accrual has been recorded. The liability as of December 31, 2023 is comprised of individually insignificant amounts for various matters.
|
|
Probable |
|
|
|
|
Contingencies |
|
|
Balance as of December 31, 2021 |
|
$ |
|
|
Expense |
|
|
|
|
Reserve for insured claim |
|
|
— |
|
Cash payments |
|
|
( |
) |
Balance as of December 31, 2022 |
|
|
|
|
Expense |
|
|
|
|
Reserve for insured claim |
|
|
|
|
Cash payments |
|
|
( |
) |
Balance as of December 31, 2023 |
|
$ |
|
|
In accordance with applicable accounting guidance, the Company establishes a liability for litigation, regulatory and governmental matters for which, based on information currently available, the Company believes that a negative outcome is known or is probable and the amount of the loss is reasonably estimable. For all such matters (whether or not discussed in this contingencies footnote), such amounts have been recorded in other accrued liabilities in the consolidated balance sheets and are included in the table above. Due to the uncertainties and difficulty in predicting the ultimate resolution of these contingencies, the actual amount could differ from the estimated amount reflected as a liability in the consolidated balance sheets.
16. CONDENSED FINANCIAL INFORMATION OF PARENT COMPANY
Parent Company Only |
|
|
|
|
|
|
||
Condensed Balance Sheets |
|
|
|
|
|
|
||
(In millions) |
|
|
|
|
|
|
||
|
|
December 31, |
|
|||||
|
|
2023 |
|
|
2022 |
|
||
ASSETS |
|
|
|
|
|
|
||
Prepaid income taxes |
|
$ |
|
|
$ |
|
||
Total current assets |
|
|
|
|
|
|
||
Deferred income taxes |
|
|
|
|
|
|
||
Other assets, net |
|
|
— |
|
|
|
— |
|
Total assets |
|
$ |
|
|
$ |
|
||
LIABILITIES AND STOCKHOLDERS' DEFICIT |
|
|
|
|
|
|
||
Intercompany payable |
|
$ |
|
|
$ |
|
||
Deferred income taxes |
|
|
|
|
|
|
||
Other long-term liabilities |
|
|
|
|
|
|
||
Total liabilities |
|
|
|
|
|
|
||
Community Health Systems, Inc. stockholders’ deficit: |
|
|
|
|
|
|
||
Preferred stock |
|
|
— |
|
|
|
— |
|
Common stock |
|
|
|
|
|
|
||
Additional paid-in capital |
|
|
|
|
|
|
||
Accumulated other comprehensive loss |
|
|
( |
) |
|
|
( |
) |
Accumulated deficit |
|
|
( |
) |
|
|
( |
) |
Total Community Health Systems, Inc. stockholders’ deficit |
|
|
( |
) |
|
|
( |
) |
Total liabilities and stockholders' deficit |
|
$ |
|
|
$ |
|
||
|
|
|
|
|
|
|
||
See note to condensed financial statements of Parent Company. |
|
|
|
|
|
|
||
115
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Parent Company Only |
|
|
|
|
|
|
|
|
|
|||
Condensed Statements of (Loss) Income |
|
|
|
|
|
|
|
|
|
|||
(In millions) |
|
|
|
|
|
|
|
|
|
|||
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Net operating revenues |
|
$ |
— |
|
|
$ |
— |
|
|
$ |
— |
|
Operating costs and expenses: |
|
|
|
|
|
|
|
|
|
|||
Salaries and benefits |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Supplies |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Other operating expenses |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Lease cost and rent |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Pandemic relief funds |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Depreciation and amortization |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Impairment and (gain) loss on sale of businesses, net |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Total operating costs and expenses |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Income from operations |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Interest expense, net |
|
|
— |
|
|
|
— |
|
|
|
— |
|
(Gain) loss from early extinguishment of debt |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Equity in loss (earnings) of unconsolidated affiliates |
|
|
|
|
|
( |
) |
|
|
( |
) |
|
(Loss) income before income taxes |
|
|
( |
) |
|
|
|
|
|
|
||
Provision for (benefit from) income taxes |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Net (loss) income |
|
|
( |
) |
|
|
|
|
|
|
||
Less: Net income attributable to noncontrolling interests |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Net (loss) income attributable to Community Health Systems, Inc. |
|
$ |
( |
) |
|
$ |
|
|
$ |
|
||
|
|
|
|
|
|
|
|
|
|
|||
See note to condensed financial statements of Parent Company. |
|
|
|
|
|
|
|
|
|
|||
116
COMMUNITY HEALTH SYSTEMS, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – (Continued)
Parent Company Only |
|
|
|
|
|
|
|
|
|
|||
Condensed Statements of Comprehensive (Loss) Income |
|
|
|
|
|
|
|
|
|
|||
(In millions) |
|
|
|
|
|
|
|
|
|
|||
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
|
|
|
|
|
(In millions) |
|
|
|
|
|||
Net (loss) income |
|
$ |
( |
) |
|
$ |
|
|
$ |
|
||
Equity in other comprehensive (loss) income of affiliates, |
|
|
|
|
|
|
|
|
|
|||
Net change in fair value of available-for-sale debt securities, net of tax |
|
|
|
|
|
( |
) |
|
|
( |
) |
|
Amortization and recognition of unrecognized pension cost |
|
|
|
|
|
|
|
|
|
|||
Other comprehensive income (loss) |
|
|
|
|
|
( |
) |
|
|
( |
) |
|
Comprehensive (loss) income |
|
|
( |
) |
|
|
|
|
|
|
||
Less: Comprehensive income attributable to noncontrolling interests |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Comprehensive (loss) income attributable to Community Health Systems, |
|
$ |
( |
) |
|
$ |
|
|
$ |
|
||
|
|
|
|
|
|
|
|
|
|
|||
See note to condensed financial statements of Parent Company. |
|
|
|
|
|
|
|
|
|
|||
Parent Company Only |
|
|
|
|
|
|
|
|
|
|||
Condensed Statements of Cash Flows |
|
|
|
|
|
|
|
|
|
|||
(In millions) |
|
|
|
|
|
|
|
|
|
|||
|
|
Year Ended December 31, |
|
|||||||||
|
|
2023 |
|
|
2022 |
|
|
2021 |
|
|||
Cash flows from operating activities: |
|
|
|
|
|
|
|
|
|
|||
Net cash used in operating activities |
|
$ |
( |
) |
|
$ |
( |
) |
|
$ |
( |
) |
Cash flows from investing activities: |
|
|
|
|
|
|
|
|
|
|||
Net cash provided by (used in) investing activities |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Cash flows from financing activities: |
|
|
|
|
|
|
|
|
|
|||
Repurchase of restricted stock shares for payroll tax withholding |
|
|
( |
) |
|
|
( |
) |
|
|
( |
) |
Changes in intercompany balances with affiliates, net |
|
|
|
|
|
|
|
|
|
|||
Net cash provided by financing activities |
|
|
|
|
|
|
|
|
|
|||
Net change in cash and cash equivalents |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Cash and cash equivalents at beginning of period |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Cash and cash equivalents at end of period |
|
$ |
— |
|
|
$ |
— |
|
|
$ |
— |
|
|
|
|
|
|
|
|
|
|
|
|||
See note to condensed financial statements of Parent Company. |
|
|
|
|
|
|
|
|
|
|||
The Parent Company is a holding company and operates no business in its own name; all of the Company’s business operations are conducted through subsidiaries of the Parent Company. The Company’s outstanding indebtedness restricts the ability of subsidiaries to dividend or otherwise provide funds to the Parent Company. Accordingly, these financial statements have been presented on a “parent-only” basis. Under parent-only presentation, the Parent Company’s investments in its consolidated subsidiaries are presented under the equity method of accounting. These parent-only financial statements should be read in conjunction with consolidated financial statements of Community Health Systems, Inc.
117
Item 9. Changes in and Disagreements with Accountants on Accounting and Financial Disclosure
None.
Item 9A. Controls and Procedures
Evaluation of Disclosure Controls and Procedures
Our Chief Executive Officer and Chief Financial Officer, with the participation of other members of management, have evaluated the effectiveness of our disclosure controls and procedures (as defined in Rules 13a-15(e) and 15d-15(e)) under the Securities and Exchange Act of 1934, as amended, as of the end of the period covered by this report. Based on such evaluations, our Chief Executive Officer and Chief Financial Officer concluded that, as of such date, our disclosure controls and procedures were effective (at the reasonable assurance level) to ensure that the information required to be included in this report has been recorded, processed, summarized and reported within the time periods specified in the SEC’s rules and forms and to ensure that the information required to be included in this report was accumulated and communicated to management, including our Chief Executive Officer and Chief Financial Officer, to allow timely decisions regarding required disclosure.
Changes in Internal Control Over Financial Reporting
As previously disclosed, we have undertaken a multi-year, transformative process of redesigning numerous workflows that is intended to modernize and consolidate our technology platforms and associated processes across our organization. As part of this process, we have created and continue to expand shared business operations to carry out certain financial and operational functions and are implementing a new enterprise resource planning system, or ERP. In connection with these changes, new internal controls have been implemented and certain existing internal controls have been replaced or modified. As the phased implementation of the ERP system continues along with continued expansion of shared business operations, additional changes to internal controls over financial reporting may result and such changes may be material. Other than changes associated with the aforementioned multi-year process that occurred during the three months ended December 31, 2023, there have been no changes in internal control over financial reporting that occurred during this three month period that have materially affected or are reasonably likely to materially affect our internal controls over financial reporting.
Management’s report on internal control over financial reporting is included herein at page 119.
The attestation report from Deloitte & Touche LLP, our independent registered public accounting firm, on our internal control over financial reporting is included herein at page 120.
Item 9B. Other Information
None. Without limiting the generality of the foregoing, during the three months ended December 31, 2023, no director or officer of the Company
Item 9C. Disclosure Regarding Foreign Jurisdictions that Prevent Inspections.
None.
118
Management’s Report on Internal Control over Financial Reporting
We are responsible for the preparation and integrity of the consolidated financial statements appearing in our Annual Report on Form 10-K. The consolidated financial statements were prepared in conformity with accounting principles generally accepted in the United States of America and include amounts based on management’s estimates and judgments. All other financial information in this report has been presented on a basis consistent with the information included in the consolidated financial statements.
We are also responsible for establishing and maintaining adequate internal controls over financial reporting (as defined in Rule 13a-15(f) under the Securities and Exchange Act of 1934, as amended). We maintain a system of internal controls that is designed to provide reasonable assurance as to the fair and reliable preparation and presentation of the consolidated financial statements, as well as to safeguard assets from unauthorized use or disposition.
Our control environment is the foundation for our system of internal control over financial reporting and is embodied in our Code of Conduct. It sets the tone of our organization and includes factors such as integrity and ethical values. Our internal control over financial reporting is supported by formal policies and procedures which are reviewed, modified and improved as changes occur in business conditions and operations.
The Audit and Compliance Committee of the Board of Directors, which is composed solely of outside directors, meets periodically with members of management, the internal auditors and the independent registered public accounting firm to review and discuss internal control over financial reporting and accounting and financial reporting matters. The independent registered public accounting firm and internal auditors report to the Audit and Compliance Committee and have full and free access to the Audit and Compliance Committee at any time.
We conducted an evaluation of the effectiveness of our internal control over financial reporting based on the framework in Internal Control - Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission. This evaluation included review of the documentation of controls, evaluation of the design effectiveness of controls, testing of the operating effectiveness of controls and a conclusion on this evaluation. We have concluded that our internal control over financial reporting was effective as of December 31, 2023, based on these criteria.
Deloitte & Touche LLP, an independent registered public accounting firm, has issued an attestation report on our internal control over financial reporting, which is included herein.
We do not expect that our disclosure controls and procedures or our internal controls will prevent all errors and all fraud. A control system, no matter how well conceived and operated, can provide only reasonable, not absolute, assurance that the objectives of the control system are met. Further, the design of a control system must reflect the fact there are resource constraints and the benefits of controls must be considered relative to their costs. Because of the inherent limitations in all control systems, no evaluation of controls can provide absolute assurance that all control issues and instances of fraud, if any, within the Company have been detected.
119
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Stockholders and the Board of Directors of
Community Health Systems, Inc.,
Franklin, Tennessee
Opinion on Internal Control over Financial Reporting
We have audited the internal control over financial reporting of Community Health Systems, Inc., and subsidiaries (the “Company”) as of December 31, 2023, based on criteria established in Internal Control — Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO). In our opinion, the Company maintained, in all material respects, effective internal control over financial reporting as of December 31, 2023, based on criteria established in Internal Control — Integrated Framework (2013) issued by COSO.
We have also audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the consolidated financial statements as of and for the year ended December 31, 2023, of the Company and our report dated February 21, 2024, expressed an unqualified opinion on those financial statements.
Basis for Opinion
The Company’s management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting, included in the accompanying Management’s report on Internal Control over Financial Reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audit in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects. Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
Definition and Limitations of Internal Control over Financial Reporting
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
/s/ Deloitte & Touche LLP
Nashville, Tennessee
February 21, 2024
120
PART III
Item 10. Directors, Executive Officers and Corporate Governance
The Company has adopted a Code of Conduct that is applicable to all members of the Board of Directors and our officers, as well as employees of our subsidiaries. A copy of the current version of our Code of Conduct is available in the Company-Overview — Corporate Governance section of our internet website at www.chs.net/company-overview/corporate-governance. A copy of the Code of Conduct is also available in print, free of charge, to any stockholder who requests it by writing to Community Health Systems, Inc., Investor Relations, at 4000 Meridian Boulevard, Franklin, TN 37067. The Company intends to post amendments to or waivers, if any, from its Code of Conduct at this location on its website, in each case to the extent such amendment or waiver would otherwise require the filing of a Current Report on Form 8-K pursuant to Item 5.05 thereof.
The committee report of the Audit and Compliance Committee of the Board of Directors is presented below. Information required by Item 10 of Part III is incorporated herein by reference to the Company’s definitive proxy statement to be filed under Regulation 14A in connection with the Annual Meeting of the Stockholders of the Company scheduled to be held on May 10, 2024.
AUDIT AND COMPLIANCE COMMITTEE REPORT
The Audit and Compliance Committee of the Board of Directors of the Company is composed of five directors, each of whom is “independent” as defined by the applicable listing standards of the New York Stock Exchange and Section 10A-3 of the Exchange Act and are financially literate in accordance with New York Stock Exchange listing standards. In addition, four of our five Audit and Compliance Committee members meet the Securities and Exchange Commission definition of “audit committee financial expert.” The Audit and Compliance Committee operates under a written charter adopted by the Board of Directors, which is posted on our corporate website (www.chs.net) and which is reviewed by the Committee annually, in conjunction with the Committee’s annual self-evaluation. The Company’s management is responsible for its internal controls and the financial reporting process. Our independent registered public accounting firm, Deloitte & Touche LLP, is responsible for performing an independent audit of our consolidated financial statements in accordance with the standards of the Public Company Accounting Oversight Board (United States) and to issue its reports thereon. The Audit and Compliance Committee is responsible for, among other things, monitoring and overseeing these processes, and recommending to the Board of Directors: (i) that the audited consolidated financial statements be included in the Company’s Annual Report on Form 10-K; and (ii) the selection of the independent registered public accounting firm to audit the consolidated financial statements of the Company.
In keeping with that responsibility, the Audit and Compliance Committee has reviewed and discussed the Company’s audited consolidated financial statements with management and with the independent registered public accounting firm, reviewed internal controls and accounting procedures and provided oversight review of the Company’s corporate compliance program. In addition, the Audit and Compliance Committee has discussed with the Company’s independent registered public accounting firm the matters required to be discussed by the applicable requirements of the Public Company Accounting Oversight Board.
The Audit and Compliance Committee discussed with the Company’s internal auditors and independent registered public accounting firm the overall scope and plans for their respective audits. The Audit and Compliance Committee met with the internal auditors and the independent registered public accounting firm with and without management present to discuss the results of their examinations, their evaluations of the Company’s internal controls and the overall quality of the Company’s financial reporting.
The Audit and Compliance Committee has received the written disclosures and the letter from the independent registered public accounting firm required by applicable requirements of the Public Company Accounting Oversight Board regarding the independent accountant’s communications with the audit committee concerning independence. The Audit and Compliance Committee has discussed with the independent registered public accounting firm its independence and also has reviewed the amount of fees paid to the independent registered accounting firm for audit and non-audit services.
Based on the Audit and Compliance Committee’s discussions with management and the independent registered public accounting firm and the Audit and Compliance Committee’s review of the representations of management and the materials it received from the independent registered public accounting firm as described above, the Audit and Compliance Committee recommended to the Board of Directors that the audited consolidated financial statements be included in the Company’s Annual Report on Form 10-K for the year ended December 31, 2023 for filing with the SEC.
121
This report is respectfully submitted by the Audit and Compliance Committee of the Board of Directors.
|
THE AUDIT AND COMPLIANCE COMMITTEE |
|
Michael Dinkins, Chair |
|
Ronald L. Burgess, Jr. James S. Ely III |
|
Elizabeth T. Hirsch |
|
H. James Williams, Ph.D. |
Item 11. Executive Compensation
Information required by Item 11 of Part III is incorporated herein by reference to the Company’s definitive proxy statement to be filed under Regulation 14A in connection with the Annual Meeting of the Stockholders of the Company scheduled to be held on May 10, 2024.
Item 12. Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters
Information required by Item 12 of Part III is incorporated herein by reference to the Company’s definitive proxy statement to be filed under Regulation 14A in connection with the Annual Meeting of the Stockholders of the Company scheduled to be held on May 10, 2024.
Information required by Item 13 of Part III is incorporated herein by reference to the Company’s definitive proxy statement to be filed under Regulation 14A in connection with the Annual Meeting of the Stockholders of the Company scheduled to be held on May 10, 2024.
Item 14. Principal Accounting Fees and Services
Information required by Item 14 of Part III is incorporated herein by reference to the Company’s definitive proxy statement to be filed under Regulation 14A in connection with the Annual Meeting of the Stockholders of the Company scheduled to be held on May 10, 2024.
122
PART IV
Item 15. Exhibits and Financial Statement Schedules
Item 15(a) 1. Financial Statements
Reference is made to the index of financial statements and supplementary data under Item 8 in Part II.
Item 15(a) 2. Financial Statement Schedules
The following financial statement schedule is included within the notes to the consolidated financial statements at page 115 hereof:
Schedule I – Condensed Financial Information of Registrant
All other schedules are omitted since the required information is not present or is not present in amounts sufficient to require submission of the schedule.
123
Item 15(a) 3. Exhibits
The following exhibits are either filed with this Report or incorporated herein by reference.
No. |
|
Description |
|
|
|
2.1 |
|
|
|
|
|
2.2 |
|
|
|
|
|
2.3 |
|
|
|
|
|
2.4 |
|
|
|
|
|
2.5 |
|
|
|
|
|
2.6 |
|
|
|
|
|
2.7* |
|
|
|
|
|
2.8 |
|
|
|
|
|
3.1 |
|
|
|
|
|
3.2 |
|
|
|
|
|
3.3 |
|
|
|
|
|
4.1 |
|
|
|
|
|
4.2 |
|
|
|
|
|
4.3 |
|
Form of 8.000% Senior Secured Note due 2026 (included in Exhibit 4.2) |
|
|
|
124
No. |
|
Description |
|
|
|
4.4 |
|
|
|
|
|
4.5 |
|
|
|
|
|
4.6 |
|
|
|
|
|
4.7 |
|
|
|
|
|
4.8 |
|
|
|
|
|
4.9 |
|
|
|
|
|
4.10* |
|
|
|
|
|
4.11 |
|
|
|
|
|
4.12 |
|
Form of 8.000% Senior Secured Note due 2027 (included in Exhibit 4.11) |
|
|
|
4.13 |
|
|
|
|
|
4.14 |
|
|
|
|
|
125
No. |
|
Description |
|
|
|
4.15* |
|
|
|
|
|
4.16 |
|
|
|
|
|
4.17 |
|
Form of 6.875% Senior Unsecured Note due 2028 (included in Exhibit 4.16) |
|
|
|
4.18 |
|
|
|
|
|
4.19 |
|
|
|
|
|
4.20* |
|
|
|
|
|
4.21 |
|
|
|
|
|
4.22 |
|
Form of 5.625% Senior Secured Note due 2027 (included in Exhibit 4.21) |
|
|
|
4.23* |
|
|
|
|
|
4.24 |
|
|
|
|
|
4.25 |
|
Form of 6.000% Senior Secured Note due 2029 (included in Exhibit 4.24) |
|
|
|
4.26* |
|
|
|
|
|
4.27 |
|
|
|
|
|
4.28 |
|
Form of 6.875% Junior-Priority Secured Note due 2029 (included in Exhibit 4.27) |
|
|
|
4.29* |
|
|
|
|
|
4.30 |
|
126
No. |
|
Description |
|
|
|
|
|
|
|
|
|
4.31 |
|
Form of 4.750% Senior Secured Note due 2031 (included in Exhibit 4.30) |
|
|
|
4.32* |
|
|
|
|
|
4.33 |
|
|
|
|
|
4.34 |
|
Form of 6.125% Junior-Priority Secured Note due 2030 (included in Exhibit 4.33) |
|
|
|
4.35* |
|
|
|
|
|
4.36 |
|
|
|
|
|
4.37 |
|
Form of 5.250% Senior Secured Note due 2030 (included in Exhibit 4.36) |
|
|
|
4.38* |
|
|
|
|
|
4.39 |
|
|
|
|
|
4.40 |
|
Form of 10.875% Senior Secured Note due 2032 (included in Exhibit 4.39) |
|
|
|
4.41 |
|
|
|
|
|
4.42 |
|
|
|
|
|
4.43 |
|
|
|
|
|
4.44 |
|
127
No. |
|
Description |
|
|
|
|
|
|
|
|
|
4.45 |
|
|
|
|
|
10.1 |
|
|
|
|
|
10.2 |
|
|
|
|
|
10.3 |
|
|
|
|
|
10.4† |
|
|
|
|
|
10.5† |
|
|
|
|
|
10.6† |
|
|
|
|
|
10.7† |
|
|
|
|
|
10.8† |
|
|
|
|
|
10.9† |
|
|
|
|
|
10.10† |
|
|
|
|
|
10.11† |
|
|
|
|
|
128
No. |
|
Description |
|
|
|
10.12† |
|
|
|
|
|
10.13† |
|
|
|
|
|
10.14† |
|
|
|
|
|
10.15† |
|
|
|
|
|
10.16† |
|
|
|
|
|
10.17† |
|
|
|
|
|
10.18† |
|
|
|
|
|
10.19† |
|
|
|
|
|
10.20† |
|
|
|
|
|
10.21† |
|
|
|
|
|
10.22† |
|
|
|
|
|
10.23† |
|
|
|
|
|
10.24† |
|
|
|
|
|
10.25† |
|
|
|
|
|
10.26 |
|
129
No. |
|
Description |
|
|
|
|
|
|
10.27 |
|
|
|
|
|
21* |
|
|
|
|
|
23.1* |
|
|
|
|
|
31.1* |
|
Certification of Chief Executive Officer pursuant to Section 302 of the Sarbanes-Oxley Act of 2002 |
|
|
|
31.2* |
|
Certification of Chief Financial Officer pursuant to Section 302 of the Sarbanes-Oxley Act of 2002 |
|
|
|
32.1** |
|
|
|
|
|
32.2** |
|
|
|
|
|
97†* |
|
Community Health Systems, Inc. Amended and Restated Clawback Policy, dated September 13, 2023 |
|
|
|
99.1 |
|
|
|
|
|
101* |
|
The following financial information from our annual report on Form 10-K for the year ended December 31, 2023, filed with the SEC on February 21, 2024, formatted in Inline Extensible Business Reporting Language: (i) the consolidated statements of (loss) income for the years ended December 31, 2023, 2022 and 2021, (ii) the consolidated statements of comprehensive (loss) income for the years ended December 31, 2023, 2022 and 2021, (iii) the consolidated balance sheets at December 31, 2023 and December 31, 2022, (iv) the consolidated statements of stockholders’ deficit for the years ended December 31, 2023, 2022 and 2021, (v) the consolidated statements of cash flows for the years ended December 31, 2023, 2022 and 2021, and (vi) the notes to the consolidated financial statements. The instance document does not appear in the Interactive Data File because its XBRL tags are embedded within the Inline XBRL document. |
|
|
|
104* |
|
Cover Page Interactive Data File (formatted as Inline XBRL and contained in Exhibit 101) |
|
|
|
* Filed herewith.
** Furnished herewith.
† Indicates a management contract or compensatory plan or arrangement.
Item 16. Form 10-K Summary
None.
130
SIGNATURES
Pursuant to the requirements of section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
|
|
Community Health Systems, Inc. |
|
|
|
|
By: |
/s/ Tim L. Hingtgen |
|
|
Tim L. Hingtgen |
|
|
Director and |
|
|
|
|
Date: |
February 21, 2024 |
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the Registrant and in the capacities and on the dates indicated.
Name |
Title |
Date |
/s/ Tim L. Hingtgen |
Director and |
February 21, 2024 |
Tim L. Hingtgen |
Chief Executive Officer |
|
|
|
|
/s/ Kevin J. Hammons |
President and |
February 21, 2024 |
Kevin J. Hammons |
Chief Financial Officer |
|
|
|
|
/s/ Jason K. Johnson |
Senior Vice President and |
February 21, 2024 |
Jason K. Johnson |
Chief Accounting Officer |
|
|
|
|
/s/ Wayne T. Smith |
Chairman of the |
February 21, 2024 |
Wayne T. Smith |
Board of Directors |
|
|
|
|
/s/ Susan W. Brooks |
Director |
February 21, 2024 |
Susan W. Brooks |
|
|
|
|
|
/s/ Ronald L. Burgess, Jr. |
Director |
February 21, 2024 |
Ronald L. Burgess, Jr. |
|
|
|
|
|
/s/ John A. Clerico |
Director |
February 21, 2024 |
John A. Clerico |
|
|
|
|
|
/s/ Michael Dinkins |
Director |
February 21, 2024 |
Michael Dinkins |
|
|
|
|
|
/s/ James S. Ely III |
Director |
February 21, 2024 |
James S. Ely III |
|
|
|
|
|
/s/ John A. Fry |
Director |
February 21, 2024 |
John A. Fry |
|
|
|
|
|
/s/ Joseph A. Hastings, D.M.D |
Director |
February 21, 2024 |
Joseph A. Hastings, D.M.D |
|
|
|
|
|
/s/ Elizabeth T. Hirsch |
Director |
February 21, 2024 |
Elizabeth T. Hirsch |
|
|
|
|
|
/s/ William Norris Jennings, M.D. |
Director |
February 21, 2024 |
William Norris Jennings, M.D. |
|
|
|
|
|
/s/ K. Ranga Krishnan, MBBS |
Director |
February 21, 2024 |
K. Ranga Krishnan, MBBS |
|
|
|
|
|
/s/ H. James Williams, Ph.D. |
Director |
February 21, 2024 |
H. James Williams, Ph.D. |
|
|
131